
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Celiac disease (gluten enteropathy)
Medical expert of the article
Last reviewed: 12.07.2025
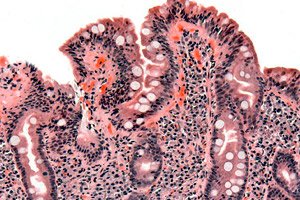
Celiac disease (non-tropical sprue, gluten enteropathy, celiac disease) is an immunologically mediated gastrointestinal disease in genetically susceptible individuals, characterized by intolerance to gluten, inflammation of the mucous membrane, and malabsorption. Symptoms of celiac disease typically include diarrhea and abdominal discomfort. Diagnosis is by small intestinal biopsy, which shows some non-specific changes, including pathological villous atrophy, with improvement occurring with a strict gluten-free diet.
Synonyms for the term "gluten or gluten-sensitive enteropathy" are celiac sprue, celiac disease, adult celiac disease, idiopathic steatorrhea, non-tropical sprue. A number of authors consider the term "celiac sprue" to be more appropriate. Many emphasize that the definition of "gluten enteropathy" is alternative.
What causes celiac disease?
Celiac disease is an inherited disorder caused by hypersensitivity to the gliadin fraction of gluten, a protein found in wheat; similar proteins are found in rye and barley. In genetically susceptible individuals, gluten-sensitive T cells become activated when gluten-derived protein determinants are presented. The inflammatory response results in characteristic villous atrophy of the small intestinal mucosa.
The prevalence of the disease varies from about 1/150 in southwestern Ireland to 1/5000 in North America. Celiac disease occurs in approximately 10-20% of first-degree relatives. The female to male ratio is 2:1. The disease most often appears in childhood, but can develop later.
Symptoms of Celiac Disease
There are no specific symptoms of celiac disease. Some patients are asymptomatic or have only symptoms of nutritional deficiency. Others may have significant gastrointestinal symptoms.
In infancy and childhood, celiac disease may manifest itself after adding cereals to the diet. The child has developmental disorders, apathy, anorexia, pallor, general hypotonia, abdominal distension, and muscle wasting. The stool is usually soft, abundant, clay-colored, with an unpleasant odor. In older children, anemia and growth disorders are usually observed.
In adults, the most common symptoms of celiac disease are fatigue, weakness, and anorexia. Mild and intermittent diarrhea is sometimes the main symptom. Steatorrhea is moderate to severe (7-50 g fat/day). Some patients experience weight loss, but it is rare for the weight to be below normal. These patients typically present with anemia, glossitis, angular stomatitis, and aphthous ulcers. Vitamin D and calcium deficiencies (eg, osteomalacia, bone formation disorders, osteoporosis) are common. In both men and women, fertility may be reduced.
Approximately 10% have dermatitis herpetiformis, a severe papulo-vesicular rash with itching that symmetrically affects the extensor surfaces of the elbow and knee joints, buttocks, shoulders, and scalp. The rash may be caused by eating foods high in gluten. The development of celiac disease is also associated with diabetes mellitus, autoimmune thyroid diseases, and Down syndrome.
What's bothering you?
Diagnosis of celiac disease
The diagnosis is suspected when clinical and laboratory changes suggest malabsorption. Family history is an important element in the diagnosis. Celiac disease is suspected in patients with iron deficiency without obvious gastrointestinal bleeding.
Confirmation of the diagnosis requires a small bowel biopsy from the descending duodenum. Morphologic findings include a lack or reduction of villi (villous atrophy), enlarged intraepithelial cells, and crypt hyperplasia. However, such findings may also be seen in tropical sprue, severe intestinal bacterial overgrowth, eosinophilic enteritis, lactose intolerance, and lymphoma.
Since biopsy does not reveal specific changes, serologic markers may help in establishing the diagnosis. The detection of a combination of antigliadin (AGAb) and antiendomysial antibodies (AEAb - an antibody against intestinal connective tissue protein) has a positive and negative predictive value of almost 100%. These markers can also be used for screening populations with a high prevalence of celiac sprue, including first-generation relatives of affected patients and patients with diseases that are frequently associated with celiac sprue. In case of any positive test, the patient should undergo a diagnostic small intestinal biopsy. If both tests are negative, celiac disease is unlikely. The titer of these antibodies decreases with adherence to a gluten-free diet, and therefore these tests are useful in monitoring dietary compliance.
Other laboratory abnormalities are often seen and should be investigated. These include anemia (iron deficiency anemia in children and folate deficiency anemia in adults); decreased albumin, calcium, potassium, and sodium levels; and increased alkaline phosphatase and prothrombin time.
Malabsorption tests are not specific for celiac disease. However, if tests are performed, the results show steatorrhea of up to 10-40 g/day, abnormal D-xylose test and (in severe ileal disease) Schilling test.
What do need to examine?
What tests are needed?
Celiac disease treatment
Treatment of celiac disease involves a gluten-free diet (avoiding foods containing wheat, rye, or barley). Gluten is widely used in foods (e.g., ready-made soups, sauces, ice cream, hot dogs), so patients need a detailed description of the composition of foods to avoid gluten. The patient needs to consult a dietitian and join a support group for patients with celiac disease. The result after the introduction of a gluten-free diet is rapid and resolution of symptoms occurs within 1-2 weeks. Ingestion of even small amounts of food containing gluten can lead to an exacerbation or cause a relapse.
Small bowel biopsy should be repeated 3-4 months after the gluten-free diet. If changes persist, other causes of villous atrophy (eg, lymphoma) should be considered. The disappearance of celiac disease symptoms and improvement of small bowel morphology are accompanied by a decrease in AGAT and AEAt titers.
Depending on the deficiency, vitamins, minerals, and hemoglobin-boosting drugs should be prescribed. Mild cases do not require additional drugs, but severe cases require comprehensive therapy. In adults, additional treatment includes iron sulfate 300 mg orally one to three times a day, folate 5-10 mg orally once a day, calcium supplements, and any standard multivitamin complex. Sometimes, in severe cases of the disease in children and its initial detection (rarely in adults), it is necessary to exclude food intake and parenteral nutrition.
If there is no effect from a gluten-free diet, one should think about an erroneous diagnosis or the development of a refractory stage of the course of celiac disease. In the latter case, the administration of glucocorticoids may be effective.
What is the prognosis for celiac disease?
Celiac disease is fatal in 10-30% of cases without dietary compliance. With dietary compliance, mortality is less than 1%, mainly in adults who initially had a severe course of the disease. Complications of celiac disease include refractory sprue, collagenous sprue, and the development of intestinal lymphomas. Intestinal lymphomas occur in 6-8% of patients with celiac disease, usually in patients over 50 years of age. The risk of malignant growth of other parts of the gastrointestinal tract (e.g., carcinoma of the esophagus or oropharynx, adenocarcinoma of the small intestine) increases. Adherence to a gluten-free diet can significantly reduce the risk of malignancy.


 [
[