
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Hemorrhagic cystitis
Medical expert of the article
Last reviewed: 04.07.2025
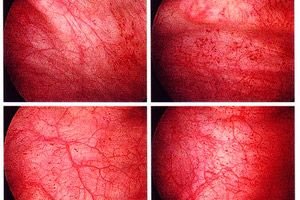
What is the difference between hemorrhagic cystitis and common bladder inflammation? The main difference is hematuria – the appearance of blood in the urine during urination. And this indicates a significant depth of damage to the multilayered epithelium (urothelium) of the mucous membrane of the inner walls of the bladder, as well as the spread of the destructive process to the endothelium of the capillaries of its microcirculatory bed.
Epidemiology
Bladder and urinary tract infections affect approximately 150 million people each year.
According to research, infectious hemorrhagic cystitis occurs much more often in women than in men. Especially in women during menopause, since the protective properties of the vaginal flora are reduced due to a decrease in estrogen levels.
In two thirds of cases, hemorrhagic cystitis in newborns is associated with the presence of untreated urogenital infections in the mother.
Hemorrhagic cystitis also develops in almost 6% of patients who have undergone bone marrow transplantation and receive high doses of Cyclophosphamide or Ifosfamide.
Causes hemorrhagic cystitis
Today, the causes of hemorrhagic cystitis, which determine its types, are divided into infectious and non-infectious.
In most cases, bacterial acute hemorrhagic cystitis occurs due to infection of the bladder with uropathogenic strains of Escherichia coli (UPEC), Proteus vulgaris, opportunistic bacteria Klebsiella oxytoca and saprophytic staphylococcus (Staphylococcus saprophyticus).
The pathogenesis of UPEC lesions is associated with the ability of Escherichia coli (representing synanthropic intestinal flora, but found in the urinary tract) to act as opportunistic intracellular pathogens. Using adhesive organelles, the bacteria penetrate into cells and colonize the mucosa of the urethra and bladder; here they feed on iron compounds extracted from cells and produce toxins - hemolysin, which destroys erythrocytes, and cytotoxic necrotizing factor 1 (CNF1), which catalyzes receptor-mediated endocytosis, which causes a response of urothelial effector cells and inflammatory reactions.
Infectious hemorrhagic cystitis in women is often provoked by ureaplasma, mycoplasma, chlamydia, gardnerella, gonococci, trichomonas. But primary fungal cystitis is rare and, as a rule, is associated with the treatment of bacterial cystitis: suppression of commensal vaginal microflora with antibiotics allows Candida fungi and lactobacilli to reproduce unhindered.
Against the background of inflammation of the prostate gland, hemorrhagic cystitis may develop in older men. It is often provoked by unsuccessful catheterization of the bladder and subsequent infection.
Viral hemorrhagic cystitis in children, as well as hemorrhagic cystitis in newborns, is most often associated with adenovirus - serotypes 11 and 21 subgroup B. Although this disease can be the result of activation of the latent polyomavirus BK (Human polyomavirus 1). According to the latest edition of Virus Taxonomy, the BK virus infects most people, and in childhood it initiates respiratory diseases and acute cystitis. By the way, this virus persists in a latent form throughout life (in the tissues of the genitourinary organs and pharyngeal tonsils).
Reactivation of the "dormant" polyomavirus BK occurs due to one or another form of immunosuppression: in old age, with congenital immunodeficiency in children, acquired immunodeficiency syndrome (AIDS) in adults, in women - during pregnancy, which can be associated with hemorrhagic cystitis during pregnancy. The virus is also activated during bone marrow and allogeneic stem cell transplantation, when drugs are used to suppress the immune system. Studies have shown that after bone marrow transplantation, virally induced hemorrhagic cystitis in children and adolescents is the most common complication.
Non-infectious causes of hemorrhagic cystitis
According to urologists, chronic hemorrhagic cystitis of nonbacterial etiology can develop due to the presence of stones in the bladder - especially urate stones in uric acid diathesis - when the bladder mucosa is injured, and the damage becomes deeper under the influence of excessively acidic urine. Many domestic specialists call this hemorrhagic cystitis ulcerative.
Also not associated with infection are such types of hemorrhagic cystitis as radiation (radiation) or chemically induced cystitis. Radiation hemorrhagic inflammation of the bladder mucosa develops after treatment of malignant neoplasms localized in the small pelvis. In this case, the pathogenesis is due to the fact that radiation causes breaks in DNA chains, leading to the activation of genes for DNA damage repair and apoptosis. In addition, radiation penetrates into the deeper layers of the bladder muscles, which reduces the impermeability of the vessel walls.
Chemically induced hemorrhagic cystitis is the result of intravenous administration of anticancer cytostatic drugs, in particular, Ifosfamide (Holoxan), Cyclophosphamide (Cytoforsfan, Endoxan, Claphen, etc.) and, to a lesser extent, Bleomycin and Doxorubicin.
Thus, the metabolism of Cyclophosphamide in the liver leads to the formation of acrolein, which is a toxin and destroys the tissues of the bladder wall. Severe inflammation of the bladder, which occurs as a complication of chemotherapy for cancer patients, is called refractory (difficult to cure) hemorrhagic cystitis.
Hemorrhagic cystitis in women – in particular chemical – can develop when intravaginal agents enter the bladder through the urethra. This happens when douching the vagina with the antiseptic methyl violet (gentian violet) to treat vaginal candidiasis or spermicidal agents, such as Nonoxynol.
Risk factors
The main risk factors for the development of hemorrhagic cystitis are associated with a decrease in the body's immune defense; the presence of latent urogenital infections and oncological diseases; urinary stasis and urolithiasis; thrombocytopenia (low platelet levels in the blood); poor hygiene of the genitourinary organs and failure to comply with aseptic standards during gynecological and urological manipulations.
The risk of urinary tract and bladder infection in children is associated with vesicoureteral reflux (abnormal movement of urine) and constipation.
Symptoms hemorrhagic cystitis
Usually, the first signs of hemorrhagic cystitis are manifested by pollakiuria - more frequent urination with a simultaneous decrease in the volume of urine excreted. Almost simultaneously, such a characteristic sign of the initial stage of inflammation as multiple false urges to empty the bladder (including at night) as well as burning and acute pain at the end of urination are added.
In addition, the following clinical symptoms of hemorrhagic cystitis are noted: discomfort in the pubic area; pain in the pelvis radiating to the lower back and groin; cloudiness of excreted urine, change in its color (from pink to all shades of red) and smell. Often, control of the bladder is lost (there may be urinary incontinence).
General well-being worsens - with weakness, loss of appetite, increased temperature and fever.
If at a certain stage of the disease the patient experiences difficulty urinating, this indicates that the outlet of the bladder is blocked by blood clots (tamponade).
Where does it hurt?
What's bothering you?
Complications and consequences
The main consequences and complications of hemorrhagic cystitis of any etiology include:
- obstruction of urine outflow (due to the above-mentioned tamponade by a blood clot) can lead to urosepsis, rupture of the bladder and renal failure;
- disruption of the integrity of the vessels of the microcirculatory bed of the bladder threatens blood loss and the development of iron deficiency anemia, especially if patients have chronic hemorrhagic cystitis;
- damaged areas of the urothelium can become “entry points” for infections and ensure the entry of bacteria into the systemic bloodstream;
- Open ulcers on the internal surfaces of the bladder often lead to permanent scarring of its lining and sclerotic changes in the walls - with a decrease in size and deformation of the shape of the bladder.
Diagnostics hemorrhagic cystitis
Diagnosis of hemorrhagic cystitis is carried out by urologists, but the participation of gynecologists may be required when hemorrhagic cystitis occurs in women.
The following tests are required:
- general urine analysis;
- microbiological analysis of urine (using PCR sequencing of urine – to identify the type of infectious agent and its resistance to antibacterial drugs);
- clinical blood test;
- blood test for STDs;
- vaginal and cervical smear (for women);
- urethral smear (for men);
Instrumental diagnostics are used: ultrasound of the bladder and all pelvic organs, cystoscopy, urethroscopy.
To clarify the functional state of the muscular layer of the bladder in chronic hemorrhagic cystitis, specialists can examine urodynamics using uroflowmetry or electromyography of the bladder.
What do need to examine?
What tests are needed?
Differential diagnosis
Differential diagnostics aims to distinguish hemorrhagic cystitis from hematuria, which may accompany inflammation of the urethra (urethritis); tumors of the bladder or urinary tract; prostate adenoma (in men) or endometriosis (in women); pyelonephritis, focal proliferative glomerulonephritis, polycystic kidney disease, etc.
Who to contact?
Treatment hemorrhagic cystitis
Complex treatment of hemorrhagic cystitis is aimed at the causes of the disease, as well as at alleviating its symptoms.
If the disease is of bacterial origin, antibiotics are necessarily prescribed for hemorrhagic cystitis. The most active are fluoroquinolones, for example, Norfloxacin (other trade names: Nolitsin, Baktinor, Norbactin, Normax, Urobacil) and Ciprofloxacin (Ciprobay, Ciplox, Ciprinol, Ciproxin, Ciprolet, etc.).
Norfloxacin (400 mg tablets) is recommended to be taken one tablet twice a day for one to two weeks. The drug can cause nausea, loss of appetite, diarrhea, and general weakness. Norfloxacin is contraindicated in cases of kidney problems, epilepsy, children under 15, and pregnant women.
The bactericidal action of Ciprofloxacin (in tablets of 0.25-0.5 g and in the form of an infusion solution) is stronger. The recommended dosage is 0.25-0.5 g twice a day (in severe cases, the drug is administered parenterally). Ciprofloxacin has similar contraindications, and its side effects include skin allergies, abdominal pain, dyspepsia, a decrease in leukocytes and blood platelets, and increased sensitivity of the skin to UV rays.
Fosfomycin antibiotic containing fosfomycin trometamol and its synonyms Fosforal, Fosmitsin, Urofoscin, Urofosfabol, Ecofomural or Monural are also effective in hemorrhagic cystitis due to their predominant concentration in kidney tissue. The drug is prescribed at 300 mg once a day (granules are dissolved in 100 ml of water) - two hours before meals. Fosfomycin can be used for children after five years: one dose of 200 mg. Side effects can be in the form of urticaria, heartburn, nausea and diarrhea.
See also - Cystitis Tablets
The most important component of the treatment of hemorrhagic cystitis is the removal of the blood clot from the bladder. It is removed by inserting a catheter into the bladder and continuous instillation (irrigation) of the bladder cavity with sterile water or saline (urologists note that water is preferable to sodium chloride solution, as it dissolves clots better).
If hematuria persists after clot removal, irrigation can be performed with Carboprost or silver nitrate solution. In severe cases, 3-4% formalin solution (which is instilled under anesthesia and cystoscopic control) can be used intravesically, followed by thorough irrigation of the bladder cavity.
For the treatment of hemorrhagic cystitis, hemostatic drugs are used: aminocaproic and tranexamilic acid, Dicynone (orally), Etamsylate (parenterally). Vitamins are necessarily prescribed - ascorbic acid (C) and phylloquinone (K).
An acceptable physiotherapeutic treatment for radiation hemorrhagic cystitis is hyperbaric oxygenation (oxygen therapy), which stimulates cellular immunity, activates angiogenesis and regeneration of tissues lining the bladder; causes vasoconstriction and helps reduce bleeding.
Surgical treatment
When it is not possible to instill the bladder cavity with a catheter, endoscopic removal of the blood clot (cystoscopy) is used - under anesthesia, followed by the use of antibiotics. At the same time, cauterization of hemorrhagic areas (electrocoagulation or argon coagulation) can be performed - to stop bleeding.
Surgical treatment is most often required for refractory hemorrhagic cystitis. In addition to cystoscopy with electrocoagulation, selective embolization of the hypogastric branch of the artery is possible. In extreme cases (with extensive scarring of the bladder walls and its deformation), cystectomy (removal of the bladder) is indicated with urine drainage through the ileum (near the ileocecal valve), the sigmoid colon, or by percutaneous ureterostomy.
According to experts, cystectomy carries a significant risk of postoperative complications and mortality, since patients have already undergone radiation or chemotherapy.
Folk remedies
Limited folk treatment of hemorrhagic cystitis (which in most cases requires hospitalization) applies to the bacterial form of this disease.
This is a treatment with herbs that promote diuresis and relieve inflammation. It is recommended to take decoctions of diuretic medicinal plants: three-part Bidens, field horsetail, meadowsweet, field restharrow, red clover, creeping wheatgrass, stinging nettle, bearberry, corn silk. Decoctions are prepared at the rate of one and a half tablespoons of dry grass per 500 ml of water (boil for 10-12 minutes); the decoction is taken 100 ml 3-4 times a day.
Among the anti-inflammatory medicinal plants in urology, the most commonly used are juniper berries, bearberry, lingonberry leaf and white deadnettle. You can mix all the plants in equal proportions and brew a tablespoon of the mixture with three glasses of boiling water to make a medicinal herbal tea. It is recommended to take 200 ml three times a day for 8-10 days.
Diet for hemorrhagic cystitis - see the publication Diet for cystitis
More information of the treatment
Prevention
Prevention of urogenital infections and timely detection and treatment of latent urogenital infections, strengthening the immune system and avoiding bad habits will help protect against hemorrhagic cystitis, but do not guarantee 100% protection and will not protect against diseases of non-infectious origin.
It is possible to prevent the development of hemorrhagic cystitis during cancer chemotherapy by using Mesna before the start of treatment. However, Mesna will not overcome refractory hemorrhagic cystitis that has already begun. The toxicity of the antitumor drugs listed in the article can also be minimized by the simultaneous use of Amifostine (Etiol).
Forecast
The prognosis for the outcome of bladder inflammation accompanied by hematuria depends on its cause, correct diagnosis, adequate treatment and the general condition of the body.
 [ 44 ]
[ 44 ]

