All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Urogenital chlamydia.
Medical expert of the article
Last reviewed: 04.07.2025
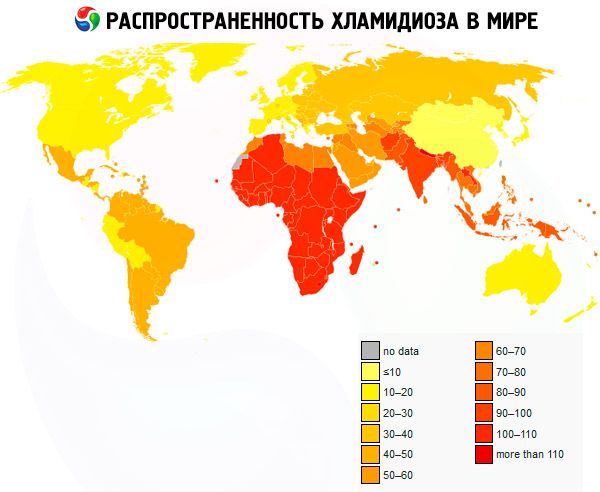
Urogenital chlamydia is one of the most common diseases among sexually transmitted infections.
Chlamydia is a common disease in Europe. Currently, at least 50% of sexually active young women are infected with chlamydia. The mechanism of transmission of the infection is usually sexual.
Causes urogenital chlamydia
Chlamydia belongs to a separate group of microorganisms of eubacterial nature. They can infect a wide range of hosts and cause various diseases. Microorganisms are united in a single genus Chlamydia, belonging to a single family Chlamydiaceae, included in the order Chlamydiales. Three types of chlamydia are known - C. pneumoniae, C. psittaci, C. trachomatis.
Pathogens
Symptoms urogenital chlamydia
Women:
- often asymptomatic;
- discharge from the genital tract;
- dysuria (if other urinary tract infections are excluded);
- pain in the lower abdomen;
- irregular bleeding from the genital tract;
- dyspareunia.
Men:
- discharge from the urethra;
- dysuria;
- itching when urinating;
- pain in the epididymis.
Children:
- conjunctivitis in newborns;
- pneumonia in children during the first 6 months of life.
Chlamydial cervicitis is the most common primary manifestation of chlamydial urogenital infection in women. The disease is often asymptomatic. Sometimes patients complain of minor discharge from the genitals, and vaginal itching, dysuria, and bleeding in the intermenstrual period may also be observed. Chlamydial cervicitis is characterized by yellow, mucopurulent discharge from the cervical canal. Chlamydia can affect the uterine appendages and pelvic peritoneum, resulting in the development of inflammatory diseases of the pelvic organs.
Pregnant women often experience changes in the course of the disease. When chlamydia affects the tubes and endometrium, the process of implantation of the fertilized egg and formation of the placenta is disrupted, which contributes to the development of secondary placental insufficiency. Chlamydia can affect the placenta and membranes, causing the formation of pathogenic immune complexes, which significantly disrupts the function of the placenta as an organ that provides the fetus with adequate nutrition during breathing. In such cases, signs of exhaustion of compensatory-adaptive reactions, involutional-dystrophic processes, dissociation of the development of stromal elements and villi, excessive fibrinoid deposition and lymphocytic infiltration are found in the placenta. Morphofunctional changes in the placenta lead to placental insufficiency, which in turn leads to delayed development and fetal hypotrophy. The risk of placental damage is highest when a woman is infected during pregnancy. In cases where pregnancy occurs against the background of chronic chlamydial infection, the presence of antichlamydial antibodies in a woman prevents the spread of the infectious process.
Where does it hurt?
What's bothering you?
Forms
Women:
- cervicitis;
- VZOMT;
- urethritis;
- perihepatitis.
Men:
- urethritis;
- epididymitis.
Men and women:
- proctitis;
- conjunctivitis;
- Reiter's syndrome;
- lymphogranuloma venereum.
Children:
- urethritis;
- vulvovaginitis;
- proctitis;
- conjunctivitis;
- lymphogranuloma venereum.
Newborns and infants:
- conjunctivitis in newborns;
- pneumonia in children in the first 6 months of life.
Complications and consequences
Diagnostics urogenital chlamydia
Laboratory diagnostic methods:
- Direct immunofluorescence (DIF) is a relatively simple method and is available to almost any laboratory. The sensitivity and specificity of the method depend on the quality of the luminescent antibodies used. Due to the possibility of obtaining false positive results, the DIF method cannot be used in forensic examination. In addition, this method is not recommended for the study of materials obtained from the nasopharynx and rectum.
- The cultural method - cell culture sowing, is considered a priority for laboratory diagnostics of chlamydial infection, especially for forensic medical examination, it is more specific than PIF, irreplaceable in determining the cure of chlamydia, since other methods can give distorted results. However, the sensitivity of the method remains low (within 40-60%).
- Enzyme-linked immunosorbent assay (ELISA) for antigen detection is rarely used for diagnostics due to its low sensitivity.
- Nucleic acid amplification methods (NAAT) are considered highly specific and sensitive and can be used for screening, especially for the study of clinical materials obtained non-invasively (urine, ejaculate). The specificity of the methods is 100%, the sensitivity is 98%. These methods do not require the viability of the pathogen, but it is necessary to comply with strict requirements for the conditions of transportation of the clinical material, which can significantly affect the result of the analysis. These methods include PCR and real-time PCR. The new and promising NASBA (Nucleic Acid Based-Amplification) method in real time allows you to determine the viable pathogen and replace the culture method.
- Serological methods (microimmunofluorescence, immunoenzyme) have limited diagnostic value and cannot be used to diagnose urogenital chlamydial infection, much less to monitor recovery. Detection of IgM AT can be used to diagnose pneumonia in newborns and children in the first 3 months of life. When examining women with PID, infertility, detection of a 4-fold increase in the IgG AT titer when examining paired blood sera is diagnostically significant. An increase in the level of IgG AT to chlamydia (to the serotype of venereous lymphogranuloma) is considered the basis for examining the patient in order to exclude venereous lymphogranuloma.
Conducting a test to determine the sensitivity of chlamydia to antibiotics is not advisable. Taking clinical samples is carried out:
- in women, samples are taken from the cervical canal (diagnostic methods: culture, PIF, PCR, ELISA) and/or the urethra (culture method, PIF, PCR, ELISA) and/or the vagina (PCR);
- in men, samples are taken from the urethra (culture method, PIF, PCR, ELISA) or the first portion of urine is examined (PCR, LCR). The patient must refrain from urinating for 2 hours before taking the sample;
- In infected newborns, samples are taken from the conjunctiva of the lower eyelid and from the nasopharynx; vulvar discharge is also examined in girls.
The technique for taking material depends on the methods used.
Currently, the following terminology is used for diagnosis: fresh (uncomplicated chlamydia of the lower genitourinary tract) and chronic (long-term, persistent, recurrent chlamydia of the upper genitourinary tract, including the pelvic organs). Next, the topical diagnosis should be indicated, including extragenital localization. Chlamydial infection manifests itself after an incubation period, the duration of which ranges from 5 to 40 days (on average 21 days).
If complications develop, consultation with related specialists is required.
The doctor's procedure when a diagnosis of chlamydial infection is established
- Informing the patient about the diagnosis.
- Providing information on behavior during treatment.
- Collection of sexual anamnesis.
- Detection and examination of sexual contacts is carried out depending on the clinical manifestations of the disease and the expected period of infection - from 15 days to 6 months.
- If chlamydia is detected in a woman in labor, a woman who has given birth, or a pregnant woman who has not received timely treatment, the newborn is examined by taking material from the conjunctival sacs of both eyes. If chlamydial infection is detected in a newborn, his parents are examined.
- In the presence of chlamydial infection of the genitals, rectum and pharynx in children in the postnatal period, sexual abuse should be suspected. It should be borne in mind that perinatally acquired C. trachomatis can persist in a child up to 3 years of age. Siblings of an infected child should also be examined. The fact of sexual abuse should be reported to law enforcement agencies.
- Conducting epidemiological measures among contact persons (sanitization of the epidemiological focus) is carried out jointly with the district epidemiologist:
- examination and screening of contact persons;
- laboratory data statement;
- deciding on the need for treatment, its scope and observation period.
- If the contact persons live in other territories, a work order is sent to the territorial KVU.
- If there are no results from treatment, it is recommended to consider the following possible reasons:
- false positive test result;
- non-compliance with treatment regimen, inadequate therapy;
- repeated contact with an untreated partner;
- infection from a new partner;
- infection with other microorganisms.
 [ 32 ], [ 33 ], [ 34 ], [ 35 ], [ 36 ], [ 37 ]
[ 32 ], [ 33 ], [ 34 ], [ 35 ], [ 36 ], [ 37 ]
Patient education
Patient education should be aimed at preventing the spread of infection.
What do need to examine?
Who to contact?
Treatment urogenital chlamydia
Urogenital chlamydia can be effectively treated with antibiotic therapy. Venereologists recommend the following medications: azithromycin, doxycycline, erythromycin or ofloxacin. Pregnant women are recommended to take erythromycin or amoxicillin.
More information of the treatment
Forecast
If therapy is inadequate, complications may develop.
- Women with mucopurulent discharge from the cervical canal, symptoms of adnexitis, infertility.
- Persons who have had sexual contact with a person infected with chlamydia.
- People undergoing testing for other STIs.
- Newborns born to mothers who had chlamydial infection during pregnancy.