
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
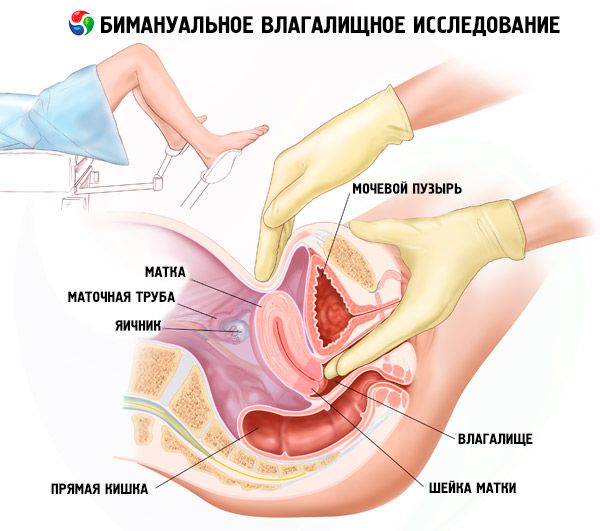
Bimanual vaginal examination
Medical expert of the article
Last reviewed: 04.07.2025
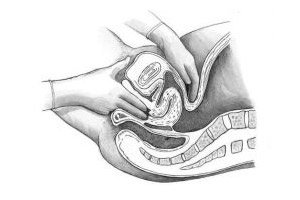
Vaginal (internal) examination is performed with the middle and index fingers of one hand (usually the right). The other hand must first separate the labia. Vaginal examination allows determining the condition of the pelvic floor muscles, large glands of the vestibule, urethra, vagina (volume, extensibility, soreness, presence of pathological processes, condition of the vaults), vaginal part of the cervix (position, size, shape, consistency, surface, mobility, soreness, condition of the external os).
The examination is then continued with both hands (inserted into the vagina and with the other hand through the anterior abdominal wall).
Bimanual vaginal (bimanual, combined, vaginal-abdominal) examination is the main method for recognizing diseases of the uterus, appendages, pelvic peritoneum and tissue. When examining the uterus, its position (tilt, bend, etc.), size, shape, consistency, mobility, and soreness are determined. By moving the outer hand to the lateral walls of the pelvis (alternately), and the inner hand to the lateral fornices of the vagina, the uterine appendages are examined. Unchanged fallopian tubes and ovaries are usually not palpated.
Using the brush of the second hand, palpation of the pelvic organs is performed from the side of the abdominal wall according to certain rules. In this case, it is possible to determine the width of the vaginal opening, the condition of the perineum, the pelvic floor muscles, the length of the vagina, the depth of the vaginal vaults, the length and condition of the vaginal part of the cervix, the body of the uterus (position, size, consistency, mobility, soreness, shape, etc.) and appendages (fallopian tubes and ovaries). This examination can also provide an idea of the condition of the pelvic walls (bone exostoses).
To obtain the most complete information, it is necessary to adhere to a certain sequence. Diseases of the urethra are excluded, its condition is determined (thickened, compacted, painful). The capacity of the vagina, the severity of the folding of the mucous membrane, the condition of its walls are assessed.
The next stage is the examination of the vaginal part of the cervix. Its normal size is approximately the nail phalanx of the thumb.
In women who have given birth, the cervix is cylindrical in shape, while in women who have not given birth, it is cone-shaped. The consistency of the cervical tissue is dense. The condition of the external os (normally closed) is of great importance.
After this, the uterus is examined. Its shape, size, consistency, mobility, sensitivity to palpation and movement are determined.
An enlarged uterus may indicate pregnancy or a tumor. Different consistency, asymmetry of the uterus, combined with its enlargement, may be associated with a tumor process. Limitation of uterine mobility is most often caused by an inflammatory or adhesive process.
The next stage is to establish the condition of the uterine appendages. For this, the examining fingers are alternately moved to the lateral vaults. Unchanged uterine appendages can be palpated in a thin woman and with good relaxation of the anterior abdominal wall.
If the appendages are palpated, attention is paid to their size, shape, clarity of contours, surface character, consistency, mobility and sensitivity.
In acute inflammatory diseases of the uterine appendages, internal examination is painful, the contours of the palpated organs are unclear, and it is often impossible to separate the uterus from the general inflammatory conglomerate by palpation. In chronic inflammation, the altered appendages are palpated more clearly, are less painful, and are located in adhesions that limit their movement.
Ovarian cysts are usually unilateral, palpated as a clear round formation with a smooth surface, fairly mobile and painless.
Ovarian cysts have a denser, sometimes uneven consistency; tumor movement may be limited.
In advanced forms of ovarian cancer, massive, immobile tumor conglomerates are found in the pelvis. It is not possible to palpate the uterus.
Then they move on to examining the parametria. Usually, the parametrium tissues are not felt with the fingers. In inflammatory diseases of the genitals, the tissue may appear edematous, sharply painful, in some cases it becomes denser (after inflammation suffered in the past). It is necessary to assess the condition of the parametria in malignant neoplasms, since metastasis in cervical cancer occurs along the lymphatic pathways to the lymph nodes on the lateral walls of the pelvis. In this case, the tissue becomes denser, and the cervix is pulled upward or to one of the lateral walls of the pelvis.
Some changes can also be detected in the sacrouterine ligaments (in chronic inflammatory processes with prevalence of cicatricial-adhesive changes). The ligaments (behind the uterus) are palpated as thickened, shortened, and sharply painful. Movements of the uterus, especially forward, cause sharp pain.
Rectal, rectal-abdominal and recto-vaginal examinations are performed according to indications (or as an additional examination) in virgins, with atresia or stenosis of the vagina, with inflammatory or tumor processes in the reproductive system.
A rectal examination is performed with the 2nd finger of the right hand and several fingers of the left (rectoabdominal). It helps to visualize the condition of the cervix, paravaginal and pararectal tissue, to establish changes in the rectum (narrowing, compression by a tumor, infiltration of the walls, etc.). This examination is also used in patients who have not had sexual intercourse (with a preserved hymen ). A rectovaginal examination is performed by inserting the 2nd finger into the vagina and the 3rd into the rectum. This combined examination is advisable to use if there is a suspicion of pathological changes in the parametric tissue and in the rectouterine space.
All women undergo a gynecological examination to obtain bacteriological smears from the urethra, vagina and cervical canal. The material is applied to two slides, each divided (from below) into three parts - U (urethra), C (cervical canal) and V (vagina). Before taking the smears, the urethra is lightly massaged (outward). The discharge is taken with a grooved probe, the tip of tweezers or, preferably, by light scraping with a special spoon (Volkman) and applied to both slides (on part M). To take the following smears, speculums are inserted into the vagina. A smear from the cervical canal is taken in the same way as from the urethra. Discharge from the posterior fornix of the vagina is usually taken with a spatula (tweezers, forceps). The smears are applied to the corresponding parts of the slides (C and V).
For cytological examination, smears and material from the cervical canal are taken from the surface of the cervix of all women who are initially examined by a gynecologist in an outpatient clinic or admitted to a hospital."
What's bothering you?
What do need to examine?


 [
[