
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
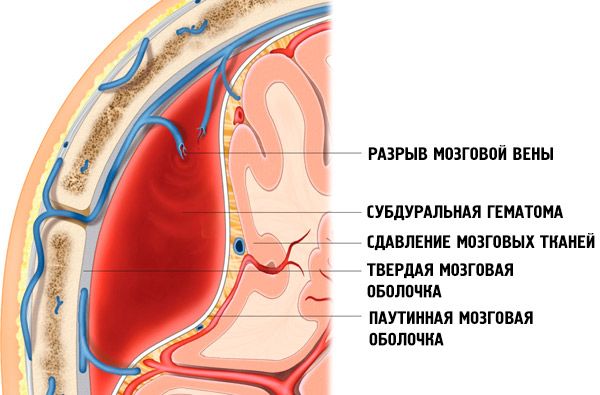
Subdural hematoma
Medical expert of the article
Last reviewed: 04.07.2025
A subdural hematoma is a large collection of blood located between the dura mater and arachnoid mater, causing compression of the brain.
Isolated subdural hematomas account for approximately 2/5 of the total number of intracranial hemorrhages and rank first among the various types of hematomas. Among victims with traumatic brain injury, acute subdural hematoma accounts for 1-5%, reaching 9-22% in severe traumatic brain injury. Subdural hematomas predominate in men compared to women (3:1), they are found in all age categories, but more often in people over 40 years of age.
Epidemiology
The vast majority of subdural hematomas are formed as a result of traumatic brain injury. Much less often they occur in vascular pathology of the brain (for example, hypertension, arterial aneurysms, arteriovenous malformations, etc.), and in some cases they are a consequence of taking anticoagulants. Isolated subdural hematomas account for approximately 2/5 of the total number of intracranial hemorrhages and rank first among the various types of hematomas. Among victims with traumatic brain injury, acute subdural hematoma accounts for 1-5%, reaching 9-22% in severe traumatic brain injury. Subdural hematomas predominate in men compared to women (3:1), they are found in all age categories, but more often in people over 40 years old.
Causes subdural hematoma
The vast majority of subdural hematomas are formed as a result of craniocerebral trauma. Much less frequently, they occur in vascular pathology of the brain (for example, hypertension, arterial aneurysms, arteriovenous malformations, etc.), and in some cases they are a consequence of taking anticoagulants.
Pathogenesis
Subdural hematomas develop with head trauma of varying severity. Acute subdural hematomas are more typically caused by severe craniocerebral trauma, while subacute and (especially) chronic hematomas are more typically caused by relatively mild trauma. Unlike epidural hematomas, subdural hematomas occur not only on the side where the traumatic agent was applied, but also on the opposite side (with approximately the same frequency).
The mechanisms of formation of subdural hematomas are different. In case of homolateral injuries it is to some extent similar to the formation of epidural hematomas, i.e. a traumatic agent with a small area of application affects a motionless or slightly moving head, causing a local contusion of the brain and rupture of pial or cortical vessels in the area of injury.
The formation of subdural hematomas contralateral to the site of application of the traumatic agent is usually caused by displacement of the brain, which occurs when the head, which is in comparatively fast motion, hits a massive stationary or slow-moving object (falling from a relatively great height, from a moving vehicle onto the pavement, collision of cars, motorcycles, falling backwards, etc.). In this case, the so-called bridge veins, which flow into the superior sagittal sinus, are ruptured.
The development of subdural hematomas is possible even in the absence of direct application of a traumatic agent to the head. A sharp change in speed or direction of movement (with a sudden stop of fast-moving transport, a fall from a height onto the feet, buttocks, etc.) can also cause displacement of the cerebral hemispheres and ruptures of the corresponding veins.
In addition, subdural hematomas on the opposite side may occur when a traumatic agent with a wide area of application is applied to a fixed head, when there is not so much a local deformation of the skull as a displacement of the brain, often with a rupture of the veins flowing into the sagittal sinus (a blow from a log, a falling object, a snow block, the side of a car, etc.). Often, different mechanisms are simultaneously involved in the formation of subdural hematomas, which explains the significant frequency of their bilateral location.
In some cases, subdural hematomas are formed due to direct injury to the venous sinuses, when the integrity of the dura mater is compromised with rupture of its vessels, and also when the cortical arteries are damaged.
In the development of subacute and (especially) chronic subdural hematomas, a significant role is also played by secondary hemorrhages, which occur as a result of the disruption of the integrity of blood vessels under the influence of dystrophic, angioedema and angioedema factors.
Symptoms subdural hematoma
The symptoms of subdural hematomas are extremely variable. Along with their volume, source of bleeding, rate of formation, localization, spread and other factors, this is due to more frequent severe concomitant brain damage than with epidural hematomas; often (due to the counter-impact mechanism) they are bilateral.
The clinical picture consists of general cerebral, local and secondary brainstem symptoms, which is caused by compression and dislocation of the brain with the development of intracranial hypertension. Typically, there is a so-called "light" interval - time after injury, when clinical manifestations of subdural hematoma are absent. The duration of the "light" interval (expanded or erased) in subdural hematomas varies widely - from several minutes and hours (in their acute development) to several days (in subacute development). In chronic course, this interval can reach several weeks, months and even years. In such cases, clinical manifestations of hematoma can be provoked by a variety of factors: additional trauma, fluctuations in blood pressure, etc. In concomitant brain contusions, the "light" interval is often absent. With subdural hematomas, wave-like and gradual changes in the state of consciousness are more pronounced than with epidural ones. However, sometimes patients suddenly fall into a coma, as with epidural hematomas.
Thus, the three-phase nature of disorders of consciousness (primary loss of consciousness after injury, its recovery for some period and subsequent repeated loss) often described when characterizing the clinical course of subdural hematoma may be absent.
Unlike epidural hematomas, in which disturbances of consciousness occur mainly according to the brainstem type, with subdural hematomas, especially subacute and chronic ones, disintegration of consciousness according to the cortical type is often noted with the development of amentive, oneiroid, delirium-like states, memory impairment with features of Korsakov's syndrome, as well as "frontal psyche" with a decrease in criticism of one's condition, aspontaneity, euphoria, ridiculous behavior, and impaired control over the functions of the pelvic organs.
In the clinical picture of subdural hematomas, psychomotor agitation is often noted. With subdural hematomas, epileptic seizures are encountered somewhat more often than with epidural ones. Generalized convulsive paroxysms predominate.
Headache in contactable patients with subdural hematoma is an almost constant symptom. Along with cephalgia, which has a meningeal tint (radiation of pain to the eyeballs, back of the head, pain during eye movements, photophobia, etc.), and objectified local pain during percussion of the skull, diffuse hypertensive headaches accompanied by a feeling of "bursting" of the head are encountered much more often with subdural hematomas than with epidural ones. The period of intensification of headaches with subdural hematoma is often accompanied by vomiting.
In approximately half of the observations with subdural hematomas, bradycardia is recorded. With subdural hematomas, unlike epidural ones, congestion in the fundus is a more frequent component of the compression syndrome. In patients with chronic hematomas, congestive discs with decreased visual acuity and elements of optic nerve disc atrophy can be detected. It should be noted that due to severe concomitant brain contusions, subdural hematomas, especially acute ones, are often accompanied by brainstem disorders in the form of respiratory disorders, arterial hyper- or hypotension, early hyperthermia, diffuse changes in muscle tone and the reflex sphere.
For subdural hematomas, in contrast to epidural ones, the prevalence of general cerebral symptoms over the relatively widespread focal ones is more typical. However, concomitant contusions, as well as dislocation phenomena, sometimes cause the presence of complex relationships of various groups of symptoms in the clinical picture of the disease.
Among the focal signs in subdural hematomas, the most important role is played by unilateral mydriasis with a decrease or loss of pupillary response to light. Mydriasis, homolateral to the subdural hematoma, is found in half of the observations (and in 2/3 of cases with acute subdural hematomas), which significantly exceeds the number of similar findings in epidural hematomas. Dilation of the pupil on the side opposite the hematoma is noted much less often, it is caused by a contusion of the opposite hemisphere or infringement of the cerebral peduncle opposite the hematoma in the opening of the cerebellar tentorium. In acute subdural hematoma, the maximum dilation of the homolateral pupil with a loss of its response to light predominates. In subacute and chronic subdural hematomas, mydriasis is often moderate and dynamic, without loss of photoreactions. Often, a change in pupil diameter is accompanied by ptosis of the upper eyelid on the same side, as well as limited mobility of the eyeball, which may indicate craniobasal radicular genesis of oculomotor pathology.
Pyramidal hemisyndrome in acute subdural hematoma, unlike epidural hematoma, is inferior to mydriasis in diagnostic significance. In subacute and chronic subdural hematoma, the lateralization role of pyramidal symptoms increases. If pyramidal hemisyndrome reaches the level of deep paresis or paralysis, then this is most often due to concomitant brain contusion. When subdural hematomas occur in their "pure form", pyramidal hemisyndrome is usually characterized by anisoreflexia, a slight increase in tone and a moderate decrease in strength in the extremities contralateral to the hematoma. Insufficiency of the VII cranial nerve in subdural hematomas usually has a mimic tint.
In subdural hematomas, pyramidal hemi-syndrome is more often than in epidural hematomas homolateral or bilateral due to concomitant contusion or dislocation of the brain. The rapid significant reduction of dislocation hemiparesis in the reflux of the brainstem infringement and the comparative stability of hemi-syndrome due to contusion of the brain help differentiate the cause. It should also be remembered that the bilaterality of pyramidal and other focal symptoms may be due to the bilateral location of subdural hematomas.
With subdural hematomas, symptoms of irritation in the form of focal seizures usually appear on the side of the body opposite the hematoma.
When a subdural hematoma is localized over the dominant hemisphere, speech disorders, most often sensory ones, are often detected.
Sensitivity disorders are significantly less frequent than pyramidal symptoms, but still occur more frequently with subdural hematomas than with epidural ones, and are characterized not only by hypalgesia, but also by disorders of epicritic types of sensitivity. The proportion of extrapyramidal symptoms with subdural hematomas, especially chronic ones, is comparatively high. They reveal plastic changes in muscle tone, general stiffness and slowness of movements, reflexes of oral automatism and a grasping reflex.
Where does it hurt?
What's bothering you?
Forms
The opinion about the relatively slow development of subdural hematomas, compared to epidural ones, has long dominated in the literature. At present, it has been established that acute subdural hematomas are often not inferior to epidural ones in their rapid rate of development. Subdural hematomas are divided into acute, subacute and chronic according to their course. Acute hematomas include those in which brain compression is clinically manifested on the 1st-3rd day after a craniocerebral injury, subacute ones - on the 4th-10th day, and chronic subdural hematomas - those manifesting 2 weeks or more after the injury. Non-invasive visualization methods have shown that these terms are very conditional, however, the division into acute, subacute and chronic subdural hematomas retains its clinical significance.
Acute subdural hematoma
Acute subdural hematoma in approximately half of the cases is manifested by a picture of brain compression in the first 12 hours after the injury. Three main variants of the clinical picture of acute subdural hematomas should be distinguished.
 [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ]
[ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ]
Classic version
The classic variant is rare. It is characterized by a three-phase change in the state of consciousness (primary loss at the moment of injury, an extended "light" interval, and a secondary shutdown of consciousness).
At the moment of a relatively mild craniocerebral injury (mild or moderate brain contusion), a short-term loss of consciousness is observed, during the recovery of which only moderate stunning or its elements are observed.
During the lucid interval, lasting from 10-20 minutes to several hours, occasionally 1-2 days, patients complain of headache, nausea, dizziness, and amnesia. With adequate behavior and orientation in the surrounding environment, rapid exhaustion and slowing of intellectual and mnestic processes are detected. Focal neurological symptoms during the lucid interval, if present, are usually mild and diffuse.
Later, the stupor deepens with the appearance of increased drowsiness or psychomotor agitation. Patients become inadequate, headaches increase sharply, and vomiting recurs. Focal symptoms in the form of homolateral mydriasis, contralateral pyramidal insufficiency and sensitivity disorders, as well as other dysfunctions of a relatively large cortical zone, become more clearly manifested. Along with the loss of consciousness, secondary brainstem syndrome develops with bradycardia, increased blood pressure, changes in respiratory rhythm, bilateral vestibulo-oculomotor and pyramidal disorders, and tonic convulsions.
Option with erased "light" gap
This variant is often encountered. Subdural hematoma is usually combined with severe brain contusions. Primary loss of consciousness often reaches the level of coma. Focal and brainstem symptoms caused by primary damage to the brain matter are expressed. Later, partial recovery of consciousness is noted before stunning, usually deep. During this period, disorders of vital functions are somewhat reduced. In a victim who has come out of a coma, psychomotor agitation and search for an antalgic position are sometimes noted. Often it is possible to detect a headache, meningeal symptoms are expressed. After a certain period of time (from several minutes to 1-2 days), the erased "light" interval is replaced by a repeated shutdown of consciousness up to stupor or coma with deepening disorders of vital functions, the development of vestibular-oculomotor disorders and decerebrate rigidity. As the comatose state develops, focal symptoms caused by the hematoma worsen, in particular, unilateral mydriasis appears or becomes extreme, hemiparesis increases, and sometimes epileptic seizures may develop.
Option without a "light" gap
The variant without a "light" interval is often encountered, usually with multiple severe brain injuries. Stupor (and more often coma) from the moment of injury to surgery or death of the patient does not undergo any significant positive dynamics.
Subacute subdural hematoma
Subacute subdural hematoma, unlike acute hematoma, is characterized by a relatively slow development of compression syndrome and a significantly longer duration of the "clear" interval. In this regard, it is often regarded as a concussion or brain injury, and sometimes as a non-traumatic disease (flu, meningitis, spontaneous subarachnoid disease, alcohol intoxication, etc.). Despite the often early formation of subacute subdural hematomas, their threatening clinical manifestation usually occurs 3 days after the injury. The severity of the injury is often inferior to that of acute hematoma. In most cases, they occur with relatively mild head injuries.
Three-phase changes in consciousness are much more characteristic of subacute subdural hematoma than of acute hematoma. The duration of the initial loss of consciousness in most victims ranges from several minutes to an hour. The subsequent "light" period can last up to 2 weeks, manifesting itself in a more typically expanded version.
During the "light" interval, the victims are in a clear consciousness or only elements of stunning are present. Vital functions are not affected, and if an increase in blood pressure and bradycardia are noted, then they are very insignificant. Neurological symptoms are often minimal, sometimes they are manifested by a single symptom.
The dynamics of secondary loss of consciousness in victims is variable.
Sometimes wave-like fluctuations of consciousness are observed within the limits of stupefaction of varying degrees, and sometimes even stupor. In other cases, secondary loss of consciousness develops progressively: more often - gradually over the course of hours and days, less often - with a violent entry into a coma. At the same time, among victims with subdural hematomas, there are also those who, with the increase of other symptoms of brain compression, have a long-term impairment of consciousness within the limits of moderate stupefaction.
With subacute subdural hematomas, mental changes are possible in the form of decreased critical attitude towards one’s condition, disorientation in place and time, euphoria, inappropriate behavior, and apathetic-abulic phenomena.
Subacute subdural hematoma often manifests itself as psychomotor agitation provoked by headaches. Due to the availability of patients to contact, the increasing headache appears more vividly than with acute hematomas, playing the role of the main symptom. Along with vomiting, bradycardia, arterial hypertension, congestion in the fundus becomes an important component of the diagnosis of compression syndrome. They tend to initially develop on the side of the hematoma.
Stem symptoms in subacute subdural hematoma are encountered much less frequently than in acute hematoma, and they are almost always secondary in genesis - compression. Among lateralization signs, the most significant are homolateral mydriasis and contralateral pyramidal insufficiency, they appear or increase during observation. It should be taken into account that in the phase of gross clinical decompensation, pupil dilation may also appear on the side opposite to the hematoma. Pyramidal hemisyndrome in subacute subdural hematomas is usually expressed moderately and is much less often than in acute hematomas, it is bilateral. Due to the patient's availability, it is almost always possible to detect focal hemispheric symptoms, even if they are mild or selectively represented by sensitivity disorders, visual fields, as well as disorders of higher cortical functions. With localization of hematomas over the dominant hemisphere, aphasic disorders occur in half of the cases. Some patients develop focal seizures on the opposite side of the body.
Chronic subdural hematomas
Subdural hematomas are considered chronic if they are detected or removed 14 days or more after a traumatic brain injury. However, their main distinguishing feature is not the verification period itself, but the formation of a capsule that gives a certain autonomy in coexistence with the brain and determines all subsequent clinical and pathophysiological dynamics.
 [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ], [ 34 ]
[ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ], [ 34 ]
Diagnostics subdural hematoma
When recognizing a subdural hematoma, one often has to overcome difficulties caused by the variety of forms of clinical manifestation and course. In cases where a subdural hematoma is not accompanied by severe concomitant brain damage, its diagnosis is based on a three-phase change in consciousness: primary loss at the moment of injury, a "lucid" interval, and repeated loss of consciousness caused by compression of the brain.
If, with a relatively slow development of brain compression, the clinical picture reveals, along with other signs, diffuse bursting headaches, mental changes of the "frontal" type and psychomotor agitation, there is reason to assume the development of a subdural hematoma. The mechanism of injury may also incline to this conclusion: a blow to the head with a blunt object (usually to the occipital, frontal or sagittal region), a blow to the head against a massive object or a sharp change in the speed of movement, leading not so much to a local impression as to a displacement of the brain in the cranial cavity with the possibility of rupture of the bridging veins and the formation of a subdural hematoma on the side opposite to the site of application of the traumatic agent.
When recognizing subdural hematomas, one should take into account the frequent predominance of general cerebral symptoms over focal ones, although these ratios are variable. The nature of focal symptoms in isolated subdural hematoma (their comparative softness, prevalence, and often bilaterality) can facilitate diagnosis. The assumption of a subdural hematoma can be indirectly supported by the features of hemispheric symptoms. Detection of sensitivity disorders is more typical for subdural hematomas. Craniobasal symptoms (and among them, first of all, homolateral mydriasis) are often more pronounced than in epidural hematomas.
The diagnosis of subdural hematomas is especially difficult in victims with severe concomitant brain damage, when the "lucid" interval is absent or erased. In victims in stupor or coma, bradycardia, increased blood pressure, epileptic seizures raise concerns regarding the possibility of brain compression. The occurrence or tendency to worsen respiratory disorders, hyperthermia, reflex paresis of upward gaze, decerebrate rigidity, bilateral pathological signs and other brainstem pathology support the assumption of brain compression by a hematoma.
Detection of traumatic traces in the occipital, frontal or sagittal region (especially if the mechanism of injury is known), clinical (bleeding, cerebrospinal fluid rhinorrhea from the nose, ears) and radiographic signs of a skull base fracture allow one to approximately lean towards the diagnosis of a subdural hematoma. For its lateralization, the side of mydriasis should be taken into account first.
In case of subdural hematoma, unlike epidural, craniographic findings are not so characteristic and important for local diagnostics. In acute subdural hematoma, fractures of the skull base are often detected, usually extending to the middle and posterior, less often - to the anterior cranial fossa. Combinations of damage to the bones of the base and cranial vault are detected. Isolated fractures of individual bones of the cranial vault are less common. If damage to the bones of the vault is detected in acute subdural hematoma, then they are usually extensive. It should be taken into account that, unlike epidural, bone damage in subdural hematomas is often found on the side opposite the hematoma. In general, bone damage is absent in a third of victims with acute subdural hematomas and in 2/3 - with subacute ones.
Linear echoes may facilitate the recognition of subdural hematoma by revealing the lateralization of the traumatic substrate compressing the brain.
In cerebral angiography for subdural hematomas on direct images, the "border" symptom is typical - a sickle-shaped avascular zone in the form of a strip of varying width. The "border" more or less evenly displaces the vascular pattern of the compressed hemisphere from the cranial vault along the length from the sagittal suture to the base of the skull, which can be seen in images in the frontal plane. It should be taken into account that the "border" symptom is often more clearly expressed in the capillary or venous phase. Displacement of the anterior cerebral artery is also characteristic. Lateral angiograms for convexital subdural hematomas are less demonstrative. However, for subdural hematomas located in the interhemispheric fissure, lateral images are also convincing: they reveal downward compression of the pericallous artery.
CT and MRI play a decisive role in recognizing a subdural hematoma and in clarifying its location, size, and impact on the brain.
Acute subdural hematoma on CT scan is usually characterized by a crescent-shaped zone of homogeneous increased density.
In most cases, the subdural hematoma extends to the entire hemisphere or most of it. Subdural hematomas can often be bilateral and extend to the interhemispheric fissure and the tentorium cerebelli. The absorption coefficients of acute epidural hematoma are higher than the density of subdural hematoma due to the latter being mixed with cerebrospinal fluid and/or detritus. For this reason, the inner edge of acute and subacute subdural hematoma, repeating the surface relief of the underlying brain, may have an unclear outline. Atypical localization of subdural hematomas - in the interhemispheric fissure, above or below the tentorium, at the base of the middle cranial fossa - is a much rarer finding than convexital.
Over time, as a result of liquefaction of the hematoma contents and the disintegration of blood pigments, its density gradually decreases, making diagnosis difficult, especially in cases where the absorption coefficients of the altered blood and the surrounding brain matter become the same. Subdural hematomas become isodense within 1-6 weeks. The diagnosis is then based on secondary signs, such as compression or medial displacement of the convexital subarachnoid grooves, narrowing of the homolateral lateral ventricle, and dislocation of the midline structures. The isodense phase is followed by a phase of reduced density, in which the absorption coefficient of the spilled blood approaches the density of the cerebrospinal fluid. With a subdural hematoma, the phenomenon of sedimentation is encountered: the lower part of the hematoma is hyperdense as a result of sedimentation of high-density blood elements, and the upper part is iso- or hypodense.
In case of subdural hematomas, the tomogram shows predominantly signs of reduction of intracranial reserve spaces: narrowing of the ventricular system, compression of convexital subarachnoid spaces, moderate or severe deformation of basal cisterns. Significant displacement of midline structures is accompanied by the development of dislocation hydrocephalus, combined with compression of subarachnoid spaces. When the hematoma is localized in the posterior cranial fossa, acute occlusive hydrocephalus develops.
After removal of the subdural hematoma, the position and size of the ventricular system, cisterns of the base of the brain and subarachnoid spaces are normalized.
On MRI images, acute subdural hematomas may have low image contrast due to the absence of methemoglobin. In 30% of cases, chronic subdural hematomas appear hypo- or isodense on T1-weighted tomograms, but almost all of them are characterized by increased signal intensity in T2 mode. In cases of repeated hemorrhages in subacute or chronic subdural hematomas, heterogeneity of their structure is noted. The capsule of chronic hematomas, as a rule, intensively accumulates a contrast agent, which allows them to be differentiated from hygromas and arachnoid cysts. MRI makes it possible to successfully detect subdural hematomas that are isodense on CT. MRI also has advantages in planar subdural hematomas, especially if they enter the interhemispheric fissure or extend basally.
What do need to examine?
What tests are needed?
Who to contact?
Treatment subdural hematoma
Treatment of subdural hematomas can be conservative and surgical. The choice of tactics depends on the volume of the hematoma, the phase of its development and the patient's condition.
Surgical treatment of subdural hematomas
Absolute indications for surgical treatment are as follows.
- Acute subdural hematoma causing compression and displacement of the brain. The operation must be performed as soon as possible after the injury. The sooner the subdural hematoma is removed, the better the outcome.
- Subacute subdural hematoma with increasing focal symptoms and/or signs of intracranial hypertension.
In other cases, the decision to operate is made based on a combination of clinical and radiological data.
Surgical technique for acute subdural hematoma
Wide craniotomy is usually indicated for complete removal of acute subdural hematoma and reliable hemostasis. The size and location of the osteoplastic trepanation depend on the extent of the subdural hematoma and the location of associated parenchymatous injuries. When a subdural hematoma is combined with contusions of the pole-basal parts of the frontal and temporal lobes, the lower border of the trepanation window should reach the base of the skull, and the other borders should correspond to the size and location of the subdural hematoma. Removal of the hematoma helps stop bleeding if it continues from the foci of brain crushing. In case of rapidly increasing brain dislocation, craniotomy should begin with the application of a burr hole through which part of the subdural hematoma can be quickly aspirated and thereby reduce the degree of brain compression. Then the remaining stages of the craniotomy should be quickly performed. However, no significant differences were found when comparing mortality in groups of patients where “rapid” removal of the subdural hematoma through a trephination hole was initially used and in the group of patients where bone-plastic trephination was immediately performed.
In case of a subdural hematoma, a tense, cyanotic, non-pulsating or weakly pulsating dura mater protrudes through the trephination window.
In the presence of concomitant polar-basal contusions of the frontal and temporal lobes on the side of the subdural hematoma, it is preferable to open the dura mater in an arcuate manner with the base toward the base, since in these cases the source of bleeding is most often the cortical vessels in the area of contusion foci. In the case of convexital-parasagittal localization of the subdural hematoma, the opening of the dura mater can be performed with the base toward the superior sagittal sinus.
In the presence of underlying intracerebral hematomas and crushing foci, blood clots and brain detritus are removed by irrigation and gentle aspiration. Hemostasis is achieved by bipolar coagulation, a hemostatic sponge, or fibrin-thrombin adhesive compositions. After suturing the dura mater or its plastic surgery, the bone flap can be put back in place and fixed with sutures. If prolapse of brain matter into the trepanation defect occurs, the bone flap is removed and preserved, i.e. the operation is completed by decompressive trepanation of the skull.
Errors in surgical tactics include removal of a subdural hematoma through a small resection window without suturing the dura mater. This does allow for rapid removal of the main part of the subdural hematoma, but is fraught with prolapse of brain matter into the bone window with compression of the convexital veins, disruption of venous outflow and increased cerebral edema. In addition, in conditions of cerebral edema after removal of a subdural hematoma through a small trepanation window, it is not possible to revise the source of bleeding and perform reliable hemostasis.
Drug treatment of subdural hematomas
Victims with a subdural hematoma in clear consciousness with a hematoma thickness of less than 10 mm, displacement of midline structures of no more than 3 mm, without compression of the basal cisterns usually do not require surgical intervention.
In victims who are in a stupor or coma, with a stable neurological status, no signs of brainstem compression, intracranial pressure not exceeding 25 mm Hg, and a subdural hematoma volume of no more than 40 ml, conservative therapy may be administered under dynamic clinical, as well as CT and MRI control.
Resorption of a flat subdural hematoma usually occurs within a month. In some cases, a capsule forms around the hematoma and the hematoma transforms into a chronic one. If, during dynamic observation, the gradual transformation of a subdural hematoma into a chronic one is accompanied by a deterioration in the patient's condition or an increase in headaches, the appearance of congestion in the fundus, there is a need for surgical intervention by closed external drainage.
Forecast
Acute subdural hematoma is often less favorable in prognosis than acute epidural hematoma. This is due to the fact that subdural hematomas usually occur with primary severe brain damage, and are also accompanied by a rapid rate of brain displacement and compression of stem structures. Therefore, despite the introduction of modern diagnostic methods, acute subdural hematomas have a relatively high mortality rate, and among surviving victims, severe disability is significant.
The speed of detection and removal of the subdural hematoma is also of significant importance for the prognosis. The outcomes of surgical treatment are significantly better in victims operated on in the first 4-6 hours after the injury, compared with the group of patients operated on at a later date. The volume of the subdural hematoma, as well as the age of the victims, play an increasingly negative role in the outcomes as it increases.
Unfavorable outcomes in subdural hematoma are also due to the development of intracranial hypertension and cerebral ischemia. Recent studies have shown that these ischemic disturbances can be reversible with rapid removal of cerebral compression. Important prognostic factors include cerebral edema, which often progresses after removal of acute subdural hematoma.

