
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Spinal cord
Medical expert of the article
Last reviewed: 07.07.2025
The spinal cord (medulla spinalis) is a long, cylindrical cord, flattened from front to back. Because of this, the transverse diameter of the spinal cord is greater than the anteroposterior diameter.
The spinal cord is located in the spinal canal and at the level of the lower edge of the foramen magnum it passes into the brain. At this point, the roots that form the right and left spinal nerves emerge from the spinal cord (its upper border). The lower border of the spinal cord corresponds to the level of the I-II lumbar vertebrae. Below this level, the apex of the medullary cone of the spinal cord continues into a thin terminal thread. The terminal thread (filum terminale) in its upper sections still contains nervous tissue and is a rudiment of the caudal end of the spinal cord. This part of the terminal thread, called the internal one, is surrounded by the roots of the lumbar and sacral spinal nerves and, together with them, is located in a blind-ending sac formed by the dura mater of the spinal cord. In an adult, the internal part of the terminal thread is about 15 cm long. Below the level of the second sacral vertebra, the terminal thread is a connective tissue formation that is a continuation of all three membranes of the spinal cord and is called the external part of the terminal thread. The length of this part is about 8 cm. It ends at the level of the body of the second coccygeal vertebra, fusing with its periosteum.
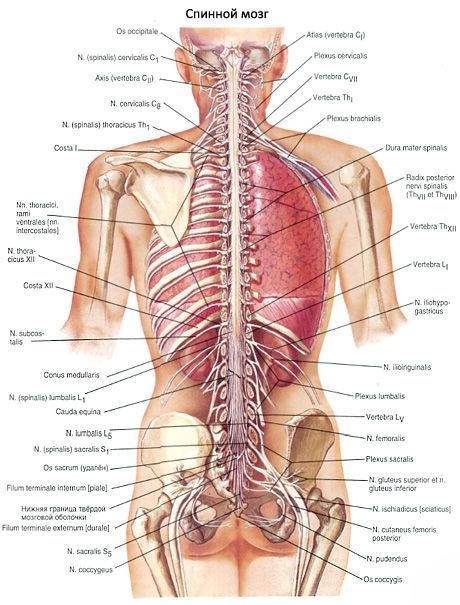
The length of the spinal cord in an adult is on average 43 cm (in men - 45 cm, in women - 41-42 cm), weight - about 34-38 g, which is approximately 2% of the mass of the brain.
In the cervical and lumbosacral sections of the spinal cord, two noticeable thickenings are found - the cervical thickening (intumescentia cervicalis) and the lumbosacral thickening (intumescentia lumbosacralis). The formation of thickenings is explained by the fact that the cervical and lumbosacral sections of the spinal cord innervate the upper and lower extremities, respectively. In these sections, the spinal cord contains a greater number of nerve cells and fibers than in other sections. In the lower sections, the spinal cord gradually narrows and forms the medullary cone (conus medullaris).
On the anterior surface of the spinal cord, the anterior median fissure (fissura medidna anterior) is visible, which projects into the spinal cord tissue deeper than the posterior median groove (sulcus medianus posterior). They are the boundaries dividing the spinal cord into two symmetrical halves. In the depths of the posterior median groove, there is a glial posterior median septum (septum medianum posterius) penetrating almost the entire thickness of the white matter. This septum reaches the posterior surface of the gray matter of the spinal cord.
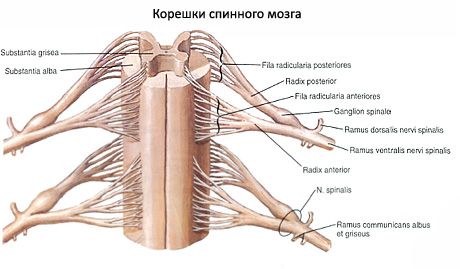
On the anterior surface of the spinal cord, on each side of the anterior fissure, there is an anterior lateral groove (sulcus anterolateralis). It is the place where the anterior (motor) roots of the spinal nerves exit the spinal cord and the border on the surface of the spinal cord between the anterior and lateral funiculi. On the posterior surface, on each half of the spinal cord, there is a posterior lateral groove (sulcus posterolateralis) - the place where the posterior sensory roots of the spinal nerves penetrate the spinal cord. This groove serves as the border between the lateral and posterior funiculi.

The anterior rootlet (radix anterior) consists of the processes of motor nerve cells located in the anterior horn of the gray matter of the spinal cord. The posterior rootlet (radix posterior) is sensitive and is represented by a set of central processes of pseudounipolar cells penetrating the spinal cord, the bodies of which form a spinal ganglion (ganglion spinale) located in the spinal canal at the junction of the posterior rootlet with the anterior rootlet. Along the entire length of the spinal cord, 31-33 pairs of roots extend from each side. The anterior and posterior roots converge at the inner edge of the intervertebral foramen, merge with each other and form a spinal nerve (nervus spinalis).
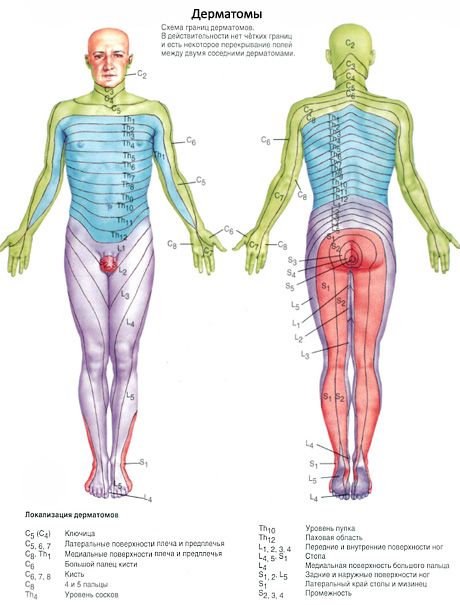
Thus, 31-33 pairs of spinal nerves are formed from the roots. The section of the spinal cord corresponding to two pairs of roots (two anterior and two posterior) is called a segment. Accordingly, 31-33 pairs of spinal nerves in the spinal cord are divided into 31-33 segments: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral and 1-3 coccygeal segments. Each segment of the spinal cord corresponds to a certain area of the body that receives innervation from this segment. Segments are designated by initial letters indicating the region (part) of the spinal cord, and numbers corresponding to the ordinal number of the segment:
- cervical segments (segmenta cervicalia) - CI-CVIII;
- thoracic segments (segmenta thoracica) - ThI-ThXII;
- lumbar segments (segmenta lumbalia) - LI-LV;
- sacral segments (segmenta sacralia) - SI-SV;
- coccygeal segments (segmenta coccygea) - CoI-CoIII.
It is very important for a physician to know the topographic relationships of the spinal cord segments with the vertebral column (skeletotopy of segments). The length of the spinal cord is significantly less than the length of the vertebral column. Therefore, the ordinal number of any segment of the spinal cord and the level of its position, starting from the lower cervical region, do not correspond to the ordinal number of the vertebra. The positions of the segments in relation to the vertebrae can be determined as follows. The upper cervical segments are located at the level of the vertebral bodies corresponding to their ordinal number. The upper thoracic segments lie one vertebra higher than the bodies of the corresponding vertebrae. In the middle thoracic region, this difference between the corresponding segment of the spinal cord increases by 2 vertebrae, in the lower thoracic region - by 3. The lumbar segments of the spinal cord lie in the spinal canal at the level of the bodies of the 10th and 11th thoracic vertebrae, the sacral and coccygeal segments - at the level of the 12th thoracic and 1st lumbar vertebrae.
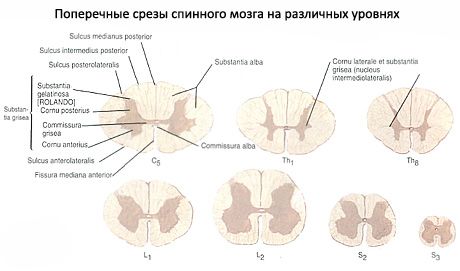
The spinal cord consists of nerve cells and fibers of gray matter, which in cross-section looks like the letter H or a butterfly with spread wings. On the periphery of the gray matter is the white matter, formed only by nerve fibers.
In the gray matter of the spinal cord there is a central canal (canalis centralis). It is a remnant of the cavity of the neural tube and contains cerebrospinal fluid. The upper end of the canal communicates with the fourth ventricle of the brain, and the lower end, slightly expanding, forms a small terminal ventricle (ventriculus terminalis) that ends blindly. The walls of the central canal of the spinal cord are lined with ependyma, around which there is a central gelatinous (gray) substance (substantia gelatinosa centralis). The ependyma is a dense layer of ependymocytes (neuroglial cells) that perform demarcation and support functions. On the surface facing the cavity of the central canal, there are numerous cilia that can facilitate the flow of cerebrospinal fluid in the canal. Thin long branching processes extend from the ependymocytes into the brain tissue, performing a supporting function. In adults, the central canal grows into various parts of the spinal cord, and sometimes throughout its entire length.
The gray matter (substantia gnsea) along the spinal cord to the right and left of the central canal forms symmetrical gray columns (columnae griseae). In front and behind the central canal of the spinal cord, these columns are connected to each other by thin plates of gray matter, called the anterior and posterior gray commissures.
Each column of gray matter has an anterior part, the anterior column (columna ventralis, s. anterior), and a posterior part, the posterior column (columna dorsalis, s. posterior). At the level of the lower cervical, all thoracic, and two upper lumbar segments (from CVII to LI-LII) of the spinal cord, the gray matter on each side forms a lateral protrusion, the lateral column (columna lateralis). In other parts of the spinal cord (above the VIII cervical and below the II lumbar segments), the lateral columns are absent.
In a cross-section of the spinal cord, the columns of gray matter on each side look like horns. There is a wider anterior horn (cornu ventrale, s.anterius) and a narrow posterior horn (cornu dorsale, s. posterius), corresponding to the anterior and posterior columns. The lateral horn (cornu laterale) corresponds to the lateral intermediate (autonomous) column of gray matter of the spinal cord.
The anterior horns contain large nerve root cells - motor (efferent) neurons. These neurons form 5 nuclei: two lateral (anterior and posterolateral), two medial (anterior and posteromedial), and a central nucleus. The posterior horns of the spinal cord are represented mainly by smaller cells. The posterior, or sensory, roots contain central processes of pseudounipolar cells located in the spinal (sensory) nodes.
The gray matter of the posterior horns of the spinal cord is heterogeneous. The bulk of the nerve cells of the posterior horn form its own nucleus. In the white matter, immediately adjacent to the apex of the posterior horn of the gray matter, a border zone is distinguished. Anterior to the latter is the spongy zone, which received its name due to the presence in this section of a large-meshed glial network containing nerve cells. Even more anteriorly, the gelatinous substance (substantia galatinosa) is distinguished, consisting of small nerve cells. The processes of the nerve cells of the gelatinous substance, spongy zone and diffusely scattered throughout the gray matter of the fascicular cells communicate with neighboring segments. As a rule, these processes end in synapses with neurons located in the anterior horns of their segment, as well as the above- and below-lying segments. Directing from the posterior horns of the gray matter to the anterior horns, the processes of these cells are located along the periphery of the gray matter, forming a narrow border of white matter near it. These bundles of nerve fibers are called the anterior, lateral and posterior proper bundles (fasciculi proprii ventrales, s. anteriores, laterales et dorsales, s. posteriores). The cells of all nuclei of the posterior horns of the gray matter are, as a rule, intercalary (intermediate, or conductor) neurons. Neurites extending from nerve cells, the totality of which constitutes the central and thoracic nuclei of the posterior horns, are directed in the white matter of the spinal cord to the brain.
In the medial part of the base of the lateral horn, the thoracic nucleus (nucleus thoracicus) is clearly visible, well outlined by a layer of white matter, consisting of large nerve cells. This nucleus extends along the entire posterior column of gray matter in the form of a cellular cord (Clarke's nucleus). The largest diameter of this nucleus is at the level from the 11th thoracic to the 1st lumbar segment.
The intermediate zone of the gray matter of the spinal cord is located between the anterior and posterior horns. Here, from the VIII cervical to the II lumbar segment, there is a protrusion of gray matter - the lateral horn. In the lateral horns are the centers of the sympathetic part of the autonomic nervous system in the form of several groups of small nerve cells, united in the lateral intermediate (gray) matter [substantia (grisea) intermedia lateralis]. The axons of these cells pass through the anterior horn and exit the spinal cord as part of the anterior roots.
In the intermediate zone is located the central intermediate (gray) substance [substantia (grisea) intermedia centralis], the processes of the cells of which participate in the formation of the spinocerebellar tract. At the level of the cervical segments of the spinal cord between the anterior and posterior horns, and at the level of the upper thoracic segments - between the lateral and posterior horns in the white matter adjacent to the gray, is located the reticular formation (formatio reticularis). Here it has the appearance of thin crossbars of gray matter intersecting in different directions, and consists of nerve cells with a large number of processes.
The gray matter of the spinal cord with the posterior and anterior roots of the spinal nerves and proper bundles of white matter bordering the gray matter form the proper, or segmental, apparatus of the spinal cord. The main purpose of the segmental apparatus as the phylogenetically oldest part of the spinal cord is to carry out innate reactions (reflexes) in response to irritation (internal or external). I.P. Pavlov defined this type of activity of the segmental apparatus of the spinal cord with the term "unconditioned reflexes".
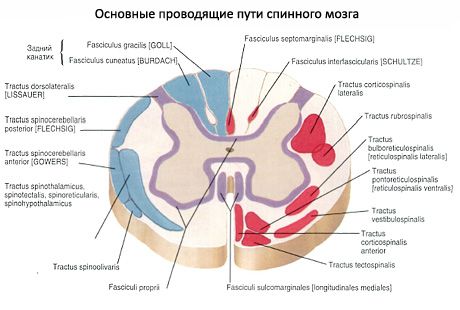
The white matter (substantia alba), as noted, is located outside the gray matter. The grooves of the spinal cord divide the white matter into three funiculi, symmetrically located on the right and left. The anterior funiculus (funiculus ventralis anterior) is located between the anterior median fissure and the anterior lateral sulcus. In the white matter posterior to the anterior median fissure, there is an anterior white commissure (commissura alba), which connects the anterior funiculi of the right and left sides. The posterior funiculus (funiculus dorsalis, s. posterior) is located between the posterior median and lateral sulci. The lateral funiculus (funiculus lateralis) is a section of white matter between the anterior and posterior lateral sulci.
The white matter of the spinal cord is represented by processes of nerve cells. The totality of these processes in the funiculi of the spinal cord constitute three systems of bundles (tracts, or conducting paths) of the spinal cord:
- short bundles of association fibers connecting segments of the spinal cord located at different levels;
- into the descending (afferent, sensory) bundles directed to the centers of the cerebrum and cerebellum;
- descending (efferent, motor) bundles that go from the brain to the cells of the anterior horns of the spinal cord.
The last two systems of bundles form a new (in contrast to the phylogenetically older segmental apparatus) suprasegmental conduction apparatus of bilateral connections of the spinal cord and brain. In the white matter of the anterior funiculi there are predominantly descending conduction pathways, in the lateral funiculi - both ascending and descending conduction pathways, in the posterior funiculi there are ascending conduction pathways.
The anterior funiculus includes the following conducting pathways:
1. The anterior corticospinal (pyramidal) tract [tractus corticospinalis (pyramidalis) ventralis, s. anterior] is motor and contains processes of giant pyramidal cells (giant pyramidal neurocytes). Bundles of nerve fibers that form this tract lie near the anterior median fissure, occupying the anteromedial parts of the anterior funiculus. The conduction tract transmits impulses of motor reactions from the cerebral cortex to the anterior horns of the spinal cord.
The reticular-spinal tract (tractus reticulospinalis) conducts impulses from the reticular formation of the brain to the motor nuclei of the anterior horns of the spinal cord. It is located in the central part of the anterior funiculus, lateral to the corticospinal tract.
The anterior spinothalamic tract (tractus spinothalamicus ventralis, s. anterior) is located somewhat in front of the reticular-spinal tract. Conducts impulses of tactile sensitivity (touch and pressure).
The tectospinal tract (tractus tectospinalis) connects the subcortical centers of vision (superior colliculi of the midbrain roof) and hearing (inferior colliculi) with the motor nuclei of the anterior horns of the spinal cord. It is located medial to the anterior corticospinal (pyramidal) tract. A bundle of these fibers is directly adjacent to the anterior median fissure. The presence of such a tract allows for reflexive protective movements to be performed during visual and auditory stimuli.
Between the anterior corticospinal (pyramidal) tract in front and the anterior gray commissure behind is the posterior longitudinal fascicle (fasciculus longitudinalis dorsalis, s. posterior). This fascicle extends from the brainstem to the upper segments of the spinal cord. The fibers of the fascicle conduct nerve impulses that coordinate, in particular, the work of the muscles of the eyeball and the muscles of the neck.
The vestibulospinal tract (tractus vestibulospinalis) is located on the border of the anterior funiculus with the lateral funiculus. This tract is localized in the superficial layers of the white matter of the anterior funiculus of the spinal cord, directly near its anterior lateral groove. The fibers of this tract go from the vestibular nuclei of the VIII pair of cranial nerves, located in the medulla oblongata, to the motor cells of the anterior horns of the spinal cord.
The lateral funiculus (funiculus lateralis) of the spinal cord contains the following conducting pathways:
1. The posterior spinocerebellar tract (tractus spinocerebellaris dorsalis, s. posterior, Flechsig's bundle) conducts impulses of proprioceptive sensitivity, occupies the posterolateral parts of the lateral funiculus near the posterior lateral groove. Medially, the bundle of fibers of this conducting pathway is adjacent to the lateral corticospinal and lateral spinothalamic tracts. Anteriorly, the bundles of the posterior spinocerebellar tract come into contact with the bundles of the anterior tract of the same name.
The anterior spinocerebellar tract (tractus spinocerebellaris ventralis, s. anterior, Gowers' bundle), which also carries proprioceptive impulses to the cerebellum, is located in the anterolateral parts of the lateral funiculus. Anteriorly, it adjoins the anterior lateral groove of the spinal cord and borders on the olivospinal tract. Medially, the anterior spinocerebellar tract is adjacent to the lateral spinothalamic and spinotegmental tracts.
The lateral spinothalamic tract (tractus spinothalamicus lateralis) is located in the anterior sections of the lateral funiculus, between the anterior and posterior spinocerebellar tracts - on the lateral side, and the rubrospinal and vestibulospinal tracts - on the medial side. Conducts impulses of pain and temperature sensitivity.
The descending systems of fibers of the lateral funiculus include the lateral corticospinal (pyramidal) and rubrospinal (extrapyramidal) conducting pathways.
- The lateral corticospinal (pyramidal) tract (tractus corticospinalis (pyramidalis) lateralis) conducts motor impulses from the cerebral cortex to the anterior horns of the spinal cord. A bundle of fibers of this tract, which are processes of giant pyramidal cells, lies medial to the posterior spinocerebellar tract and occupies a significant part of the area of the lateral funiculus, especially in the upper segments of the spinal cord. In the lower segments, it occupies an increasingly smaller area in sections. In front of this tract is the rubrospinal tract.
- The rubrospinal tract (tractus rubrospinalis) is located anterior to the lateral corticospinal (pyramidal) tract. Laterally to it, in a narrow section, are the posterior spinocerebellar tract (its anterior sections) and the lateral spinothalamic tract. The rubrospinal tract is a conductor of impulses of automatic (subconscious) control of movements and tone of skeletal muscles to the anterior horns of the spinal cord.
Bundles of nerve fibers also pass through the lateral funiculi of the spinal cord, forming other conduction pathways (for example, spinal-tegmental, olivospinal, etc.).
The posterior funiculus (funiculus dorsalis, s. posterior) at the level of the cervical and upper thoracic segments of the spinal cord is divided into two bundles by the posterior intermediate groove. The medial bundle is directly adjacent to the posterior longitudinal groove - this is a thin bundle (fasciculus gracilis, Goll's bundle). Lateral to it is the cuneate bundle (fasciculus cuneatus, Burdach's bundle), adjacent to the posterior horn on the medial side. The thin bundle consists of longer conductors that go from the lower parts of the trunk and lower limbs of the corresponding side to the medulla oblongata. It includes fibers that enter the posterior roots of the 19 lower segments of the spinal cord and occupy a more medial part of the posterior funiculus. Due to the entry of fibers belonging to neurons innervating the upper limbs and upper body into the 12 upper segments of the spinal cord, a wedge-shaped bundle is formed, occupying a lateral position in the posterior funiculus of the spinal cord. The thin and wedge-shaped bundles are bundles of proprioceptive sensitivity (joint-muscle sense), which carry information about the position of the body and its parts in space to the cerebral cortex.
In different parts of the spinal cord, the ratios of areas (on horizontal sections) occupied by gray and white matter are not the same. Thus, in the lower segments, in particular, in the area of the lumbar thickening, gray matter occupies a larger part on the section. Changes in the quantitative ratios of gray and white matter are explained by the fact that in the lower parts of the spinal cord, the number of fibers of the descending pathways following from the brain is significantly reduced, and the ascending pathways are only beginning to form. The number of fibers forming the ascending pathways gradually increases from the lower segments to the upper ones. On transverse sections of the middle thoracic and upper cervical segments of the spinal cord, the area of white matter is larger. In the area of the cervical and lumbar thickenings, the area occupied by gray matter is larger than in other parts of the spinal cord.
The spinal cord of a newborn is 14 cm (13.6-14.8 cm) long. The lower border of the brain is at the level of the lower edge of the second lumbar vertebra. By the age of two, the length of the spinal cord reaches 20 cm, and by the age of 10, it doubles compared to the neonatal period. The thoracic segments of the spinal cord grow most rapidly. The spinal cord of a newborn weighs about 5.5 g, in children aged 1 year - 10 g. By the age of 3, the spinal cord weighs more than 13 g, and at 7 years it is approximately 19 g.
In cross-section, the spinal cord looks the same as in an adult. In a newborn, the cervical and lumbar thickenings are well expressed, the central canal is wider than in an adult. The lumen of the central canal decreases mainly during the 1-2 years, as well as in later age periods, when the mass of gray and white matter increases. The volume of white matter increases faster, especially due to the proper bundles of the segmental apparatus, which is formed earlier than the conductive pathways connecting the spinal cord with the brain.
Blood vessels of the spinal cord. The spinal cord receives branches from the vertebral artery (from the subclavian artery), the deep cervical artery (from the costocervical trunk), and from the posterior intercostal lumbar and lateral sacral arteries. Three long longitudinal arterial vessels are adjacent to it: the anterior and two posterior spinal arteries.
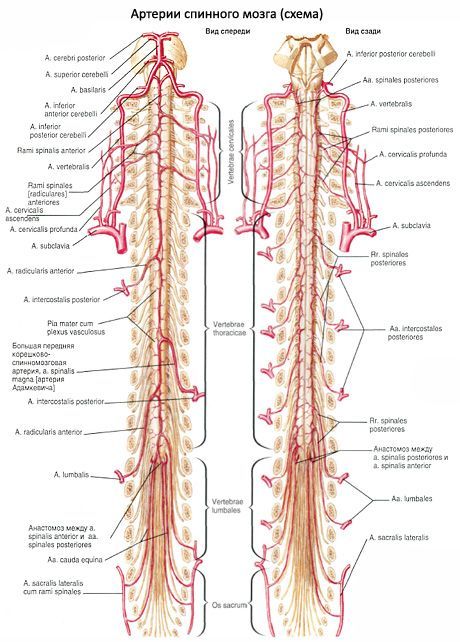
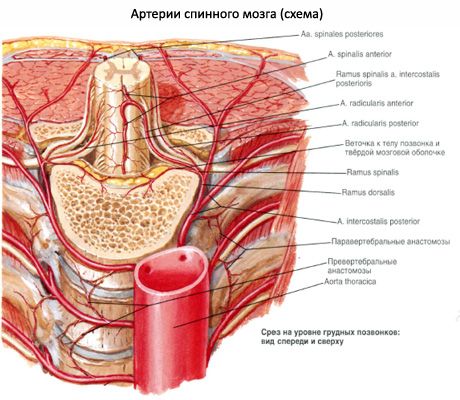

The anterior spinal artery (unpaired) adjoins the anterior longitudinal fissure of the spinal cord. It is formed from two arteries of the same name (branches of the right and left vertebral arteries) in the upper sections of the spinal cord. The posterior spinal artery is paired. Each of the arteries is adjacent to the posterior surface of the spinal cord near the entry of the posterior roots of the spinal nerves into the brain. These three arteries continue to the lower end of the spinal cord. The anterior and two posterior spinal arteries are connected to each other on the surface of the spinal cord by numerous anastomoses and with branches of the intercostal, lumbar and lateral sacral arteries, penetrating the spinal canal through the intervertebral openings and sending thin branches into the substance of the brain.
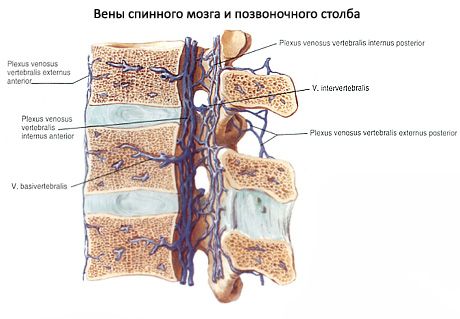
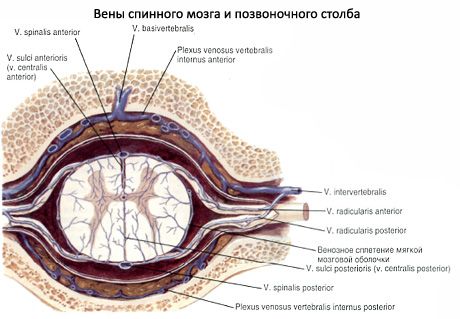
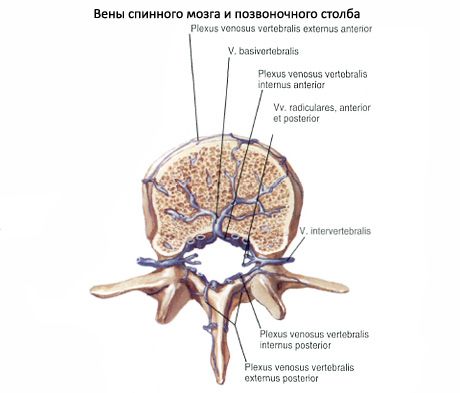
The veins of the spinal cord drain into the internal vertebral venous space.
 [ 1 ]
[ 1 ]
Where does it hurt?
What do need to examine?
What tests are needed?

