
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Hemopericardium of the heart
Medical expert of the article
Last reviewed: 12.07.2025
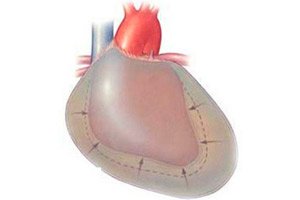
One of the adverse effects of acute myocardial infarction is hemopericardium, a dangerous and common condition that requires urgent medical intervention. The term "cardiac tamponade" is often used for this complication: hemopericardium is characterized by the accumulation of blood in the pericardial cavity, the so-called pericardial bursa, which consists of connective tissue.
The blood accumulated in the pericardium exerts a compressive effect, as a result of which it becomes difficult for the ventricles to perform their function. As a result, acute failure develops, shock and death occurs.
Epidemiology
According to statistics, hemopericardium occurs in two out of 10 thousand patients with the above risk factors.
After right ventricular endomyocardial biopsy, damage to the heart muscle occurs in 0.3-5% of patients, with hemopericardium developing in less than 50% of cases. The incidence of damage during left ventricular endomyocardial biopsy is estimated at 0.1-3%. Mortality after this procedure is no more than 0.05%.
After dissection of the ascending aortic section, hemopericardium is recorded in 17-45% of cases.
Causes hemopericardium
Blood accumulation in hemopericardium is observed not only as a result of a heart attack. Traumatic and non-traumatic causes of the development of pathology are distinguished. This allows us to divide the state of hemopericardium into separate types:
- traumatic hemopericardium – is a consequence of direct physical damage to the structures of the heart;
- non-traumatic hemopericardium – occurs as a result of other, indirect causes.
Trauma hemopericardium may occur:
- after severe chest trauma, chest or heart wounds;
- after any intracardiac manipulations ( puncture biopsy, injections, catheter insertion);
- after heart surgery (installation of a bypass graft, catheter ablation, mediastinotomy, poorly placed sutures, etc.);
- after performing sternal puncture.
Non-traumatic type of hemopericardium occurs:
- after left ventricular damage due to acute myocardial infarction;
- in case of rupture of pericardial and coronary vascular walls;
- in case of rupture of an aneurysm of the heart or aorta;
- as a result of rupture of cardiac tissue against the background of an abscess, myocardial echinococcosis, gummatous inflammation of the myocardium;
- for heart tumors;
- in case of increased bleeding due to hemorrhagic diathesis or hemophilia;
- after tuberculous, purulent or idiopathic inflammation of the pericardium;
- during hemodialysis against the background of insufficient renal function;
- for autoimmune diseases with damage to connective tissue.
Risk factors
Any person can injure the chest under various circumstances. The injury can be caused by a direct wound (both knife and gunshot), a bruise from a fall from a height, or chest compression. Emergencies that can lead to the development of hemopericardium include:
- natural disasters earthquakes, floods, avalanches, landslides;
- road traffic accidents.
People who have certain problems with the heart and nervous system are also at risk. Hemopericardium is often caused by rupture of the vascular walls, acute myocardial infarction, myocarditis.
Other risk factors also include:
Pathogenesis
The pericardial cavity, or pericardial bursa, is formed from the parietal and visceral pericardial membranes. Between these membranes there remains a cavity that consists of separate sections (they are also called sinuses):
- anterior inferior sinus;
- transverse sinus;
- oblique sinus.
If a hemopericardium condition develops, then blood begins to accumulate inside the anterior inferior section, located in the middle of the diaphragmatic and sternocostal pericardial region.
Symptoms hemopericardium
Clinical symptoms of hemopericardium may vary or not appear at all: it depends on how much blood is in the pericardial cavity. If the blood volume is insignificant, then symptoms may be absent.
Hemopericardium becomes obvious if the amount of blood entering the pericardial cavity is more than 150 ml. With such a volume, the heart experiences increased pressure, blood circulation in it is disrupted, and cardiac output decreases. In addition, arterial vessels that deliver blood to the myocardium can be compressed.
The first signs of hemopericardium development are conventionally divided into two categories – subjective and objective. Subjective signs include:
- difficulty breathing;
- a feeling of anxiety and fear;
- nausea, general weakness;
- increased sweating.
Objective signs are:
- tachycardia;
- hypotension;
- weakening of the pulse;
- bluish skin;
- disorder of consciousness.
Often, when listening, it is difficult to determine the heartbeat.
In addition, the patient may complain of pain behind the breastbone and a feeling of internal pressure in the chest. Swelling of the jugular veins is visually observed.
If a large volume of blood (more than 0.5 l) accumulates in the pericardial cavity, cardiac arrest and death are possible. To prevent this, the patient must be provided with qualified assistance as a matter of urgency.
Hemopericardium in acute myocardial infarction occurs against the background of damage to the wall of the left ventricle - in the transmural form of infarction. In the case of a rupture of the heart or aorta, critical hemodynamic disorders occur within a few seconds, turning into sudden clinical death.
Iatrogenic hemopericardium is frequently observed after percutaneous mitral valvuloplasty or transseptal puncture.
When the ventricles are damaged, symptoms develop rapidly, while when the atria are damaged, clinical signs may not appear until approximately 5 hours later.
Complications and consequences
With a significant volume of blood spilled into the pericardial sac, terminal circulatory disorders and sudden clinical death may occur. In this case, measures to provide resuscitation assistance most often become ineffective, since the amount of blood inside the pericardium can be 400-500 ml.
In cases where a rupture of the heart or aortic vessel occurs in a hospital, it is possible to establish a fatal outcome and its cause with a high degree of probability: electrocardiography records a sinus rhythm for a certain period of time. In some situations, with layered damage to the aneurysm, a couple of hours or several days may pass from the moment of the first symptoms until the patient's death.
Myocardial penetration is possible in the presence of an artificial pacemaker located in the right ventricle. One of the first symptoms is the occurrence of a right bundle branch block.
Diagnostics hemopericardium
In addition to examining the patient, auscultatory listening to the characteristics of cardiac activity and tapping the cardiac borders, additional types of research are used to diagnose hemopericardium.
Blood tests are performed to assess the coagulation function and to determine the presence of an inflammatory process.
Urine analysis is necessary to assess kidney function.
Instrumental diagnostics usually consists of the following procedures:
- Electrocardiography: Typically shows a pattern consistent with pericardial effusion or tall, peaked T waves in the chest leads.
- X-ray diagnostics indicate:
- to increase the volume of the organ;
- on smoothed cardiac arcs;
- to a reduced pulsation amplitude, or its absence.
The X-ray must be performed dynamically: this will allow us to determine the rate of blood accumulation in the pericardial sac.
- The echocardiography method demonstrates the following pathological changes:
- with a small hemopericardium, a relatively free echo lumen is visualized in the space between the posterior portion of the pericardium and the posterior portion of the left ventricular epicardium;
- with significant hemopericardium, this lumen is localized between the anterior portion of the right ventricular pericardium and the parietal portion of the pericardium below the anterior chest wall;
- In severe hemopericardium, the heart often oscillates in the pericardial cavity: sometimes such oscillation can lead to a disorder of the electrical functionality of the organ.
- The angiocardiography method involves the introduction of contrast into the cavity of the right atrium. This allows one to examine the separation of the lateral wall from the border of the heart silhouette.
Differential diagnosis
Differential diagnosis of hemopericardium is carried out with such pathological conditions as exudative pericarditis, hydropericardium, as well as with other hemopericarditis of non-inflammatory etiology.
Who to contact?
Treatment hemopericardium
With a small accumulation of blood in the pericardial bursa, the patient is prescribed medication, with mandatory bed rest, and is also provided with rest and a complete balanced diet. At first, a cold compress is applied to the chest area.
If necessary, in case of hemopericardium, the doctor prescribes hemostatic therapy and medications to support the functionality of the cardiovascular system.
Some patients may be prescribed anti-inflammatory and antibacterial drugs (if an infectious component of the pathology is diagnosed).
During the entire course of treatment, hemodynamic parameters must be monitored. If the patient's condition is assessed as stable, then subsequent treatment tactics should be aimed at eliminating the cause of hemopericardium.
If blood continues to accumulate in the pericardial sac, the doctor decides to stop drug treatment and begin surgical intervention.
Medicines that can be used for hemopericardium
To relieve pain, the patient is given 1 ml of 1% morphine, 2 ml of 2% promedol, 2 ml of 2% pantopon as a subcutaneous or intravenous injection.
An anesthetic mixture is administered intravenously, and nitrous oxide and oxygen are inhaled.
In no case should drugs that can lower blood pressure (for example, chlorpromazine) or heparin-based medications, which increase bleeding, be administered in the case of hemopericardium.
After performing a pericardial puncture, if necessary, an antibiotic is administered through the needle - for example, penicillin 300,000 IU.
After the puncture, the doctor prescribes anti-inflammatory therapy, using corticosteroids and non-steroidal anti-inflammatory drugs. Intrapericardial administration of corticosteroids is considered more effective and helps to avoid side effects that are possible with systemic use of these drugs.
With a gradual reduction in the dosage of prednisolone, ibuprofen or colchicine is administered as early as possible, in individual dosages.
The recommended dose of colchicine may be 2 mg per day for 1-2 days, then 1 mg per day.
The recommended dose of prednisolone is 1-1.5 mg/kg for 4 weeks. Treatment with corticosteroids is stopped gradually, slowly reducing the dosage.
The selection of hemostatic drugs and their dosage are performed strictly individually, depending on the cause and characteristics of the course of hemopericardium.
Vitamins
What vitamins does the heart need after hemopericardium? How to ease cardiac function?
- Vitamin E is a powerful antioxidant that strengthens vascular walls.
- B vitamins – normalize metabolic processes and cholesterol levels.
- Omega-3 acids – prevent the development of atherosclerosis, improve the elasticity of blood vessels.
- Coenzyme Q 10 – improves cellular metabolism and respiration, optimizes myocardial contractility, accelerates energy metabolism.
After hemopericardium, special attention should be paid to nutrition. It should be complete and at the same time low-calorie, because getting rid of extra pounds will reduce the load on the heart. It is useful to enrich the diet with such foods as fish, beans, olive oil, vegetables and fruits.
Physiotherapy treatment
Physiotherapy and massage are the main procedures for the recovery of patients after hemopericardium. Moderate and properly selected physical activity will strengthen the myocardium and coronary vessels, as well as prevent the likelihood of recurrent pathology.
At first, slow walking along the corridor is allowed for a quarter of an hour. At the same time, the doctor must measure the pulse rate and blood pressure.
Little by little, walking is supplemented with climbing and descending stairs, as well as simple gymnastic movements and massage. If chest pain, shortness of breath and instability of pressure occur, the exercises are made less intense.
After the patient is discharged from the hospital, the exercises continue, gradually increasing the load. It is important to understand that the myocardium needs regular training. The exception is the presence of an aneurysm. Loads in this case are contraindicated.
Folk remedies
Traditional medicine often helps even in very severe cases. However, in case of hemopericardium, traditional recipes can be used only at the recovery stage, and only after consulting a doctor - traditional medicine will not replace a puncture.
To regenerate damaged tissues after a state of hemopericardium and to improve heart function, traditional healers offer the following popular recipes:
- A medicinal gruel is prepared from equal parts of ground walnut kernels and honey. To prevent complications, you need to eat 50-70 g of this mass every day.
- Mix 100 ml of aloe tree juice and 200 ml of linden honey, add 200 ml of quality Cahors wine. Take 1 teaspoon of the resulting remedy before each meal.
- The lemon is peeled and minced together with the peel. The resulting mass is then mixed with crushed apricot kernels, ground pelargonium and honey (0.5 l). The remedy is consumed up to 4 times a day, 1 tbsp before meals.
- Two parts of anise seeds are mixed with one part of ground valerian root, one part of crushed yarrow and lemon balm leaves. One tablespoon of the mixture is poured with 200 ml of boiling water and infused for half an hour. The resulting remedy is drunk two or three times.
 [ 41 ], [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ], [ 48 ]
[ 41 ], [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ], [ 48 ]
Herbal treatment
In hemopericardium, it is very important to properly support cardiac function and strengthen the body's resistance. Medicinal plants will be an excellent means for these purposes.
- The juice from the thick leaves of coltsfoot should be drunk at least four times a day, 1-2 tablespoons. Healers claim that even one course of treatment per year is enough to strengthen the body. On average, such a course can last 1-2 weeks.
- To prevent complications from the heart, prepare a balanced mixture of such plants as coltsfoot, linden blossom, willow bark, raspberry and anise. One tablespoon of the dry mixture is brewed in 400 ml of boiling water, infused in a thermos for about half an hour, then filtered and drunk instead of tea, at any time of the day.
- Mix equal amounts of horsetail, black elderberry blossom and marshmallow root. Brew overnight in a thermos at a rate of 2 tbsp. of the mixture per 500 ml of boiling water. Take 100 ml of the infusion 2-3 times a day.
- Prepare a mixture of one part chamomile flowers, three parts hawthorn flowers, motherwort and immortelle. Pour 1 tbsp of the mixture with 400 ml of boiling water and leave for eight hours. Take 100 ml 3-4 times a day between meals.
Homeopathy
Homeopathic doctors recommend using homeopathic treatment for almost any disease that does not require emergency surgical intervention. Hemopericardium is a serious and dangerous condition in which it is absolutely impossible to rely on homeopathy alone: urgent intervention and emergency medical care are necessary.
At the stage of recovery after hemopericardium, against the background of drug treatment, it is allowed to take individual homeopathic preparations, at the discretion of the doctor. For example, it is possible to use the following homeopathic remedies:
- Purpose: prescribed for the restoration of soft tissues, one tablet three times a day.
- Traumeel - take one tablet three times a day, for a long period of time (at the discretion of the doctor).
- Nux vomica-homaccord - take 30 drops per day in 100 ml of water, 15-20 minutes before meals.
- Berberis gommacord - take 10 drops three times a day, 15-20 minutes before meals, with water.
- Belladonna gommacord - take 10 drops 3 times a day, 15 minutes before meals.
Homeopathic medicines can in rare cases cause allergic reactions: this should be taken into account if the medicine is being taken for the first time.
Surgical treatment
If the heart or vascular walls are damaged, an emergency operation is performed to eliminate the underlying cause of blood leaking into the pericardium. This is a thoracotomy operation and suturing of damaged tissues.
The type and nature of surgery for hemopericardium is determined by the doctor, depending on the complexity of the damage.
With rapid development of hemopericardium, it is necessary to urgently eliminate excess pressure on the heart and remove the spilled blood. For this purpose, the following is performed:
- pericardial puncture ( pericardiocentesis operation ), when an aspiration needle is inserted into the pericardium and the spilled blood is sucked out;
- surgical drainage of the pericardial sac (a puncture is performed and a drainage catheter is installed in the area of maximum blood accumulation);
- percutaneous balloon pericardiotomy (a special balloon is inserted into the pericardial sac, providing a window for the removal of blood).
Minimally invasive surgeries are performed under ECG and echocardiography monitoring, with mandatory background monitoring of hemodynamic function.
In case of significant blood loss, the patient may be prescribed oxygen therapy, plasma substitutes and other solutions to restore homeostatic balance.
After stopping the flow of blood into the pericardium, therapy is carried out for the underlying cause of hemopericardium.
Prevention
Prevention of hemopericardium consists of warning and avoiding situations that can cause the development of hemopericardium:
- preventing injuries to the chest area;
- prevention of cardiovascular diseases, blood diseases;
- prevention and timely treatment of infectious diseases.
It is necessary to undergo regular medical examinations, including a cardiologist, and also to contact a doctor in a timely manner at the slightest sign of deterioration in health.
Forecast
The prognosis of hemopericardium depends mainly on the amount of blood in the pericardial cavity, as well as on how quickly tamponade occurs and how promptly medical care was provided.
In the chronic form of the disease, it is important to properly treat the underlying cause of hemopericardium: this will stop further release of blood into the pericardial bursa.
Acute hemopericardium has the most negative prognosis: if 400 ml or more of blood accumulates in the cavity, the patient dies.
Timely surgical intervention increases the probability of a favorable outcome. Statistics confirm: if the puncture is performed on time, the patient's chances of survival increase by 95-100%. Therefore, it is very important not to hesitate at the slightest suspicion of hemopericardium.

