Puncture of pericardium, pericardiocentesis: methods of carrying out, complications
Cardiosurgery is an area of medicine that allows you to regulate the work of the heart through surgical intervention. In its arsenal, there are many different operations on the heart. Some of them are considered quite traumatic and are conducted for therapeutic purposes on acute indicators. But there are also such types of cardiac operations as puncture of the pericardium, which do not require opening of the sternum and penetration into the heart cavity. This rather informative mini-operation can be carried out both for medical and diagnostic purposes. And, despite all the seeming simplicity of execution, can even save a person's life.
Indications for the procedure
Puncture of the pericardium (pericardiocentesis) is an operation, the essence of which is to remove the exudate from the pericardial sac. It should be understood that some liquid is constantly in the pericardial cavity, but this is a physiologically conditioned phenomenon that does not have a negative effect on the heart. Problems arise if the liquid is recruited more than usual.
The operation for pumping the fluid from the pericardial sac is performed only if preliminary diagnostic studies confirm the presence of effusion in it. The presence of a large amount of exudate can be observed in the inflammatory process in the pericardium (pericarditis), which in turn can be exudative or purulent if a bacterial infection is attached. With such a type of pathology as hemopericardium, there is a significant amount of blood cells in the exudate and the pumped out liquid has a red color.
But pericarditis also does not arise by itself. An effusion to the pericardial cavity can provoke both cardiac pathologies, for example, myocardial infarction, and diseases not associated with the cardiovascular system. Such diseases include: renal failure, rheumatoid arthritis, tuberculosis, collagenosis, uremia. A similar situation physicians sometimes observe in autoimmune and oncological pathologies. In addition, the presence of purulent exudate in the pericardium can be associated with the presence in the patient's body of a bacterial infection.
Some readers may have a fair question, why pumped the fluid out of the pericardium, if its presence there is considered to be a physiologically conditioned phenomenon? A small amount of liquid can not interfere with the work of the heart, but if its volume increases rapidly, creating pressure on the vital organ, it becomes harder for it to cope with its functions, developing a cardiac tamponade.
Cardiac tamponade refers to the state of cardiogenic shock that occurs if the pressure in the pericardial cavity becomes higher than the blood pressure in the right atrium, and during diastole and in the ventricle. The heart is squeezed and becomes unable to provide adequate discharge of blood. This leads to a marked violation of blood circulation.
If the effusion in the pericardium forms slowly, then gradually a large amount of exudate accumulates in the pericardium, which again can provoke a cardiac tamponade. In this case, excessive squeezing of the heart with a large volume of fluid can lead to a critical decrease in blood flow, which requires immediate intervention to save the patient's life.
In all the cases described above, pericardial puncture is performed to prevent (planned) or treat (emergency) cardiac tamponades. But this procedure has a high diagnostic value, so it can be appointed to identify the nature of exudate in case of suspected pericarditis, which, as we already know, can have various forms.
Preparation
No matter how easy the procedure of pumping out fluid from the pericardial cavity seemed, it can be carried out only after a serious diagnostic study of the heart, including:
- Physical examination of a cardiologist (examination of anamnesis and patient complaints, listening to tones and noises in the heart, tapping its boundaries, measuring blood pressure and pulse).
- The delivery of a blood test, which allows you to identify the inflammatory process in the body and determine the indicators of blood coagulability.
- Carrying out electrocardiography. In case of impaired pericardial effusion, certain changes will be seen on the electrocardiogram: signs of sinus tachycardia, change in the height of the R wave, indicating a displacement of the heart inside the pericardium sac, low voltage due to a decrease in the electric current after passing through the fluid accumulated in the pericardium or pleura.
- In addition, central venous pressure can be measured, which is increased with pericarditis with a large effusion.
- Assignment of chest radiograph. On the X-ray film, the enlarged silhouette of the heart, having rounded forms and an enlarged caudal vena cava, will be clearly visible.
- Echocardiography. It is performed on the eve of the operation and helps to clarify the cause of the impaired effusion, for example, the presence of a malignant neoplasm or a rupture of the left atrial wall.
Only after the diagnosis of pericarditis has been confirmed or the accumulation of exudate in the pericardial cavity is detected, an emergency or planned operation is made to take fluid from the pericardial sac for the purpose of studying it or facilitating the work of the heart. The results of instrumental studies allow the doctor to chart the expected points of pericardial puncture and to determine the actual methods of performing the operation.
During physical examination and communication with the attending physician, you must tell him about all medications taken, especially those that can reduce blood clotting (acetylsalicylic acid and other anticoagulants, some anti-inflammatory drugs). Usually within a week before the operation, doctors are forbidden to take such medications.
At a diabetes it is necessary to consult necessarily in occasion of reception sugarosnizhajushchih medicamentous agents before carrying out a puncture of a pericardium.
This is about medicines, now let's talk about nutrition. The operation should be performed on an empty stomach, therefore the use of food and even water will have to be limited in advance, which the doctor will warn at the stage of preparation for surgery.
Even before the beginning of the operation, the medical staff should prepare all the necessary medicines used during this procedure:
- antiseptics for the treatment of the skin in the puncture area (iodine, chlorhexidine, alcohol),
- antibiotics for insertion into the pericardial cavity after removal of purulent exudate (with purulent pericarditis),
- anesthetics for local injection anesthesia (usually, lidocaine 1-2% or novocaine 0.5%),
- sedatives for intravenous administration (fentanyl, midazolam, etc.).
Puncture of the pericardium is carried out in a specially equipped room (operating room, manipulation room), which must be equipped with all the necessary tools and materials:
- A specially prepared table where you can find all the necessary medicines, a scalpel, a surgical thread, syringes with needles for the introduction of anesthesia and pericardiocentesis (a 20-cc syringe with a needle 10-15 cm long and about 1.5 mm in diameter).
- Sterile clean supplies: towels, napkins, gauze swabs, gloves, bathrobes.
- Expander, sterile clamps, tube for exudation (with a large volume of liquid, if it will be removed naturally), a drainage bag with adapters, a large catheter, a conductor made in the form of a letter "J".
- Special equipment for monitoring the patient's condition (electrocardiomonitor).
In the office, everything should be prepared for emergency resuscitation, but the operation is performed on the heart and complications are always possible.
Technique of the puncture of the pericardium
After the preparatory part of the procedure is completed, proceed directly to the operation. The patient is located on the operating table reclining on the back, i.e. The upper part of his body is raised relative to the plane by 30-35 degrees. This is necessary to ensure that the accumulated fluid during manipulation was in the lower part of the cavity of the pericardial sac. Puncture of the pericardium can be carried out and in a sitting position, but it is less convenient.
If the patient is visibly nervous, he is administered sedatives, most often through a venous catheter. The thing is that the operation is conducted under local anesthesia, and the person is conscious all this time, and therefore, can see what is happening to him and react inadequately.
Further, the skin is disinfected in the area of the puncture (the lower part of the thorax and the ribs on the left side) with an antiseptic. The rest of the body is covered with clean linen. The place of introduction of the needle (skin and subcutaneous layer) is cut with an anesthetic.
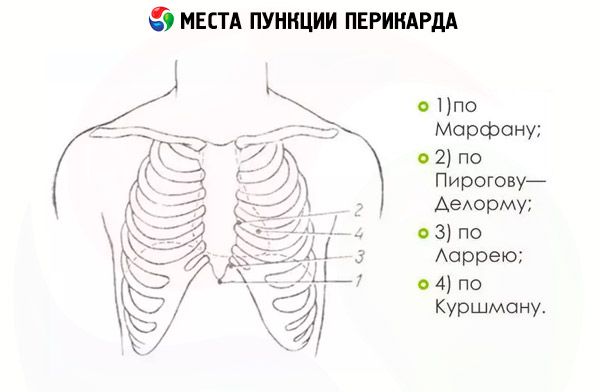
The operation can be carried out in several ways. They differ in the place of insertion of the needle and its movement until reaching the pericardial wall. For example, according to the Pirogov-Karavaev method, the needle is inserted into the region of the 4 intercostal spaces on the left side. Puncture points of the pericardium are located 2 cm laterally from the sternum.
According to the Delorme-Mignon method, the puncture should be located on the left side of the sternum between the 5th and 6th ribs, and the pericardial puncture points according to the Shaposhnikov method near the right edge of the sternum between the 3rd and 4th rib.
The most common because of their low traumaticity are the methods of Larry and Marfan. When using them, the risk of damage to the pleura, heart, lungs or stomach is minimal.
Puncture of the pericardium according to Laruey implies puncture of the skin near the xiphoid process on the left side in the place where the cartilages of the VII rib adjoin to it (the lower part of the xiphoid process). First, the puncture needle is inserted perpendicular to the body surface by 1.5-2 cm, then it sharply changes direction and goes parallel to the plane in which the patient lies. After 2-4 cm it rests against the pericardial wall, the puncture of which is carried out with a noticeable effort.
Further, there is a feeling of movement of the needle in the void (resistance is practically absent). This means that it penetrated the pericardial cavity. By pulling the plunger of the syringe onto yourself, you can see the liquid entering into it. For a diagnostic sampling of exudate or pumping out a small amount of liquid, a 10-20-cc syringe is sufficient.
Puncture must be done very slowly. The movement of the needle inside the body is accompanied by the injection of an anesthetic every 1-2 mm. When the syringe needle has reached the pericardial cavity, a small dose of anesthetic is injected additionally, and then proceed to aspiration (pumping out the exudate).
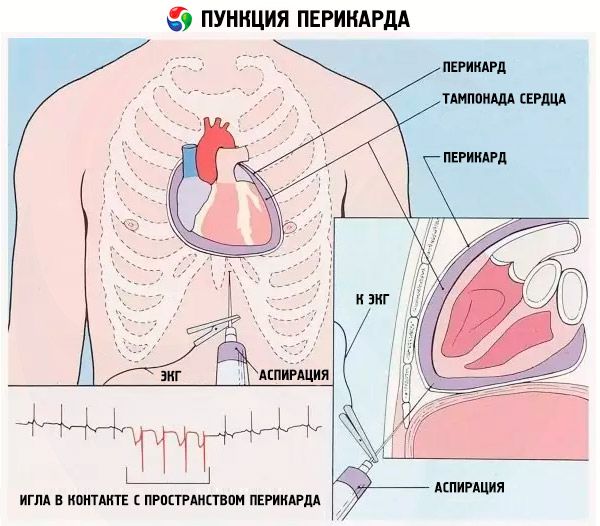
The movement of the needle is monitored on the monitor by means of a special electrode attached to it. However, doctors prefer to rely on their feelings and experience, because passing the needle through the pericardial wall does not go unnoticed.
If there is a rhythmic twitching of the syringe, the needle may rest on the heart. In this case, it is slightly retracted and press the syringe closer to the sternum. After this, you can safely proceed to remove effusion from the pericardial bag.
If pericardial puncture is performed for therapeutic purposes with suspicion of purulent pericarditis, after pumping out the effusion, the pericardial cavity is treated with an antiseptic, in an amount not exceeding the amount of pumped out exudate, and then oxygen and an effective antibiotic are introduced into it.
Puncture of the pericardium in the ambulance stage can be carried out in conditions where there is a large amount of exudate presenting a danger to the life of the patient. One syringe is indispensable here. After removal of the needle from the body, a conductor is left in it, an expander is inserted into the injection hole and a catheter with clamps is inserted along the conductor, to which the drainage system joins. Through this design, fluid is subsequently removed from the pericardial cavity.
The catheter is tightly attached to the patient's body at the end of the operation and is left for a certain period of time during which the patient will be in a medical facility under the supervision of a doctor. If the liquid is pumped out by a syringe, then at the end of the procedure, after removing the needle from the body, the puncture site is briefly pressed and glued with medical glue.
Puncture of the pericardium according to Marfan is carried out in a similar way. Only the needle for the pericardiocentesis is inserted obliquely under the tip of the xiphoid process and moves in the direction of the posterior sternum. When the needle abuts against the pericardial leaf, the syringe is slightly removed from the skin and pierced by the organ wall.
The duration of the procedure for draining the fluid from the pericardial sac can vary from 20 minutes to 1 hour. Exudate is poured a little, giving the heart the opportunity to get used to pressure changes outside and inside. The depth of penetration depends to a large extent on the patient's constitution. For thin people, this figure varies within 5-7 cm, in full depending on the thickness of the subcutaneous fat layer can reach 9-12 cm.
Contraindications to the procedure
Despite the fact that puncture of the pericardium is serious and to some extent a dangerous operation, it is carried out at any age. The period of newborn is not an exception, if there is no other way to restore coronary blood flow in a baby whose pericardium accumulates liquid.
Age restrictions have no operation. As for health restrictions, there are no absolute contraindications. If possible, try to avoid such surgery with poor blood coagulability (coagulopathy), central aortic dissection, and low platelet count. However, if there is a risk of serious impairment of blood circulation, doctors still resort to puncture treatment.
Puncture of the pericardium is not performed if the disease is not accompanied by a large effusion or rapid filling of the pericardium with secreted exudate. You can not perform a puncture in the event that after the procedure there is a high risk of cardiac tamponade.
There are certain situations that require special care when performing a puncture. Very carefully carry out the excretion of bacterial exudate from the pericardial cavity with purulent pericarditis, with efflorescence associated with oncological pathologies, in the treatment of hemopericardia, which develops as a result of injury or injury to the chest and heart. There may be complications during the operation and in patients with thrombocytopenia (due to a low concentration of platelets, the blood does not fold well, which can lead to bleeding during surgical procedures), as well as those who, shortly before the operation, took anticoagulants (drugs that dilute blood and slowing down its coagulation).
Consequences after the procedure
Puncture of the pericardium is a cardiosurgical procedure, which, like any other operation on the heart, has certain risks. The unprofessionalism of the surgeon, ignorance of the technique of surgical intervention, the violation of the sterility of the instruments used can lead to disruption of the work not only of the heart, but also of the lungs, pleura, liver, and stomach.
Since all manipulations are carried out using an acute needle that, when moving, can damage nearby organs, it is important not only to be careful of the surgeon, but also to know the ways in which the needle can freely enter the pericardial cavity. Still, the operation is carried out almost blindly. The only possibility to monitor the situation remains monitoring with the help of ECG and ultrasound devices.
The doctor should try not only to strictly follow the technique, but also to display incredible accuracy. Trying to force through the pericardial wall, you can overdo it and rest the needle in the heart shell, damaging it. This can not be allowed. Feeling the pulse of the heart through the twitching of the syringe, you must immediately take the needle back, putting it slightly obliquely into the cavity with exudate.
Before the operation, a thorough examination of the boundaries of the heart and its work is mandatory. Puncture should be done in the place where there is a large accumulation of exudate, with aspiration, the rest of the intracavitary fluid will be tightened to it.
Important and responsible approach to the choice of the method of puncture of the pericardium bag. Larry's method, although it is preferable in most cases, however, with some deformations of the chest, greatly enlarged liver, pericarditis, it is worthwhile to think about other methods of pericardial puncture, which will not have unpleasant consequences in the form of damage to the vital organs or incomplete excretion .
If the operation is performed in accordance with all the requirements of an experienced surgeon, the only consequence of this procedure will be the normalization of the heart's work due to the reduction of pressure on it pericardial fluid and the possibility of further effective treatment of the existing pathology.
Complications after the procedure
In principle, all possible complications that develop in the days after the operation, have their origin even during the procedure. For example, damage to the cardiac myocardium or large coronary arteries can lead to cardiac arrest, which requires urgent intervention by resuscitators and appropriate treatment in the future.
Most often, the right ventricle chamber is damaged by the needle, which can provoke, if not cardiac arrest, ventricular arrhythmias. Violation of the heart rhythm can occur during the movement of the conductor, which will be reflected on the cardiac monitor. In this case, doctors deal with atrial arrhythmia, which requires immediate stabilization of the condition (for example, the administration of antiarrhythmic drugs).
A sharp needle in careless hands along the path of motion can damage the pleura or lungs, thereby triggering pneumothorax. Now the accumulation of fluid can be observed in the pleural cavity, which will require identical drainage measures (pumping out fluid) in this area.
Sometimes when pumping out the liquid, its color is found red. It can be both exudate with hemopericardium, and blood as a result of damage to the needle of epicardial vessels. It is very important to determine the nature of the pumped liquid as soon as possible. In the case of vascular damage, the blood in the exudate still quickly folds when placed in clean dishes, while hemorrhagic exudates lose this ability even in the pericardial cavity.
Other vital organs may also undergo needle penetration: the liver, stomach and some other abdominal organs, which is a very dangerous complication that can lead to internal bleeding or peritonitis, requiring urgent measures to save the patient's life.
Perhaps not so dangerous, but still an unpleasant consequence after the procedure of puncture of the pericardium is infection of the wound or infection in the pericardial sac cavity, which leads to the development of inflammatory processes in the body, and sometimes can even become a cause of blood infection.
Avoid possible complications if strictly adhere to the method of puncture treatment (or diagnosis), carry out all the necessary diagnostic tests, act confidently, but carefully, without haste, fuss and sudden movements, to comply with the requirements of absolute sterility during the operation.
Care after the procedure
Even if at first glance it seems that the operation was carried out successfully, it is impossible to exclude the possibility of hidden damages, which subsequently remind themselves of big troubles, both for the patient and for the doctor who performed the surgical intervention. In order to exclude such situations, as well as if necessary, in time to provide emergency care to the patient, after the procedure, an X-ray examination is mandatory.
In a medical facility, the patient may stay for several days or even weeks after the procedure. If it was a diagnostic procedure that went without complications, the patient can leave the hospital the next day.
In case of complications, as well as the installation of a catheter, which will drain the fluid even after the operation, the patient will be discharged only after his condition is stabilized and the need for drainage disappears. And even in this case, experienced doctors prefer to be reinsured by conducting an additional ECG, a computer tomography or an MRI. Conducting tomography is also indicative for revealing neoplasms on the pericardial walls and assessing the thickness of its walls.
During recovery from pericardial puncture, the patient is under the control of the attending physician and junior medical staff, who regularly measures the pulse, blood pressure, monitors the breathing characteristics of the patient, in time to detect possible abnormalities that were not detected by the radiograph.
And even after the patient leaves the clinic, at the insistence of the attending physician, he must adhere to certain preventive measures preventing complications. We are talking about the revision of the regime and diet, the rejection of bad habits, the development of the ability to rationally respond to stressful situations.
If the puncture of the pericardium has therapeutic purposes, the patient may stay in the clinic until the end of all medical procedures that can be performed only in a hospital. Conducting a mini-operation for diagnostic purposes will give the doctor the direction of further treatment of the patient, which can be carried out both in a hospital and at home, depending on the diagnosis and condition of the patient.
Last reviewed: 25.06.2018
