
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Enterovirus meningitis in children and adults
Medical expert of the article
Last reviewed: 12.07.2025
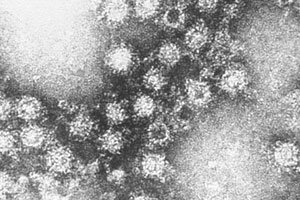
When inflammation of the pia mater of the brain is caused by enteroviruses of the Picornaviridae family, the diagnosis is enteroviral meningitis. The ICD-10 code for this disease is A87.0 under infectious diseases (and G02.0 under inflammatory diseases of the central nervous system). Enteroviruses include coxsackieviruses A and B, echoviruses, polioviruses, and recently identified viruses designated by numbers, such as enterovirus 71.
Epidemiology
Picornaviruses, particularly the enterovirus and rhinovirus groups, are responsible for the majority of human viral diseases. Enteroviruses cause 10 to 15 million symptomatic infections each year in the United States. [ 1 ]
Overall, the incidence of viral meningitis in the general population per year is estimated at five cases per 100,000 population.
The exact etiology of viral meningitis (i.e. the specific serotype of the virus) is identified in no more than 70% of cases. [ 2 ]
Enteroviruses are considered the most common cause of viral meningitis in many countries worldwide, with 12 to 19 cases per 100,000 population reported annually in some high-income countries.[ 3 ]
Causes enteroviral meningitis.
Research has shown that up to 85-90% of all cases of viral meningitis, [ 4 ] which is also called aseptic meningitis, [ 5 ] is associated with damage to the pia mater and arachnoid membrane and the subarachnoid space of the brain by enterovirus infections, the spread of which is seasonal and increases significantly in the summer. [ 6 ]
The causes are infection with Coxsackie viruses or ECHO (Enteric Cytopatthogenic Human Orphan) viruses, which can occur in two ways: feco-oral (through water, food, hands or objects contaminated with these viruses) and airborne (through contact with sick or recovering people whose respiratory aerosol contains the virus). [ 7 ]
Risk factors
Poor hygiene, children under three years of age, and weakened immunity in adolescents and adults are considered risk factors for the development of enterovirus meningitis.
Enteroviruses, which cause most cases of viral meningitis, are contagious, but many cases are asymptomatic or present with fevers other than meningitis.
Pathogenesis
It is clear that the pathogenesis of enterovirus inflammation of the meninges is caused by the action of viruses that have penetrated the body. The mechanism of the inflammatory process induced by these Coxsackie viruses and the ECHO virus is not completely clear. [ 8 ], [ 9 ]
It is known that their capsid proteins – before the start of genome replication – interact with certain receptors of cellular (lysosomal) membranes in many human tissues and cell types, including T-lymphocytes and neurons, which is essentially the first stage of the virus’s life cycle. [ 10 ]
Initially, viral replication occurs in the lymphatic tissues of the upper respiratory tract and small intestine, and then they spread by entering the blood (i.e., after secondary viremia). [ 11 ]
More information in the material - Enterovirus infections - Causes and pathogenesis
Symptoms enteroviral meningitis.
The first signs of viral (aseptic) meningitis caused by enteroviruses usually manifest as acute fever (above +38.5°C), [ 12 ] headache, photophobia, neck stiffness (stiffness of the occipital muscles), nausea and vomiting. [ 13 ]
Symptoms also include signs of meningeal irritation: involuntary contraction of the popliteal tendon when extending the knee joint in a patient lying on his back (Kernig's sign); involuntary bending of the legs and pulling them up to the stomach when trying to tilt the patient's head forward (Brudzinski's sign). [ 14 ]
With this infection of the meninges, infants experience increased irritability and capriciousness, complete lack of appetite and refusal to breastfeed, increased drowsiness, and vomiting. Although enterovirus meningitis in young children may occur without pronounced meningeal signs.
The younger the child, the faster the damage to the tissue of the meninges can occur and the inflammatory response can develop – fulminant enterovirus meningitis with the same symptoms or only with weakness and headache. In rare cases, clouding of consciousness and stupor are possible. [ 15 ]
Neonates with enteroviral meningitis may present similarly to bacterial sepsis and may also have systemic involvement such as liver necrosis, myocarditis, necrotizing enterocolitis, seizures, or focal neurologic signs.
Also read – Symptoms of Coxsackie and ECHO infections
Complications and consequences
The main complications of enterovirus meningitis are the development of meningoencephalitis and cerebral edema. Although most types of aseptic meningitis do not cause serious consequences, long-term consequences may include neuromuscular disorders, headache attacks, and short-term memory impairment.
Some enterovirus subtypes, such as EV71 and EV68, are associated with more severe neurologic disease and worse outcomes. The most common severe complications of enteroviral meningitis are meningoencephalitis, myocarditis, and pericarditis. In children, neurologic complications of enterovirus infection may include acute flaccid paralysis and rhombencephalitis. Neuropsychological impairment following viral meningitis is measurable but is generally not as severe as that following bacterial meningitis.[ 16 ] Some studies have noted sleep disturbance as a long-term sequelae of meningitis.[ 17 ]
Diagnostics enteroviral meningitis.
To provide adequate treatment, patients with suspected meningitis require accurate and prompt diagnosis, which begins with a physical examination and assessment of existing symptoms.
To determine the causative agent of the disease (and differentiate viral and bacterial meningitis), the following tests are required: a nasopharyngeal swab, blood and stool tests, and an analysis of cerebrospinal fluid (by lumbar puncture). [ 18 ]
Cerebrospinal fluid or cerebrospinal fluid in enterovirus meningitis is examined using the multiplex PCR method – polymerase chain reaction, which allows detecting the presence of viral RNA in it. [ 19 ]
Instrumental diagnostics most often consists of computed tomography of the brain
More information in the article – Enterovirus infections – Diagnostics
Differential diagnosis
And differential diagnosis is performed with bacterial, tuberculous and fungal meningitis, Lyme disease, and other viral infections (arbovirus, herpes simplex virus, paramyxovirus, etc.). Other infectious etiologies to consider include mycoplasmas, spirochetes, mycobacteria, brucellosis and fungal meningitis or encephalitis. [ 20 ] Non-infectious etiologies include drugs (NSAIDs, trimethoprim-sulfamethoxazole, intravenous immune globulin), heavy metals, neoplasms, neurosarcoidosis, systemic lupus erythematosus, Behcet's syndrome and vasculitis. In children, Kawasaki disease may present similarly to bacterial or viral meningitis. [ 21 ]
Who to contact?
Treatment enteroviral meningitis.
Most viruses, including enteroviruses that cause meningitis, have no specific treatment other than supportive care. Fluid and electrolyte replacement and pain relief are the mainstays of treatment for viral meningitis. Patients should be monitored for neurologic and neuroendocrine complications, including seizures, cerebral edema, and SIADH.
As experts note, viral is usually a benign disease that goes away on its own.
Treatment to relieve symptoms includes NSAIDs (Ibuprofen, etc.) for fever and headache, and in case of severe vomiting, fluid and electrolyte levels in the body must be maintained (drink more water). In more severe cases, Dexamethasone is administered parenterally.
Pleconaril is a first-of-its-kind, orally active antiviral agent that selectively inhibits picornavirus replication by blocking viral attachment and uncoating. This placebo-controlled, double-blind study tested the efficacy of oral pleconaril in the treatment of viral enteroviral meningitis. Pleconaril significantly shortened the duration and severity of enteroviral meningitis symptoms in children and was well tolerated.[ 22 ]
Antibiotics are not effective against viruses, but upon admission to a medical facility - while the exact cause of the inflammation is unknown - they can be prescribed empirically, and after the viral pathogen is identified, the use of antibiotics is stopped.
For more details see:
Prevention
There is no special prevention for this disease, but following personal hygiene rules can prevent infection.
Forecast
Compared with meningitis caused by bacterial and fungal infections, as well as inflammation of the meninges caused by herpesviruses, enteroviral meningitis has a better prognosis, [ 23 ] and most patients recover completely.

