
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Causes, symptoms and diagnosis of anovulation
Medical expert of the article
Last reviewed: 12.07.2025

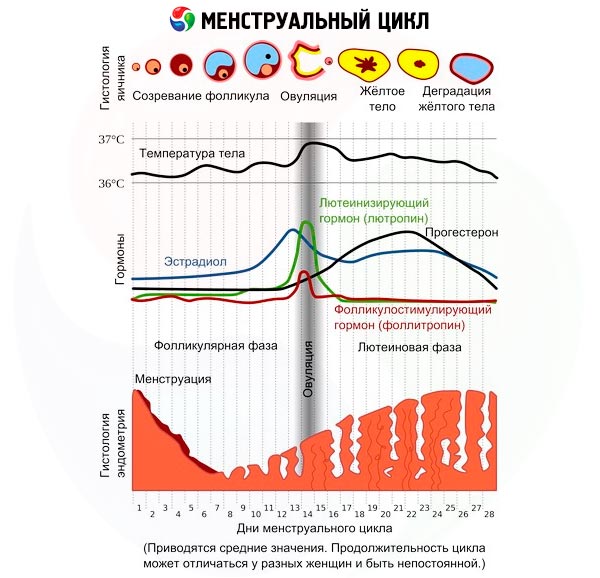
As soon as a girl's body is ready for motherhood, she begins her period. Approximately in the middle of the menstrual cycle, an egg cell, ready for fertilization, matures and leaves the ovary every month. This process is called ovulation and takes only a quarter of an hour. It is in the next 24 hours after the egg cell is released that it can be fertilized and a new life can begin. Dysfunction of the ovary, which is reduced to a violation of the maturation of the follicle and the egg cell in it or its release at the right time, is called anovulation. Ideally, a woman of fertile age should be ready to conceive, carry and give birth to a child from the moment of puberty until menopause. However, in reality, things are somewhat different.
Causes lack of ovulation
In practically healthy women, anovulatory cycles, when an egg is not released, may be observed several times a year. They are caused by hormonal disorders, since the ovulation process is controlled by hormones. The causes of anovulation with a normal (initially) hormonal background are embedded in its temporary fluctuations, sometimes quite significant, caused by dysfunctions of the hypothalamic-pituitary-ovarian system associated with nervous and physical overstrain; eating disorders (anorexia, bulimia, adherence to strict diets); taking medications; consequences of acute and relapses of chronic pathologies; a sharp change in climate; restructuring of the reproductive system and its transition to a new phase. Such periods include: puberty (development of fertility); postpartum (breastfeeding period); premenopausal (fading of fertility). Lack of ovulation caused by temporary reasons is physiological and does not require treatment.
Anovulation caused by oral contraceptives requires a separate discussion. Their action is based on the disruption of natural processes connecting the hypothalamus, pituitary gland and ovaries. In most women, fertility is restored without problems when they stop taking birth control pills, but not in all. This is very individual.
Pathological (chronic) anovulation is a regular absence of ovulation. Its main cause is hormonal imbalance caused by dysfunction of the ovaries. Ovulatory dysfunction is most often observed in women with polycystic ovary syndrome. Premature ovarian dystrophy, excess or deficiency of estrogens, follicle-stimulating hormone and luteotropin, and a violation of their ratio can affect the mechanism of ovulation development. Sclerocystic ovary disease, which is considered a complication of polycystic disease or dystrophy, consists of the formation of multiple small immature cysts with a dense membrane.
But anovulation due to lack of progesterone raises questions. After all, progesterone deficiency can only be discussed in the second phase of the cycle, when ovulation has already occurred. If there was no ovulation, then low progesterone levels are quite normal. Insufficient progesterone production is usually considered in the context of menstrual cycle disorders and the maturation of sex cells due to ovarian dysfunction. Isolated progesterone deficiency is almost never encountered, so progesterone therapy is criticized and is not recognized by all doctors, at least not by the masses.
Risk factors
Risk factors for ovulatory dysfunction are congenital pathologies of the reproductive organs and their development; adrenal hyperplasia; excess prolactin or androgens; history of acute and chronic inflammatory processes of the pelvic organs (especially endometritis and endometriosis ); sexually transmitted infections; thyroid dysfunction; chronic obesity or dystrophy; bad habits; the influence of autoimmune processes is also possible.
Pathogenesis
Pathogenetic links in the disruption of the ovulation process are the above-mentioned causes that upset the hormonal balance, the result of which is a disruption of the first phase of the ovulatory cycle at any stage - maturation or release of the egg from the dominant follicle.
Polycystic ovary syndrome plays a major role in the pathogenesis of anovulation. In this case, the hypothalamic-pituitary and ovarian ovulatory mechanisms are disrupted. In the pathogenesis of sclerocystosis, as its complication, hyperproduction of folliotropin is also considered, contributing to abnormal functioning of the ovaries and the formation of cysts covered with a dense membrane instead of follicles, which makes ovulation impossible. Luteotropin deficiency is also taken into account.
Another hypothesis puts the main causes in the hyperactivity of the adrenal cortex, steroid secretion disorders and estrogen deficiency, which disrupts the process of follicle maturation, leading to the development of androgenital syndrome, anovulation and amenorrhea.
The period of fertility development is characterized by anovulation, caused by insufficient levels of luteotropin, its production increases and reaches peak values by the age of 15-16. The reverse process - a decrease in the synthesis of hormones necessary for ovulation occurs when the ability to bear children fades (climacteric period).
In hypothalamic-pituitary disorders with excess prolactin, anovulation is a consequence of the inhibitory effect of its amount, which is several times greater than the norm, directly on the ovaries, on the pituitary function of producing luteotropin (it does not reach the peak necessary for ovulation), and on the hypothalamic function of synthesizing gonadotropin-releasing hormone.
Neoplasms of hypothalamic localization and other neuroprocesses in the hypothalamus, starvation, and a sharp decrease in body weight can provoke a decrease and even a complete cessation of the production of gonadotropin-releasing hormones even with normal prolactin levels.
A consequence of surgical intervention for pituitary adenoma, as well as radiation therapy, may be the absence of ovulation due to a sharp decrease in the level of gonadotropic hormones. This is also facilitated by excessive secretion of androgens.
Anovulation may be accompanied by the absence of menstruation or uterine bleeding, however, much more often women have a single-phase (anovulatory) monthly cycle, which ends with menstrual-like bleeding. The failure affects the ovulatory phase, and the secretory phase and the development of the corpus luteum do not occur at all. Almost the entire single-phase cycle is a proliferation of endometrial cells, followed by their necrosis and rejection. During its course, completely different stages of development and regression of the follicle occur in the ovaries in nature and duration.
Anovulation is more characterized by hyperestrogenism throughout the cycle, without a change to progesterone exposure in the second phase of the normal cycle. Although sometimes the estrogen level is reduced, which affects the nature of changes in the endometrium - from hypo- to hyperplastic, accompanied by the growth of glandular polyps.
Bleeding at the end of an anovulatory cycle is explained by the regression of immature follicles, which is usually accompanied by a decrease in estrogen levels. The functional layer of the endometrium undergoes destructive changes - vascular permeability increases, effusions, hematomas, and tissue necrosis appear. The superficial layer of the endometrium is rejected, causing bleeding. If this does not happen, diapedetic bleeding occurs due to the migration of erythrocytes through the vascular membranes.
Every third case of female infertility, according to statistics, is caused by the absence of ovulation. In turn, gynecologists call polycystic ovary syndrome the leading cause of this dysfunction, which is diagnosed in no more than every tenth representative of the fair sex of childbearing age. At the same time, external signs of polycystic disease are detected during ultrasound examination of the ovaries of women of fertile age twice as often. But the clinical picture corresponding to polycystic ovary syndrome is not found in everyone.
Sclerocystic ovary disease is diagnosed in three to five percent of gynecological pathologies, and a third of cases are accompanied by persistent infertility.
Symptoms lack of ovulation
Women generally learn about the absence of ovulation when their desire to become a mother is not realized. After several fruitless attempts to get pregnant, most women go to the doctor to find out what is wrong with them. Therefore, the main symptom of anovulation is the inability to get pregnant. Sometimes, amenorrhea is observed during anovulation (after strong emotions, regular exhausting exercise, strict diets and fasting). However, most women continue to have periods during anovulation, or rather bleeding, which the woman takes for menstruation, since the difference is not felt either in their frequency, or in quantity (blood loss), or in quality (the woman's well-being during this period). Anovulation with regular periods is not at all uncommon, but rather even the norm.
Uterine bleeding is not always regular, however, women interpret this as a change in the length of the cycle and usually do not rush to see a doctor.
Hyperestrogenism is characterized by heavy and prolonged bleeding. Their result can be the development of anemia, accompanied by its symptoms - weakness, rapid fatigue, dizziness, shortness of breath, pale skin, dry and brittle hair and nails.
Estrogen deficiency (hypoestrogenism) is characterized by scanty monthly discharge and its short duration. Amenorrhea may be observed, which may indicate sclerocystosis. In this case, ultrasound shows enlarged or wrinkled ovaries, necessarily covered with lumpy formations with cystic contours. Male-pattern hair growth, underdevelopment of the uterus and mammary glands, excess weight. The presence of all symptoms is not necessary. Symptoms of general malaise may be observed - sleep disorders, libido, headaches, weakness, lethargy, fatigue.
The first signs of anovulation are not very obvious, the most noticeable of them is the absence of menstruation, which is not often observed. However, such symptoms as irregularity, change in the amount of discharge (oligomenorrhea); absence of the usual signs of approaching menstruation (premenstrual syndrome) or their noticeable decrease; absence of an increase in basal body temperature in the supposed second phase of the cycle should alert you.
Alarming symptoms may include hirsutism (excessive growth of androgen-dependent hair), significant changes in body weight over a short period of time, light discharge from the nipples (hyperprolactinemia), and sudden mood swings.
Sometimes you need to be very attentive to yourself and your body in order to notice problems with your monthly ovulatory cycle and seek medical help in time, rather than at an advanced stage.
The following types of anovulation are distinguished depending on the cause: physiological and pathological anovulation. The first includes periods of fertility restructuring - adolescence, postpartum and the period of its fading.
Anovulatory cycles can happen to any woman during periods of very high stress, due to alimentary reasons, acute diseases and exacerbations of chronic ones. Often they are simply not noticed, sometimes, if the reasons that caused them are significant and long-term, a woman's menstruation may stop or its frequency and intensity may change. When the stress factor for the body is eliminated, the woman's condition usually normalizes.
In pathological anovulation, the absence of the second phase of the menstrual cycle occurs regularly. Chronic anovulation is necessarily accompanied by persistent infertility and is often detected precisely during attempts to realize one's maternal function. Expressed symptoms are not typical for the chronic form of absence of ovulation, monthly bleeding is usually regular. You can mainly suspect this pathology by measuring your basal temperature. Pathological anovulation is subject to mandatory treatment if a woman plans to have children.
Complications and consequences
Regular absence of ovulation can lead to worsening hormonal imbalance, disruption of ovarian function, even if anovulation was caused by other reasons, because the entire hypothalamic-pituitary-ovarian axis is involved in the process.
Chronic anovulation with hyperestrogenism results in profuse uterine bleeding, leading to hematopoiesis disorders and anemia. Refusal of treatment usually leads to persistent infertility.
Diagnostics lack of ovulation
There are two ways to determine at home whether ovulation is normal: by measuring your basal temperature over several menstrual cycles and plotting it, or by using an express ovulation test purchased at a pharmacy.
The temperature graph of the anovulatory cycle has the form of a monotonous curve, less often a broken line, all graph indicators do not exceed 37℃.
The rapid test records the peak content of luteotropin in the urine before ovulation; if ovulation does not occur, then there is no jump in this indicator.
If there is a suspicion of ovulatory dysfunction, it is necessary to consult a specialist and undergo a thorough diagnostic examination. All patients with anovulation are recommended medical and genetic counseling; sometimes an endocrinologist consultation is necessary.
In addition to the usual medical interview and classic clinical tests, to determine the general health of a woman, specific tests are prescribed to provide an idea of her hormonal status.
The most accurate idea of the degree and nature of ovulatory disorder is given by the serum levels of prolactin and gonadotropic hormones ( follicle-stimulating and luteinizing ).
Elevated serum prolactin levels require consultation with an endocrinologist and a blood test for plasma concentrations of TSH, T4, T3 (thyroid hormones).
In case of disruption of the coordinated work of the hypothalamus and pituitary gland and normal prolactin content, the serum level of follicle-stimulating hormone, luteotropin, and estradiol may be normal (normogonadotropic anovulation) or decreased (hypogonadotropic anovulation).
In case of ovarian anovulation, the follitropin content significantly (four to five times or more) exceeds the normal value. The assumption of such an origin of anovulation forces the appointment of minimally invasive diagnostics - ovarian biopsy using a laparoscope, as well as immunological tests to detect autoantibodies to ovarian tissue.
An increase in the serum concentration of luteotropin, in particular the ratio of its level to the content of follicle stimulating hormone, supported by appropriate symptoms, suggests the presence of polycystic ovary syndrome.
Ovulatory dysfunction is indicated by low serum progesterone levels in the second phase of the cycle (when this second phase is determined depending on the individual cycle, and not according to the standard scheme on the 21st day), as well as the absence of secretory changes obtained as a result of diagnostic curettage (endometrial scraping).
Serum estradiol levels may be significantly reduced (oligomenorrhea) or normal in regular anovulatory cycles.
The progesterone test is used as an alternative to the previous analysis: the body's reaction to the intramuscular injection of progesterone for seven to ten days can confirm sufficient saturation with estrogens (uterine menstrual-like bleeding occurs within two to five days after the course) and insufficient - the result is negative.
The patient's androgen status is assessed, and in the case of elevated levels of male sex hormones, a dexamethasone test is prescribed to clarify the origin of hyperandrogenism.
A PCR test may also be performed to check for sexually transmitted infections.
Of the hardware studies, the first thing the patient is prescribed is an ultrasound scan for anovulation. During an ultrasound scan, the absence of a dominant follicle is visible on the computer monitor. In polycystic ovary syndrome, more follicles mature at once than necessary, it is impossible to isolate the dominant one, and they do not mature completely, but turn into cysts that “grow” on the ovary. The ultrasound specialist sees a similar picture with multifollicular ovaries. Differentiation is carried out based on hormonal background tests.
Other instrumental diagnostics may be required – ultrasound and X-ray of the mammary glands, tomography of the brain, examination of the thyroid gland.
Differential diagnosis
Based on the examination results, differential diagnostics are performed. The exact cause of anovulation is determined by the method of data analysis and exclusion, neoplasms are excluded, in particular, of the pituitary gland.
Who to contact?
Treatment lack of ovulation
Ovulatory dysfunction that occurs as a result of high physical activity does not require hormonal treatment. With a decrease in the intensity of training and dosing of loads, anovulation goes away on its own.
Prevention
In preventing the development of anovulation, a huge role is played by educating teenage girls about their pragmatic attitude to their health: understanding the need to maintain rational physical activity, an optimal work and rest regime, and timely visits to a doctor when symptoms of trouble in the sexual sphere appear. Familiarizing them with methods of preventing sexually transmitted infections, minimizing stress, and the need for adequate nutrition.
The diet of a woman of fertile age should consist of two-thirds of plant-based products - vegetables, fruits, legumes, cereals. A third should be protein products - meat, fish, dairy. Estrogen deficiency is associated with a lack of zinc and copper in the body, so the diet must include eggs, liver, seafood, bran and whole grain bread, green leafy vegetables (raw).
 [ 21 ]
[ 21 ]

