
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Psoriasis vulgaris
Medical expert of the article
Last reviewed: 04.07.2025

Vulgar psoriasis is considered the most common form of this dermatological disease. It is also sometimes called ordinary or simple.
This pathology is characterized by the appearance of papules on the skin, covered with peculiar white scales – particles of keratinized tissue.
Epidemiology
The results of various statistical surveys have shown that vulgar psoriasis is observed in approximately 2% of the world's population (for example, in Denmark 2.9% of the population suffers from it, in the northern part of Europe (including England) - 2%, in the USA - 1.4%, and in China - 0.37%).
Causes psoriasis vulgaris
At present, there is no single theory that could fully explain the causes of vulgar psoriasis. That is why this disease is classified as a multifactorial dermatoses.
Among the most popular explanations for the causes of psoriasis are the following:
- Hereditary cause – most often the disease is diagnosed in 2, as well as 5-6 generations. Transmission occurs in two ways: recessive, as well as autosomal dominant;
- Metabolic causes – the disease occurs due to metabolic disorders. This mainly concerns the processes of cholesterol metabolism, enzymes, and disruption of RNA and DNA replication;
- Viral cause – was identified as a result of separate experiments conducted on rabbits. After implantation of skin particles affected by psoriasis, they began to develop fibrosis, as well as atrophy and other morphological modifications in the organs. However, it has not yet been possible to determine which specific virus provoked these disorders;
- Endocrine cause - many patients are diagnosed with disorders of endocrine origin. Among them are dysfunction of the gonads and the hypothalamic-adrenal system;
- Neurogenic cause, which explains the development of psoriasis by the presence of serious psychological disorders in the patient.
Pathogenesis
There are 2 main theories explaining the mechanism of occurrence of vulgar psoriasis.
The first of them explains the appearance of psoriasis by a violation of the process of maturation and division of epithelial cells, which causes their excessive growth and increased proliferation. Thus, in this case, the occurrence of pathology occurs as a result of a violation of the function of tissues and keratocytes. It should be noted that in this case, the aggressive reaction of mononuclear phagocytes and T-lymphocytes to skin cells, as well as their penetration into the skin, is considered a secondary response of the body to the rapid proliferation of keratocytes altered by the disease. This theory is confirmed by the fact that the treatment of this pathology with drugs that prevent the proliferation of keratocytes (demonstrating only a small degree of impact or no immunomodulatory effect at all) gives positive results.
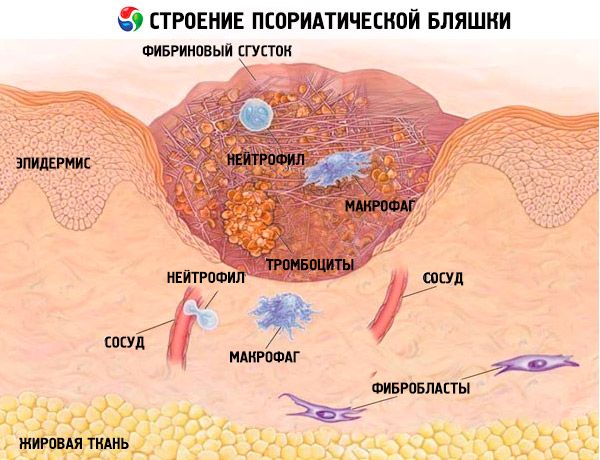
The second theory considers this pathology as one of the types of immunopathological, autoimmune disease, in the process of development of which increased growth and reproduction of skin cells are considered secondary regarding the influence of lymphokines, inflammation mediators, as well as cytokines, which are produced by immune cells. The process of occurrence of pathology is associated with penetration into the skin of cells that protect the body from the occurrence of malignant tumors and infections (the so-called T-helpers, as well as T-killers). As a result, a large number of cytokines are released, which are provocateurs of the inflammatory process and accelerate the process of proliferation of skin cells (including keratocytes).
Symptoms psoriasis vulgaris
Usually the disease develops gradually, but in some cases there is an acute onset. Among the first signs of vulgar psoriasis is the appearance of a nodular rash on the skin, which has a red or pink color. Such a rash is called papules - dense nodules limited in area, on top of which there are grayish-white scales. Not every one of them shows peeling, but if you try to scrape off the top of the papule, it will be easy to detect. The rash is usually not abundant and is located on the same area of the skin for a long time. It can be localized under the hair on the head, above large joints, etc.
Stages
Vulgar psoriasis has 3 stages of development: progressive, regressive and stationary, each of which has its own clinical specifics.

In the case of a regressive stage of the disease, the patient experiences:
- Reduction of the intensity of skin peeling or complete cessation of this process;
- Gradual disappearance of psoriatic rash and plaques, after which hypopigmentation begins to develop (sometimes hyperpigmentation begins to develop instead);
- Development of the psoriatic triad and negative isomorphic reaction.
Stationary stage
Among the characteristic signs of the stationary stage of the disease development are the following manifestations:
- Stopping the growth of new nodules;
- The size and number of existing papules remain the same, and peripheral growth is not observed;
- Moderate degree of peeling of the rash surface;
- The formation of a whitish rim begins, which surrounds the rash nodule with a horny layer (this process is called Voronov's symptom) - this indicates that the stationary stage is beginning to transition to a regressive stage;
- Negative isomorphic reaction and the emergence of the psoriatic triad.
Progressive stage
The progressive stage of psoriasis is characterized by the following manifestations:
- Periodic appearance of a new rash on the skin, which has a specific erythematous border, on which there are no plaques (while there are plaques on the rash itself);
- Existing nodules increase in size due to peripheral growth (they look like a hyperemic rim around the rash);
- The so-called Koebner reaction gives a positive result - new nodules appear on the damaged parts of the skin (the injury can be caused by a scratch, a needle prick, a sunburn or the use of an irritating ointment);
- Psoriatic rashes are very flaky, except for the area where the nodules themselves grow;
- Positive triad.
Vulgar plaque psoriasis
Plaque psoriasis is the most common type of the disease, in which the skin becomes inflamed, reddened and flaky. According to statistics, approximately 4 out of 5 people diagnosed with psoriasis have its plaque form (it is also sometimes called ordinary psoriasis). This pathology is characterized by thick red-violet plaques, on top of which silvery scales appear. Such a rash can appear on any part of the body. The appearance of rashes causes pain and itching.

Limited and widespread psoriasis vulgaris
Vulgar psoriasis can be limited or widespread. In the limited form, the rash appears on individual areas of the skin, covering a maximum of 40% of the entire surface. If a larger area of skin is affected, the pathology is classified as a widespread form.
Complications and consequences
Vulgar psoriasis can cause complications in the area of joints or nails. Nails are affected multiple times, point depressions appear on them. Often, over time, they peel off and fall off completely. Hyperkeratosis begins under the nail plate - this symptom is also called an "oil spot".
Joint complications from psoriasis can be quite serious. Various arthropathies develop, making it more difficult for the patient to move, especially in the morning, after sleep. Joints become deformed, mainly between the phalanges of the fingers - they become curved, they atrophy, which is why a person loses the ability to perform even ordinary movements.
On the part of the nervous system, such complications as depression, apathy and constant oppression along with indifference to everything are quite common. Complexes can develop (especially in a small child), so it is imperative to be observed by a psychologist.
Diagnostics psoriasis vulgaris
Usually, it is not difficult to diagnose the chronic form of vulgar psoriasis - the disease has characteristic external manifestations, so diagnosis does not cause difficulties. There are no specific diagnostic procedures or blood tests for this disease.
A typical manifestation of the chronic form of vulgar psoriasis is that scraping off the plaque easily causes bleeding.
Tests
In the case of an extensive form of the disease, or if it is in a progressive stage, deviations can be detected by taking blood tests, after which the presence of inflammatory, autoimmune, and rheumatic processes (development of leukocytosis, and in addition to it, an increased level of ESR, determination of C-reactive protein, etc.) is detected, as well as endocrine and biochemical disorders.
To confirm the diagnosis and exclude other dermatological pathologies, a skin biopsy may be performed. In this case, the following may be revealed:
- Immaturity and thickening of the keratinocyte layer;
- Signs of accelerated proliferation of keratocytes, as well as immunocompetent formations;
- Massive penetration of macrophages, branched cells, and T-lymphocytes into damaged skin;
- The process of formation of new blood vessels in the skin layer under psoriasis plaques accelerates.
Differential diagnosis
Vulgar psoriasis should be distinguished from dermatoses: nodular syphilid, lichen planus, and Reiter's syndrome; in addition, with seborrheic eczema and dermatitis, pityriasis rosea, and neurodermatitis. It should also be distinguished from follicular or parafollicular keratosis and parapsoriasis, granuloma fungoides in the infiltrative-plaque phase, and DLE.
Who to contact?
Treatment psoriasis vulgaris
Vulgar psoriasis can be treated in a variety of ways. All questions about the choice of treatment methods and its scheme, as well as the selection of drugs, dosages and other details are decided for each patient individually. For each, the severity of the disease and its prevalence, the absence / presence of any concomitant diseases, as well as contraindications, etc. are taken into account.
In hospital mode, the treatment process includes the following procedures:
- Detoxification of the patient's body;
- Systemic use of drugs;
- Implementation of local therapy.
If the disease is localized or moderately severe, therapy can be performed on an outpatient basis. In this case, local medications are mainly used. Specific medications are selected depending on the stage of the disease. Both hormonal and non-hormonal agents can be used.
Medicines
The following treatment is carried out in hospital.
If the patient has high blood pressure, magnesium sulfate is administered intramuscularly.
If psoriasis develops in an exudative form, diuretics are prescribed.
If the patient has severe itching and a tendency to allergic reactions, antihistamines should be used, such as Suprastin, Tavegil or Diphenhydramine.
Systemic treatment with glucocorticosteroids is almost never used nowadays, as it increases the risk of side effects and complications. Therefore, they are prescribed only in cases where other methods have not yielded positive results.
In case of severe course of the pathology, cytostatics are used for treatment – Methotrexate and Cyclosporine, as well as retinoids – Acitretin.
Also, in the treatment process, drugs containing monoclonal antibodies are now increasingly used: such as Efalizumab or Infliximab.
As for local preparations, their use should be careful. During an exacerbation of the disease, irritated skin should not be treated with ointments of strong action and high concentration. Such products as ASD fraction, naphthalan paste and lanolin cream are effective. But hormonal ointments should be used only for a short time.
In the outpatient setting, hormonal drugs are used, including glucocorticosteroids in the form of gels, creams, as well as emulsions and lotions (such as Hydrocortisone or Elokom). Non-hormonal agents are also used - Anthralin, Dithranol, Tazarotene and Calcipotriol. Combined local drugs - Locacortentara and Belosalik - are also effective.
Vitamins
During the treatment, it is essential to use agents that improve cellular metabolism in the body - these are vitamins from groups B and C, as well as P and A, E and D.
Physiotherapy treatment
Among the methods of physiotherapeutic treatment of vulgar psoriasis, the main ones are the following procedures:
- electrosleep;
- magnetic and magnetic laser treatment;
- UV irradiation procedures, as well as PUVA.
If the patient is in an acute stage of the disease, UV irradiation procedures are not allowed to be used, and PUVA is performed in limited quantities and with caution.
Traditional and herbal medicine
To make the treatment more effective, you can use folk remedies. For example, take additional warm baths from extracts and tinctures of medicinal herbs - such as calendula, chamomile or pine. At the same time, you cannot use washcloths when bathing, or rub yourself with a towel, limiting yourself to simply blotting. This is necessary because microtraumas can occur on the skin due to rubbing, which increases the risk of exacerbation of the disease, as well as the possible addition of some secondary infection.
Here are some more recipes that help in the treatment of psoriasis:
Take 20 g of sarsaparilla root and infuse them in 1 liter of plain water for 8-10 hours. Then boil the infusion for about 20 minutes and then strain. Drink half of the decoction hot, and the other half within 24 hours. The course lasts 20 days.
Areas of skin affected by psoriasis should be lubricated with rosehip ash, which should first be mixed with petroleum jelly in equal proportions.
Tincture of black elderberry (add 2 teaspoons to 5 liters of water). Drink 3 times a day, 0.5 cups. Fir water can be used instead of elderberry tincture.
Grind young sunflower heads, then pour white wine over them, and then leave to infuse for 2 days. Strain the finished tincture and moisten the inflamed areas of the skin with it. You can also apply bandages to them, leaving them for 2-3 hours. If the rash appears on the face, you can wash your face with this tincture.
Homeopathy
The homeopathic medicine Dulcamara Plus is used in cases of acute vulgar psoriasis.
Contraindications include: hypersensitivity to the homeopathic components of the medicine, as well as age under 18 years.
The drug should be taken only as prescribed by a homeopath. The granules should be placed under the tongue and then sucked for some time. They should not be chewed, nor should they be washed down with water. The medicine should be taken half an hour before meals or 1 hour after. The dosage is usually 8 granules three times a day. The treatment course can last up to 30 days, but only after a mandatory consultation with a dermatologist.
Among the side effects of the drug - sometimes the patient may experience an allergy. In this case, he will need to consult a dermatologist.
Among homeopathic preparations for psoriasis, such remedies as Loma Lux Psoriasis (the dose depends on the patient’s weight and is 0.5-2 teaspoons in the morning on an empty stomach) and Polyderm (take 3-5 granules three times a day for 5-6 months) also help.
Diet
It is possible to get rid of vulgar psoriasis only if you normalize your daily routine and correct your diet. You need to eliminate foods that contain components such as carbohydrates (easily digestible) and refractory fats from your diet. The diet for vulgar psoriasis also includes avoiding spicy foods, salt, various spices, semi-finished products, and products with increased allergenicity. In addition, you need to avoid foods with dyes and food additives, pickled and smoked products, and alcohol.
More information of the treatment
Forecast
Vulgar psoriasis has a fairly favorable prognosis, but it should be taken into account that there is no certainty regarding the duration of the disease, as well as periods of exacerbation and remission. Skin rashes can exist for a long time, for years, but usually periods of exacerbation alternate with periods of time when improvements and clinical recovery are observed. A considerable number of patients, especially those who did not undergo a course of systemic intensive therapy, experienced long periods of spontaneous clinical recovery.


 [
[