
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Trigonocephaly
Last reviewed: 04.07.2025
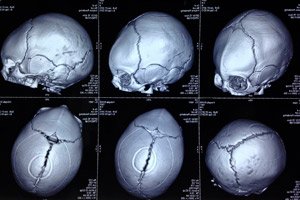
A congenital anomaly in the form of a skull deformation, in which the head of infants has an irregular shape and the skull appears triangular, is defined as trigonocephaly (from the Greek trigonon – triangle and kephale – head). [ 1 ]
Epidemiology
The prevalence of craniosynostosis is estimated at approximately five cases per 10,000 live births (or one case per 2,000–2,500 people in the general population). [ 2 ]
In 85% of cases, craniosynostosis is sporadic, the remaining cases occur as part of a syndrome. [ 3 ]
According to statistics, premature fusion of the median frontal suture is the second most common form of craniosynostosis, and trigonocephaly accounts for one case in 5-15 thousand newborns; the number of male infants with this anomaly is almost three times higher than that of female infants. [ 4 ]
In approximately 5% of cases, this congenital anomaly is present in the family history. [ 5 ]
Causes trigonocephaly
The normal formation of the skull occurs due to the presence of primary growth and bone remodeling centers in it – craniofacial synarthroses (joints), which close at a certain time during the development of the head skeleton, ensuring the fusion of bones. [ 6 ]
The frontal bone (os frontale) of the newborn's skull consists of two halves, between which there is a vertical fibrous connection - the median frontal or metopic suture (from the Greek metopon - forehead), which runs from the top of the bridge of the nose up the midline of the forehead to the anterior fontanelle. This is the only fibrous cranial suture that heals in infancy: from 3-4 months to 8-18. [ 7 ]
See also – Changes in the skull after birth
The causes of trigonocephaly are metopic craniosynostosis (craniosynostosis) or metopic synostosis (from the Greek syn – together and osteon – bone), that is, premature (before the third month) immobile fusion of the bones of the cranial vault along the median frontal suture. Thus, craniosynostosis and trigonocephaly are related as cause and effect or as a pathological process and its result. [ 8 ]
In most cases, trigonocephaly in a child is the result of primary (isolated) craniosynostosis, the exact cause of which is unknown. Isolated craniosynostosis occurs sporadically, likely due to a combination of genetic and environmental factors. [ 9 ]
But trigonocephaly can be part of congenital syndromes that arise due to chromosomal abnormalities and mutations of various genes. These include: Opitz trigonocephaly syndrome (Bohring-Opitz syndrome), Apert syndrome, Loeys-Dietz syndrome, Pfeiffer syndrome, Jackson-Weiss syndrome, craniofacial dysostosis or Crouzon syndrome, Jacobsen, Saethre-Chotzen, Münke syndromes. In such cases, trigonocephaly is called syndromic. [ 10 ]
At birth, the brain size is usually 25% of its adult size, and by the end of the first year of life it reaches about 75% of the adult brain. But with primary delay in brain growth, so-called secondary craniosynostosis is possible. The etiology of the delay is associated with metabolic disorders, some hematological diseases, and teratogenic effects of chemicals on the fetus (including those in pharmaceuticals). [ 11 ]
According to experts, trigonocephaly in adults who were not treated in childhood, as a result of isolated craniosynostosis or congenital syndrome, persists throughout life. [ 12 ]
Risk factors
Experts believe that the main risk factors for trigonocephaly (and metopic craniosynostosis as its cause) are genetic: over the past two decades, more than 60 genes have been identified whose mutations are associated with premature, immobile fusion of the cranial bones in infants.
The risk of developing pathologies of craniofacial synarthrosis and general osteogenesis (bone formation) increases in cases of abnormal presentation of the fetus, intrauterine hypoxia, multiple pregnancy, alcohol consumption, drug use or smoking during pregnancy. [ 13 ]
Pathogenesis
According to the prevailing theory, the pathogenesis of trigonocephaly is rooted in a disruption of fetal osteogenesis in the early stages of pregnancy, most often caused by genetic factors, since random chromosomal abnormalities are detected in newborns with metopic craniosynostosis. For example, one of the most common is trisomy 9p, which leads to craniofacial and skeletal defects, mental retardation and psychomotor development. [ 14 ]
Due to the too early fusion of the median frontal suture, growth in this area of the skull is hindered: lateral growth of the frontal bone is limited with shortening of the anterior cranial fossa; a bony ridge is formed along the midline of the forehead; there is a convergence of the bones that form the orbits and depression of the temporal bones. [ 15 ]
But the growth of the skull in other areas continues: there is compensatory sagittal (front-back) and transverse growth of the back of the skull (with expansion of its parietal-occipital part), as well as vertical and sagittal growth of the upper part of the face. As a result of these disorders, the skull acquires an irregular shape - triangular.
Symptoms trigonocephaly
The main symptoms of trigonocephaly are changes in the shape and appearance of the head:
- when viewed from above the crown of the head, the skull has the shape of a triangle;
- narrowed forehead;
- a noticeable or palpable ridge (bony protrusion) running along the center of the forehead, giving the frontal bone a pointed (keel-shaped) appearance;
- deformation of the upper part of the orbits (flattening of the supraorbital ridges) and hypotelorism (reduced distance between the eyes).
The frontal (anterior) fontanelle may also close prematurely.
In syndromic trigonocephaly there are other anomalies and signs of mental retardation in children. [ 16 ]
Complications and consequences
Diagnostics trigonocephaly
Trigonocephaly is diagnosed at birth or within a few months of birth. However, the less severe findings of metopic craniosynostosis may not be detected until early childhood.
To visualize the pathology of the skull, instrumental diagnostics are carried out using computed tomography of the head and ultrasound. [ 19 ], [ 20 ]
Differential diagnosis
Differential diagnosis is necessary to distinguish a syndromic defect from isolated metopic synostosis, for which the child is given a genotype test.
Treatment trigonocephaly
In some children, cases of metopic synostosis are quite mild (when there is only a noticeable groove on the forehead and no other symptoms), which do not require specific treatment. [ 21 ]
Treatment of severe trigonocephaly is surgical and involves an operation to correct the shape of the head and ensure normal brain growth, as well as surgical correction of facial bone deformities. [ 22 ]
This surgical procedure – synostectomy of the metopic suture, orbital rim shift and cranioplasty – is performed before the age of 6 months. The child is monitored until the age of one year; during the first years of life, the child is examined periodically to ensure that there are no problems with speech, motor skills or behavior. [ 23 ]
Prevention
There are no methods for preventing this congenital defect, but genetic counseling can prevent the birth of a child with an incurable craniocerebral pathology.
Craniosynostosis in a fetus can be detected by performing a prenatal ultrasound of its head in the second and third trimesters of pregnancy.
Forecast
The prognosis largely depends on the degree of skull deformation, which affects the neurocognitive functions of the brain. And if corrective surgery has not been performed, children with trigonocephaly – compared to healthy peers – have lower general cognitive abilities, problems with speech, vision, attention and behavior.
