
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Sheehan's syndrome
Medical expert of the article
Last reviewed: 04.07.2025
Ischemic necrosis of the pituitary gland and persistent decline in its function due to postpartum hemorrhage is called Sheehan's syndrome. This rare complication of childbirth, accompanied by life-threatening blood loss, is also called postpartum pituitary insufficiency, postpartum hypopituitarism, pituitary (diencephalic-pituitary) cachexia, or Simmonds' disease.
This endocrine pathology has the code E23.0 according to ICD-10.
Epidemiology
In developed countries, due to the high level of obstetric care, Sheehan's syndrome is rare: its frequency has decreased over 50 years from 10-20 cases per 100 thousand women to 0.5% of all cases of hypopituitarism in women.
According to the European Society of Endocrinology, some symptoms of mild damage to the anterior pituitary gland are observed in 4% of women who have lost a lot of blood during childbirth. Moderate signs of Sheehan's syndrome are diagnosed in 8%, and severe forms of postpartum hypopituitarism are found in 50% of women after hypovolemic shock.
The international database of the pharmacoepidemiological registry KIMS (Pfizer International Metabolic Database) for 2012 listed 1034 patients with growth hormone deficiency (GH), and in 3.1% of cases in female patients the cause of this pathology is Sheehan syndrome.
Postpartum hypopituitarism poses a serious threat to women in underdeveloped and developing countries. For example, in India, the prevalence of Sheehan syndrome is estimated at 2.7-3.9% among parous women over 20 years of age.
Causes Sheehan's syndrome
All causes of Sheehan's syndrome are the result of hypovolemic shock, which develops with a sharp decrease in circulating blood volume and a drop in blood pressure caused by bleeding during childbirth.
With massive blood loss (more than 800 ml), the blood supply to the organs and the supply of oxygen to them are disrupted. And, first of all, this concerns the brain. Sheehan's syndrome occurs due to damage to the pituitary gland - the brain gland responsible for the synthesis of the most important hormones.
The hormone-producing cells of its anterior lobe, the adenohypophysis, suffer the most. During pregnancy, under the influence of placental hormones, the size of this gland increases, according to some estimates, by 120-136%. In particular, hypertrophy and hyperplasia of lactotropocytes occurs - cells that synthesize prolactin, which is necessary for the development and preparation of the mammary glands for milk production.
Risk factors
Obstetricians and gynecologists note risk factors for the development of Sheehan's syndrome:
- blood clotting disorders in pregnant women (in particular, thrombocytopenia);
- edema of peripheral tissues (in which the hypothalamic hormone vasopressin is activated, increasing vascular tone and blood pressure);
- gestational hypertension (high blood pressure);
- preeclampsia (high blood pressure and proteinuria);
- increased hemolysis (destruction of red blood cells, most often associated with renal failure).
There is an increased risk of bleeding during childbirth and the development of Sheehan's syndrome in cases of placenta previa, its premature detachment, as well as in multiple pregnancies (twins or triplets) and in rapid (stormy) labor, during which there may be an embolism of the pulmonary vessels with amniotic fluid.
Pathogenesis
The pathogenesis of Sheehan's syndrome is associated with hypoxia of the pituitary tissues and their death. The main role in the increased vulnerability of the adenohypophysis is played by the peculiarity of its blood supply: through the portal venous system and the network of capillary anastomoses of the portal vessels. With severe bleeding and a drop in blood pressure, local blood flow in the enlarged anterior lobe of the gland is absent; spasm of the blood vessels feeding the pituitary gland associated with shock leads to oxygen deficiency and ischemic necrosis of the gland.
As a result, the pituitary gland does not produce sufficient amounts of the following tropic hormones:
- somatotropin (STH), which activates cellular protein synthesis, regulates carbohydrate metabolism and lipid hydrolysis;
- prolactin (luteotropic hormone), which stimulates the development and function of the mammary glands and corpus luteum;
- follicle-stimulating hormone (FSH), which ensures the growth of ovarian follicles and proliferative processes in uterine tissue;
- luteinizing hormone (LH), responsible for ovulation;
- adrenocorticotropic hormone (ACTH), which activates the production of corticosteroids by the adrenal cortex;
- thyroid stimulating hormone (TSH), which regulates the secretory function of the thyroid gland.
Symptoms Sheehan's syndrome
An imbalance of hormones produced by the pituitary gland causes a wide variety of symptoms in Sheehan's syndrome, depending on the degree of deficiency in the secretion of specific pituitary hormones.
The amount of damaged pituitary cells determines the acute and chronic forms of the disease. The acute form reflects significant damage to the anterior lobe of the gland, and symptoms become apparent soon after birth. In chronic cases, the damage detected is smaller, and symptoms may not appear for months or years after birth.
The most common early signs of Sheehan's syndrome are agalactia, i.e. lack of lactation. Due to a prolonged lack of estrogens, the menstrual cycle does not resume at the proper time after childbirth, the mammary glands decrease in size, and the vaginal mucosa becomes thinner. And the gonadotropin deficiency is expressed in amenorrhea, oligomenorrhea, and decreased libido. In some women, menstruation resumes, and a second pregnancy is possible.
The characteristic symptoms of thyroid-stimulating hormone deficiency in Sheehan syndrome include fatigue and impaired thermoregulation with intolerance to cold; dry skin, hair loss and brittle nails; constipation and weight gain. These symptoms usually develop gradually.
The consequences of somatotropin deficiency are limited to some loss of muscle strength, an increase in body fat, and increased sensitivity to insulin. In both acute and chronic forms, there may be signs of diabetes insipidus: intense thirst and increased diuresis (urine volume).
Symptoms of Sheehan's syndrome also include signs of secondary adrenal insufficiency, i.e. ACTH deficiency. This includes decreased overall tone and weight loss, hypoglycemia (low blood sugar), anemia, and hyponatremia (low sodium). Deficiency of this hormone leads to chronic hypotension with fainting and orthostatic hypotension, and inability to respond to stress. Hypopigmentation and folds in the skin (several weeks or months after birth) are also observed.
Exacerbation of adrenal insufficiency, requiring urgent medical care, occurs with severe infections or surgical interventions.
Complications and consequences
Severe pituitary failure in Sheehan syndrome can lead to coma and death.
Less common is also potentially life-threatening postpartum panhypopituitarism, when 90% of the adenohypophysis tissue is affected. The consequences and complications of this severe form of Sheehan's syndrome include: persistent low blood pressure, cardiac arrhythmia, low blood sugar (hypoglycemia), and hypochromic anemia.
Diagnostics Sheehan's syndrome
Typically, the diagnosis of Sheehan's syndrome is based on clinical features and the patient's medical history, particularly whether there was bleeding during labor or any other complications associated with labor. Information regarding problems with lactation or absence of menstruation after delivery are two important signs of this syndrome.
Blood tests are required to check the levels of pituitary hormones (TSH, ACTH, FSH, LH, T4), cortisol and estradiol.
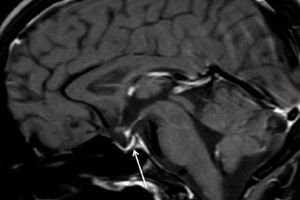
Instrumental diagnostics – using computed tomography (CT) or magnetic resonance imaging (MRI) of the brain – allows us to examine the size and structure of the pituitary gland. In the early stages, the pituitary gland is enlarged, over time the gland atrophies, and a diagnostic sign of pathology such as an “empty sella turcica” develops, which is revealed by scanning, i.e. the absence of the pituitary gland in the pituitary bone fossa at the base of the brain.
Differential diagnosis
The task that differential diagnosis must perform is to identify other diseases that manifest as hypopituitarism: pituitary adenomas, craniopharyngiomas, meningiomas, chordomas, ependymomas or gliomas.
The pituitary gland can be damaged by brain abscess, meningitis, encephalitis, neurosarcoidosis, histiocytosis, hemochromatosis, autoimmune or lymphoblastic hypophysitis, and autoimmune antiphospholipid syndrome.
Who to contact?
Treatment Sheehan's syndrome
Treatment of Sheehan's syndrome is lifelong hormone replacement therapy using synthetic analogues of tropic hormones of the ovaries, thyroid gland, and adrenal cortex.
Thus, the deficiency of ACTH and cortisol is compensated by taking glucocorticoids (Hydrocortisone or Prednisolone). Thyroxine preparations (Levothyroxine, Tetraiodothyronine, etc.) replace the thyroid hormone, and blood test data on serum levels of free thyroxine help to adjust their dosage.
Estrogen deficiency is usually corrected by the use of oral contraceptives, and these hormones must be taken by women with Sheehan's syndrome until menopause.
Endocrinologists note that if the level of hormones in the blood is controlled, there are usually no side effects. Side effects may occur when the dose of hormonal drugs is too high or too low. Therefore, patients with this syndrome are monitored, undergo regular examinations and have blood tests for hormones.


 [
[