
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Pneumococcal meningitis: symptoms, diagnosis, treatment
Medical expert of the article
Last reviewed: 12.07.2025
In addition to inflammation of the lungs and pleura, middle ear and paranasal sinuses, soft tissues and joints, pneumococcal infection can cause an inflammatory process in the soft meninges – pneumococcal meningitis. According to ICD-10, the code for this type of bacterial meningitis is G00.1. [ 1 ]
Epidemiology
Meningococcal infection occurs everywhere, but according to the World Health Organization, the highest incidence of bacterial meningitis (10 cases per thousand people) is found in sub-Saharan Africa, the so-called “meningitis belt.”
At the same time, pneumococcal meningitis in children under five years of age is estimated at 17 cases per 100 thousand worldwide.
The CDC estimates that there are 150,000 hospitalizations for pneumococcal pneumonia in the United States each year.[ 2 ]
And its fatality rate in some regions of the world exceeds 73%.
Pneumococcal meningitis accounts for 61% of meningitis cases in Europe and the United States. [ 3 ]
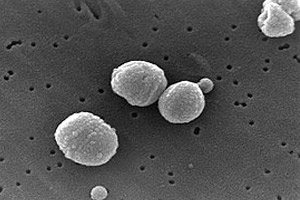
Causes pneumococcal meningitis
The causes of this type of meningitis are gram-positive alpha-hemolytic bacteria Streptococcus pneumoniae of several serotypes, called pneumococci. Along with meningococci (Neisseria meningitidis), pneumococci are recognized as the most common causative agent of bacterial meningitis and the most common cause of bacterial, in particular, pneumococcal meningitis in adults. And up to a quarter of all cases of pyogenic meningitis of bacterial origin are purulent pneumococcal meningitis.
Inflammation of the membranes of the brain caused by pneumococcal infection may be a consequence of its spread from the upper respiratory tract, lungs, middle ear, paranasal sinuses by the hematogenous route (with the bloodstream). The presence of bacteria in the systemic bloodstream - pneumococcal bacteremia - leads to their entry into the cerebrospinal fluid (cerebrospinal fluid), and with it - into the soft membranes of the brain.
In addition, damage to the meninges is possible with direct penetration of infection into the brain - as a result of TBI with a skull fracture.
Risk factors
Widespread asymptomatic nasopharyngeal carriage of S. pneumoniae (15% in children under 2 years of age, 49.6% in children aged 2 to 5 years, 35.4% in children over 5 years of age) is considered a serious prerequisite for pneumococcal inflammation of the cerebral membranes in children. [ 4 ]
Also recognized risk factors for its development are:
- old age;
- weakened immune system (including HIV and people with a removed or non-functioning spleen);
- recently suffered pneumococcal otitis media, pneumonia, pharyngitis, tonsillitis, sinusitis (frontal, sphenoid sinus, maxillary sinus, ethmoid labyrinth);
- diabetes mellitus;
- renal and/or hepatic insufficiency;
- alcohol abuse. [ 5 ], [ 6 ]
Pathogenesis
How is pneumococcal meningitis transmitted? Transmission of S. pneumoniae, which inhabits the respiratory tract, occurs as a result of direct contact through airborne droplets (during coughing and sneezing). But pneumococcal meningitis itself is not considered contagious.
The pathogenesis of pneumococcal infection is caused by their toxin pneumolysin and antigens, which allow the infection to defend itself from the cellular immune system of the nasopharyngeal mucosa.
The interaction of bacterial cells with human tissues (primarily the epithelium of the mucous membranes of the respiratory tract) is ensured by carbohydrate phosphate-containing heteropolymers of the bacterial cell wall in the form of teichoic acid.
Following epithelial adhesion, bloodstream invasion follows, and proinflammatory mediators are released into the blood – IL-1-β, TNF-α, MIP class macrophages, etc.
In this case, the release of inflammatory mediators and binding to extracellular matrix glycoproteins facilitates the penetration of S. pneumoniae through the blood-brain barrier (BBB) into the brain. In addition, the destruction of the BBB enhances the effect of pneumococci on vascular endothelial cells and increases the production of chemically active forms of nitrogen by their enzymes. Pneumococcal surface protein C can bind receptors of laminin, an adhesive glycoprotein of the basal membranes of endothelial cells of the brain's microvessels.
The bacteria then freely multiply and activate circulating antigen-presenting cells and neutrophilic granulocytes (microglial cells) of the brain, increasing the intensity of the inflammatory process in the soft cerebral membranes. Details on pathogenesis [ 7 ]
Symptoms pneumococcal meningitis
The first signs of pneumococcal meningitis are manifested by severe hyperthermia (with a body temperature of up to +39°C) and a sudden headache.
Other symptoms quickly appear, including: nausea and vomiting, weakness, increased sensitivity to light, stiffness of the neck muscles, convulsions, rapid breathing, agitation and anxiety, and impaired consciousness. Cerebrospinal fluid leakage is possible. In infants, a bulging fontanelle area and an unusual posture with the head and neck arched backwards (opisthotonus) are noted.
Read more in the publication – Symptoms of meningeal syndrome
Complications and consequences
Pneumococcal meningitis can cause severe consequences and complications in the form of: [ 8 ]
- subdural effusion;
- accumulation of fluid inside the skull (hydrocephalus) (16.1%), which leads to increased intracranial pressure and diffuse cerebral edema (28.7%);
- convulsive syndrome; (27.6%)
- hearing loss; (19.7%)
- vision loss;
- mental retardation (indicating changes in the hippocampus);
- behavioral and emotional problems;
- paralysis.
Inflammation that affects the cavity between the soft and arachnoid membranes of the brain (subarachnoid space) often leads to the development of inflammation of the brain tissue - encephalitis or inflammation of the cerebral ventricles - ventriculitis. [ 9 ], [ 10 ]
Diagnostics pneumococcal meningitis
In addition to examination and recording of existing symptoms, diagnosis of pneumococcal inflammation of the meninges requires laboratory tests.
The following tests are required: PCR blood test, [ 11 ] serological blood test – for antibodies to pneumococcus in the blood serum, as well as a general analysis of cerebrospinal fluid (CSF) (white blood cell count (WBC) with differentiation, total protein), blood glucose (or CSF glucose), which are used in combination with the medical history and epidemiology to confirm possible diagnoses). [ 12 ]
Instrumental diagnostics include computed tomography or magnetic resonance imaging of the brain and encephalography. [ 13 ], [ 14 ]
Differential diagnosis
Differential diagnosis is carried out, first of all, with meningitis of fungal and viral etiology, reactive and parasitic meningitis, as well as cerebral tumors and neurosarcoidosis.
Who to contact?
Treatment pneumococcal meningitis
Treatment of meningitis caused by pneumococcal infection involves parenteral administration of antibiotics. [ 15 ]
Antibiotic susceptibility testing shows which antibiotics will be most effective in treating a bacterial infection.[ 16 ]
Rehabilitation after pneumococcal meningitis lasts quite a long time, and patients who have had it are registered with a neurologist for at least 12 months. And in case of severe complications, disability is granted.
Prevention
An effective measure for the prevention of bacterial meningitis of this etiology is vaccination against pneumococcal infection with conjugate (PCV) and polysaccharide vaccines (PPV). [ 17 ]
The CDC recommends that all children under age 2 and all adults age 65 and older be vaccinated.[ 18 ]
Forecast
It is difficult to call the prognosis of this disease favorable, since, despite advances in medicine, mortality among patients with pneumococcal meningitis is higher than among patients with meningococcal meningitis (30% versus 7%). In 34% of episodes, the outcome was unfavorable. Risk factors for unfavorable outcome were older age, presence of otitis or sinusitis, absence of rash, low Glasgow Coma Scale score on admission, tachycardia.

