
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Encephalitic meningitis: causes, symptoms, treatment
Medical expert of the article
Last reviewed: 12.07.2025
According to medical terminology, encephalitic meningitis is more correctly called meningoencephalitis, since in this infectious disease the inflammatory process affects not only the membranes of the brain, but also its substance. [ 1 ]
Epidemiology
As clinical statistics show, in half of the cases the etiologic agent of meningoencephalitis is not identified.
Meningitis and encephalitis caused by Listeria occurs in 20% of cases in newborns and the elderly, and the mortality rate is 22%.
Tuberculous meningitis and encephalitis account for approximately 6% of all cases of extrapulmonary tuberculosis, but it is the most severe extrapulmonary form of the disease with a high mortality rate. [ 2 ]
In the case of rubella, encephalitic meningitis is considered by specialists to be a neurological complication, the frequency of which does not exceed one case per five thousand patients.
Herpesvirus meningoencephalitis accounts for about 10% of all cases of this disease. The annual incidence of herpes simplex encephalitis is approximately 2 to 4 cases per 1,000,000 population worldwide. Only a third of cases of brain membrane and tissue damage are the result of initial infection with HSV types 1 and 2; in the remaining cases, encephalitic meningitis is associated with the activation of a latent infection already present in the body. [ 3 ]
Causes encephalitic meningitis
Viral, bacterial, fungal and parasitic infections are the main causes of encephalitic meningitis. [ 4 ]
Viral inflammation of the membranes of the brain (meninges) with a simultaneous inflammatory process in the brain substance (cerebrum materia) can be provoked by:
- herpes simplex viruses HSV1 and HSV2 (genital); [ 5 ]
- Varicella zoster virus (VZV3) – chickenpox virus; [ 6 ]
- Rubella virus (RuV) of the Matonaviridae family – rubella virus; [ 7 ]
- measles virus (Morbilli virus ); [ 8 ]
- RNA arbovirus of the Flaviviridae family – tick-borne encephalitis virus (or arbovirus). [ 9 ], [ 10 ]
Bacterial meningoencephalitis can be caused by meningococci (Neisseria meningitidis), listeria (Listeria monocytogenes), Mycobacterium tuberculosis bacteria (the causative agent of tuberculosis), and also by pale treponema (Treponema pallidum), which leads to the development of syphilis. At the same time, gradually developing encephalitic meningitis in tuberculosis is, in fact, one of its extrapulmonary forms – tuberculosis of the nervous system, and brain damage by T. pallidum can be defined as syphilitic meningoencephalitis, meningovascular syphilis or neurosyphilis. [ 11 ], [ 12 ]
Fungal infections associated with brain damage include naturally occurring cryptococci (Cryptococcus neoformans) and, in rare cases, endemic fungal infections such as Histoplasma capsulatum, which most often cause pulmonary mycosis. However, according to some data, CNS damage is observed in 5-10% of cases of disseminated histoplasmosis. [ 13 ], [ 14 ], [ 15 ]
Parasitic protozoa that can infect humans and cause meningoencephalitis include:
- freshwater inhabitant Naegleria fowleri - a unicellular amoeba Naegleria f owleri of the Percolozoa type;
- Toxoplasma gondii, which can be contracted through contact with food or cat feces containing oocysts of this intracellular parasite.
Risk factors
The key risk factors for the development of meningoencephalitis are caused by problems with the immune system: a weakening of the body's defenses.
In turn, immunity decreases when fighting frequent infections of various localizations, in the presence of foci of chronic infection (for example, in the middle ear, paranasal sinuses) or progressive neoplasms, immediately after vaccinations, in connection with anti-cancer and immunosuppressive therapy.
The risk of developing such inflammation is increased in newborns and children in the first years of life, the elderly, pregnant women, patients with HIV, as well as in those with existing autoimmune diseases, severe organ dysfunction, and diabetes.
The risk of neurosyphilis, like tuberculous meningoencephalitis, is increased in cases where the disease is not treated in the early stages.
Swimming in fresh water (including in water parks) increases the risk of invasion by the amoeba Naegleria f owleri with the development of protozoal meningoecephalitis, especially in children.
Pathogenesis
When answering the question of whether encephalitic meningitis is contagious or not, experts point out that a person can become infected with viruses (mentioned earlier) from someone else, but encephalitis itself is not transmitted from person to person.
But meningococci (Neisseria meningitidis) can be contracted from a sick person - during the prodromal period of meningoencephalitis (which lasts 4-6 days). In syphilitic meningoencephalitis, damage to the membranes and tissues of the brain is the result of reactivation of treponema during untreated syphilis (which is transmitted sexually and through household contact). Although the pathogenesis of neurosyphilis has not been fully studied, it is assumed that the infection, spreading through the blood and lymph, can accumulate in tissues adjacent to the vessels, followed by inflammation and obliteration (narrowing of the lumen) of the vessels that supply blood to the brain and its membranes.
Listeria can be contracted through contaminated food products. These bacteria infect blood and lymph leukocytes, and with them, overcoming the blood-brain barrier, penetrate the brain. There they multiply, forming granulomas, which leads to focal tissue necrosis.
Viral virions, when in contact with cells of the mucous membranes, attach to receptors on their surface and – through phagocytosis, direct release of genomic nucleic acids or fusion of the viral capsid with the host cell membrane – damage tissues, causing a protective antigen reaction in the form of inflammation.
Tick-borne encephalitis virus is transmitted by transmission: by bites of ixodid ticks. And the pathogenesis lies in the dystrophy of brain neurons and their necrosis as a result of the virus penetrating into the general bloodstream through the vascular endothelium, the cells of which are damaged by viral cytolytic enzymes. Having entered the cerebrospinal fluid, the virus attacks the meninges and neuroglia.
Cryptococci, as well as histoplasma spores, enter the body with inhaled air, and their mechanism of action is due to the damage to phagocytic cells, inside which the infection passes through the BBB (microbiologists call this path the Trojan horse mechanism), penetrates the blood and cerebrospinal fluid, and then into the brain, where the fungi continue to multiply, forming colonies.
When water infected with Naegleria fowleri trophozoites enters the nasal cavity, the infection lingers on the olfactory epithelium, affecting its receptors and penetrating through the cranial olfactory nerve behind the cribriform plate of the bone between the nasal and cranial cavities, and then into the cerebral membranes and tissues. Amebic trophozoites absorb brain tissue cells, destroying them with a whole set of their enzymes.
Symptoms encephalitic meningitis
Depending on the pathogen of encephalitic meningitis, its first signs appear after different times and are expressed with different intensity. Most often, these are weakness, general malaise, headache and a sharp increase in temperature (˂ +39°C).
Next, stiffness (rigidity) of the neck muscles, sensitivity to bright light, blurred vision and double vision, problems with speech or hearing appear.
Symptoms of tick-borne meningoencephalitis begin one to three weeks after the tick bite (often people simply do not notice it) and may include headache, fever, myalgia and arthralgia, nausea, confusion. This is followed by seizures, loss of sensation or paralysis of certain areas of the face or body; patients may fall into a coma. [ 16 ]
Meningoencephalitis caused by HSV1 also begins with headache and fever for 5-6 days, followed by tremors and seizures, muscle weakness, hallucinations, and disturbances of consciousness and behavior.
Hemorrhagic inflammation of the cerebral membranes and tissues in amoebic meningoencephalitis develops rapidly, in most cases with a fatal outcome.
When Listeria monocytogenes is present, purulent encephalitic meningitis may develop with subcortical abscesses in structures such as the thalamus and medulla oblongata.
Encephalitic meningitis in children in the first year of life is manifested by symptoms such as fever, lethargy, failure to wake up for feeding, vomiting, spasticity of the skeletal muscles of the body, irritability, and bulging of the anterior fontanelle. [ 17 ]
Complications and consequences
Encephalitic meningitis is dangerous due to its complications and consequences, [ 18 ] which include:
- hydrocephalus leading to intracranial hypertension;
- damage to the cranial nerves, which leads to problems with speech, swallowing, vision, hearing, coordination of movements, memory;
- formation of an intracerebral cyst;
- convulsions of varying intensity, including generalized ones;
- shutdown of cerebral cortex functions with the development of apallic syndrome.
- memory problems, personality and behavior changes, speech and language problems
Children experience mental and psychological development disorders, and with herpesvirus etiology of inflammation, the tissues of the frontal lobes of the brain are often affected, causing behavioral and personality changes.
The consequences of syphilitic meningoencephalitis (neurosyphilis) are tabes dorsalis, general paresis, spastic and progressive paralysis, ophthalmological disorders, and partial loss of cognitive abilities.
Lower motor neuron damage and spinal arachnoiditis—in addition to gait disturbances and cognitive changes—are severe complications of cryptococcal meningoencephalitis.
Due to severe swelling and damage to the brain, coma develops in encephalitic meningitis, for more details see – Cerebral coma.
Diagnostics encephalitic meningitis
The earlier meningoencephalitis is diagnosed, the sooner it can be treated, increasing the patient's chance of recovery.
First of all, an examination is carried out, anamnesis is collected and clinical symptoms are identified. The following tests are taken: general blood test, blood test for antibodies (IgM and IgG) to viruses, for RW; serological analysis of blood serum; general, PCR and microbiological analysis of cerebrospinal fluid (CSF) - to determine the type of pathogenic infection.
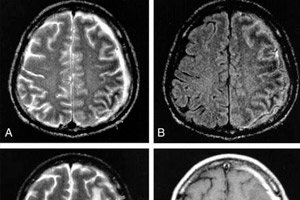
Instrumental diagnostics are used: neuroimaging using computed tomography of the brain or magnetic resonance imaging (MRI), and electroencephalography (EEG) for monitoring the electrical activity of the brain. [ 19 ]
Differential diagnosis
Differential diagnosis includes viral encephalomyelitis, autoimmune encephalitis, meningeal carcinomatosis, CNS vasculitis, etc. It is also important to differentiate viral and bacterial (or fungal) meningoecephalitis.
Who to contact?
Treatment encephalitic meningitis
Treatment of meningoencephalitis, like treatment of meningitis, involves eliminating the underlying cause, relieving symptoms, and supporting bodily functions. Typically, inflammation of the membranes and tissues of the brain is treated in an intensive care unit. [ 20 ]
How to treat meningococcal meningoecephalitis, read in the publication - Meningococcal infection
Read more about the treatment of listeriosis meningoencephalitis with antibiotics in the article - Listeriosis
In cases of tuberculous etiology of inflammation, the antibiotic Rifampicin ( Macox ) is used, and in cases of neurosyphilis, Penicillin and Ceftriaxone (Cefamed, Triaxone).
In case of encephalitic meningitis of viral etiology, glucocorticosteroids are administered, for example, Dexamethasone. And if meningoencephalitis is caused by HSV1, HSV2 or Varicella zoster viruses, the antiviral drug Acyclovir or Ganciclovir is administered parenterally.
Cryptococcal meningoencephalitis is treated in the same way as cryptococcal meningitis: with the polyene antibiotic Amphotericin B and the fungicide Flucytosine.
Liposomal Amphotericin B is also used to treat encephalitic meningitis caused by Histoplasma; then long-term administration of the fungicidal drug Itraconazole (Itracon, Sporagal) in capsule form or Ketoconazole tablets is prescribed.
The annual incidence of herpes simplex encephalitis is approximately 2 to 4 cases per 1,000,000 population worldwide. Only one third of cases of brain membrane and tissue damage are the result of initial infection with HSV types 1 and 2; in the remaining cases, encephalitic meningitis is associated with the activation of an already latent infection in the body.
In addition, intensive therapy is provided through intravenous infusions to maintain body functions and relieve symptoms.
Prevention
Fortunately, the prevention of encephalitic meningitis is not limited to observing personal hygiene rules and using tick repellents, which can prevent infectious infection. [ 21 ]
There are effective vaccines, so you need to get vaccinated against tick-borne encephalitis, chickenpox, and meningococcal infection.
Forecast
Not all cases of encephalitic meningitis have a good prognosis: it varies depending on the specific infection, the severity of the disease, and the timeliness of treatment.
In mild cases and with little or no symptoms, patients recover within a few weeks, although it may take months to resolve the neurological sequelae. [ 22 ]
In severe cases, irreversible brain damage or death are possible. The fatal outcome in cases of inflammation of the cerebral membranes and tissues is estimated at approximately 10%, in cases of encephalitic meningitis caused by HSV - at 20%, and in cases of brain damage by the amoeba Naegleria fowleri - at almost 98%.

