
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
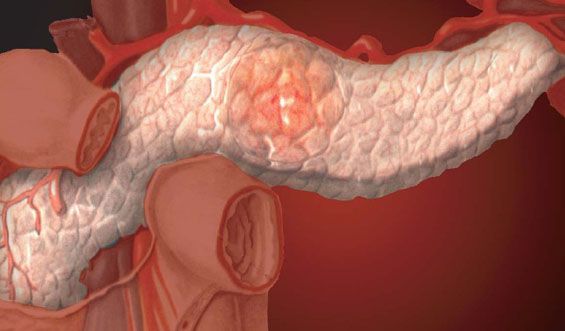
Chronic pancreatitis
Medical expert of the article
Last reviewed: 12.07.2025
Chronic pancreatitis is a persistent inflammation of the pancreas that results in permanent structural damage with fibrosis and duct strictures, accompanied by a decrease in exocrine and endocrine function. Chronic pancreatitis may be caused by chronic alcohol abuse, but may also be idiopathic.
Read also: Acute pancreatitis in adults
Initial symptoms of chronic pancreatitis include recurrent attacks of pain. Later, some patients develop glucose intolerance and malabsorption. The diagnosis is usually established by instrumental examination - ERCP, echosonography and studies of the secretory function of the pancreas. Treatment of chronic pancreatitis is symptomatic and includes an appropriate diet, analgesics and the use of enzymes. In some cases, surgical treatment is indicated.
ICD-10 code
- K86.0 Chronic pancreatitis of alcoholic etiology
- K86.1 Other chronic pancreatitis.
What causes chronic pancreatitis?
In the United States, 70-80% of cases are due to alcoholism and 15-25% are idiopathic. Rare causes of chronic pancreatitis include hereditary pancreatitis, hyperparathyroidism, and common pancreatic duct obstruction caused by stenosis, stones, or cancer. In India, Indonesia, and Nigeria, idiopathic calcific pancreatitis occurs in children and young adults ("tropical pancreatitis").
Similar to acute pancreatitis, the mechanism of disease development may be related to duct obstruction by protein plugs. Protein plugs may result from excess secretion of glycoprotein-2 or deficiency of lithostatin, a pancreatic juice protein that inhibits calcium precipitation. If obstruction is chronic, persistent inflammation leads to fibrosis, dilation, and fragmentary duct strictures with subsequent calcification. Neuronal sheath hypertrophy and perineuronal inflammation develop and may contribute to chronic pain. After several years, progressive fibrosis leads to loss of exocrine and endocrine function. Diabetes develops in 20-30% of patients within 10-15 years of disease onset.
Symptoms of chronic pancreatitis
Most patients experience episodic abdominal pain. In approximately 10-15%, left flank pain is absent and malabsorption develops. The pain is severe, localized to the epigastrium, and may last for hours or days. Episodes of pain usually resolve spontaneously after 6-10 years due to progressive destruction of the acinar cells that secrete pancreatic digestive enzymes. When lipase and protease secretion decreases to less than 10% of normal, the patient develops steatorrhea, manifested by fatty stools or even fat droplets and creatorrhea. At this time, signs of glucose intolerance may appear.
Where does it hurt?
What's bothering you?
Diagnosis of chronic pancreatitis
Diagnosis may be difficult because amylase and lipase levels are often normal due to severely reduced pancreatic function. In patients with a typical history of alcohol abuse and recurrent episodes of acute pancreatitis, the detection of pancreatic calcifications on plain abdominal radiography may be sufficient for diagnosis. However, such calcifications usually occur late in the disease course and these features are present in only about 30% of cases. In patients without a typical history, pancreatic malignancy as a cause of pain should be excluded: abdominal CT is recommended. CT may show calcifications and other glandular changes (eg, pseudocysts or dilated ducts), but these features may not be present in the early stages of the disease.
Initial workup of patients with normal CT scans includes ERCP, endoscopic echosonography, and pancreatic secretory function studies. These tests are quite sensitive, but ERCP can cause acute pancreatitis in approximately 5% of patients. MRCP may be an acceptable alternative.
Late in the course of the disease, exocrine pancreatic function parameters become abnormal. A 72-hour stool fat test can diagnose steatorrhea, but the test is not specific. The secretin test involves collecting pancreatic secretions through a duodenal tube for analysis, but this is performed in only a few centers. Serum trypsinogen and chymotrypsin and stool elastase levels may be decreased. The bentiromide and pancreolaurill tests involve oral administration of the agents and analysis of urine for breakdown products caused by pancreatic enzymes. However, all of these exocrine tests are less sensitive than ERCP or endoscopic ultrasonography in the early diagnosis of the disease.
What do need to examine?
How to examine?
Who to contact?
Treatment of chronic pancreatitis
Relapse of the disease requires treatment similar to that for acute pancreatitis, including fasting, intravenous fluids, and analgesics. After refeeding, the patient should avoid alcohol and consume only low-fat foods (< 25 g/day) (to reduce pancreatic enzyme secretion). H2 blockers or proton pump inhibitors can reduce acid-stimulated secretion of secretin and thus reduce pancreatic secretion. However, these measures often fail to relieve pain, requiring increased doses of opiates with the risk of addiction. Treatment of chronic pancreatic pain is often unsatisfactory.
Oral administration of pancreatic enzymes may reduce chronic pain by inhibiting cholecystokinin release and thereby decreasing pancreatic enzyme secretion. This approach is more likely to be successful in mild idiopathic pancreatitis than in alcoholic pancreatitis. Enzymes are also used to treat steatorrhea. Various preparations are effective, and a dose providing at least 30,000 U of lipase should be used. Acid-resistant tablets should be used and taken with food. H2 blockers or proton pump inhibitors should be given to prevent acid destruction of the enzymes.
Beneficial clinical effects include weight gain, decreased stool frequency, disappearance or reduction of steatorrhea, and improvement of general condition. The clinical effect of treatment can be documented by studies showing a decrease in stool fat after enzyme therapy. If severe steatorrhea persists despite treatment of chronic pancreatitis, medium-chain triglycerides (they are absorbed without pancreatic enzymes) can provide a source of fat, reducing other dietary fats proportionally. In addition to treatment, fat-soluble vitamins (A, D, K) should be prescribed, including vitamin E, which helps reduce inflammation.
Surgical treatment of chronic pancreatitis may be effective in the management of pain. A pancreatic pseudocyst causing chronic pain may be drained into an adjacent organ (eg, stomach) or into a disconnected loop of jejunum (by Roux-en-Y cystojejunostomy). If the main pancreatic duct is dilated more than 5-8 mm, lateral pancreaticojejunostomy (Puestow procedure) is effective in approximately 70-80% of patients. If the duct is not dilated, partial resection is effective; distal pancreatectomy (for significant involvement of the tail of the pancreas) or Whipple procedure (for involvement of the head of the pancreas) are also used. Surgical interventions should be reserved for patients who have abstained from alcohol and who are able to control secondary diabetes, which may be associated with pancreatic resection.
Some pseudocysts can be drained endoscopically. Endoscopically, under ultrasound control, it is possible to perform denervation of the solar plexus with alcohol and bupivacaine and thereby provide pain relief. In case of severe stricture of the papilla or distal pancreatic duct, ERCP with sphincterotomy, stenting or dilation can be effective.
Oral hypoglycemic agents are rarely effective in the treatment of diabetes caused by chronic pancreatitis. Insulin should be used with caution, as prolonged hypoglycemia may develop due to the deficiency of glucagon secretion by alpha cells and the lack of effect of its secretion on insulin-induced hypoglycemia.
Patients who have chronic pancreatitis are at increased risk for pancreatic cancer. Increasing symptoms of chronic pancreatitis, especially those associated with the development of a pancreatic duct stricture, require evaluation for malignancy. This may include cytologic analysis of a stricture scraping or determination of serum markers (eg, CA 19-9 carcinoembryonic antigen).
More information of the treatment


 [
[