
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
'Sugar disguise': Scientists find a way to protect beta cells in type 1 diabetes, borrowed from cancer
Last reviewed: 03.08.2025
Researchers at the Mayo Clinic have made a surprising discovery: a molecular mechanism by which cancer cells hide from the immune system can be used to protect insulin-producing beta cells in type 1 diabetes. The discovery raises the prospect of new treatments for the autoimmune disease, which affects about 1.3 million people in the United States.
Type 1 diabetes occurs when the immune system mistakenly attacks and destroys the beta cells of the pancreas. These cells produce insulin, a hormone that regulates blood sugar levels. Treatment currently involves lifelong insulin or islet cell transplantation with mandatory immune suppression.
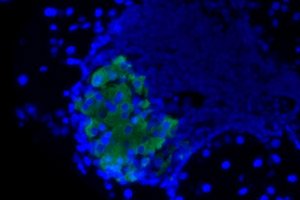
But a new study published in the Journal of Clinical Investigation suggests a different approach: engineered beta cells coated with a specific sugar molecule, sialic acid, become “invisible” to autoimmune attack without suppressing the immune system overall.
How does this work?
In previous work, a team led by Dr. Virginia Shapiro showed that tumor cells expressing the enzyme ST8Sia6 increase the amount of sialic acid on their surface. This “sugar coating” helps cancer hide from the immune system.
Now the scientists have applied the same principle to normal cells. In a model of type 1 diabetes, they genetically modified beta cells so that they synthesized ST8Sia6 on their own. As a result:
- such cells were protected from destruction in 90% of cases;
- the development of diabetes in predisposed animals was prevented;
- the immune system remained active and could fight other diseases.
What does it mean?
“We essentially ‘masked’ the beta cells so that they weren’t seen as an enemy by the immune system,” explains Dr. Shapiro. “Unlike immunosuppressants, which suppress immunity throughout the body, our approach provides localized and highly selective protection.”
According to the first author of the work, graduate student Justin Choe, it is important that the immune system was not “switched off” completely – B and T cells continued to function normally, and tolerance arose only in relation to beta cells.
Prospects
Currently, islet transplants require lifelong immunosuppressive treatment. The new technology could make such transplants safer by eliminating the need for immune suppression, thereby reducing the risk of infections and other side effects.
"Our goal is to create transplantable beta cells that won't be destroyed by the patient's immune system," adds Dr. Shapiro.
Although the research is still in the preclinical stage, the results open up a fundamentally new way to treat type 1 diabetes - not by eliminating the immune system, but by training it to leave the necessary cells alone.
