
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
AI detects a third of interval breast cancer cases missed by screening
Last reviewed: 03.08.2025
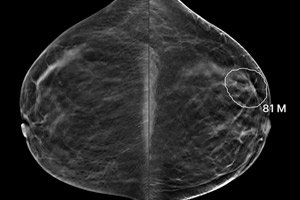
An artificial intelligence algorithm for breast cancer screening could improve the performance of digital tomosynthesis mammography (DBT), reducing interval cancer rates by up to one-third, according to a study published today in the journal Radiology.
Interval breast cancers are symptomatic tumors diagnosed between routine screening mammograms. These cases typically have a worse prognosis due to more aggressive disease and rapid tumor growth. DBT, or 3D mammography, provides improved visualization of breast lesions and can identify tumors that may be hidden by dense tissue. However, because DBT is a relatively new technology, long-term outcome data for patients at institutions that have recently adopted the technique remain limited.
“Given the paucity of breast cancer mortality data beyond 10 years of DBT screening, interval cancer rates are often used as a proxy,” explains study author Dr. Manisha Bahl, director of breast imaging quality at Massachusetts General Hospital and an associate professor at Harvard Medical School.
“A decrease in this rate suggests a decrease in breast cancer incidence and mortality.”
Study: AI identifies undetected tumors
In a study of 1,376 cases, Bal and colleagues retrospectively analyzed 224 interval cancers in 224 women who underwent DBT screening. In these images, the Lunit INSIGHT DBT v1.1.0.0 AI algorithm correctly localized 32.6% (73 of 224) of previously undetected tumors.
“We were surprised that almost a third of interval tumors were detected and accurately localized by the AI algorithm in mammograms that were previously interpreted as normal by radiologists, highlighting the potential of AI as a ‘second reader,’” Bahl said.
According to the researchers, this may be the first published study specifically looking at using AI to detect interval cancers on DBT images.
“AI has been used previously to detect interval cancers on conventional 2D digital mammograms, but to our knowledge, there have been no published studies in the literature on AI detection of interval tumors specifically on 3D tomosynthesis scans,” Bal explained.
Methodology: at the lesion level, not just a snapshot
To avoid overestimating the algorithm's sensitivity, Bal's team used a lesion-specific analysis: the AI was given a "scored hit" only if it correctly identified and localized the exact location of the tumor.
“In contrast, whole-image analysis can give the AI a ‘pass’ even if the annotation is incorrect, which artificially inflates sensitivity,” she adds.
“Focusing on the accuracy of lesion localization provides a more reliable assessment of the clinical performance of the algorithm.”
What exactly does AI find?
- Tumors detected by the algorithm tended to be larger
- More often they ended up with lymph node damage
- This could mean that AI primarily identifies aggressive or fast-growing tumors, or those that were already at an advanced stage but were missed by doctors during screening.
Overall results:
Among 1,000 patients (including both those with confirmed tumors and those with benign or false-positive results), AI:
- Correctly localized 84.4% of 334 true positive cases
- Correctly classified 85.9% of 333 true negatives
- Rejected as false 73.2% of 333 false positive cases
Conclusions and significance
“Our study showed that the AI algorithm could retrospectively detect and accurately localize nearly a third of interval breast cancers on DBT screening images, indicating its potential to reduce the incidence of interval cancers and improve screening outcomes,” said Dr. Bahl.
"Our results support the integration of AI into DBT workflows to improve the accuracy of cancer detection. However, the real impact will depend on the extent to which radiologists adopt and adapt AI in clinical practice, as well as testing its effectiveness in different clinical settings."
