
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Uterine myoma in menopause
Medical expert of the article
Last reviewed: 12.07.2025
Uterine fibroids during menopause are a very common pathology among older women. This disease occurs in every fifth woman of reproductive age and in every third woman in menopause. This is due to the fact that a woman's hormonal background changes throughout her life, which leads to such changes in the reproductive system. But do not be upset if this diagnosis is established, since this disease is benign with high treatment efficiency.
Causes menopausal uterine myomas
Uterine myoma or fibromyoma is a benign disease of the uterus, which is accompanied by high proliferative activity of myometrium cells with the formation of a volumetric structure in the uterine cavity. This disease is hormone-dependent, that is, the stimulus for such active reproduction is female sex hormones.
Therefore, the main reason can be considered to be hormonal imbalance, which occurs with the onset of menopause, so the development of these diseases is more typical for the climacteric period.
Pathogenesis
In pathogenesis, the main role in the development of uterine myoma during menopause belongs to the disturbance of hormone levels. During menopause, the level of estrogens falls, their regulatory effect on the first phase of the menstrual cycle decreases, which is accompanied by a decrease in the process of proliferation of endometrial cells. This, in turn, entails a compensatory increase in the proliferation of myometrial cells, which is accompanied by hyperplasia of these cells with the development of different types of uterine myoma. If connective tissue fibers predominate in the structure of a benign formation, then we speak of the concept of fibromyoma. Clinically, these two forms are no different, such differentiation is possible only according to histological examination data.
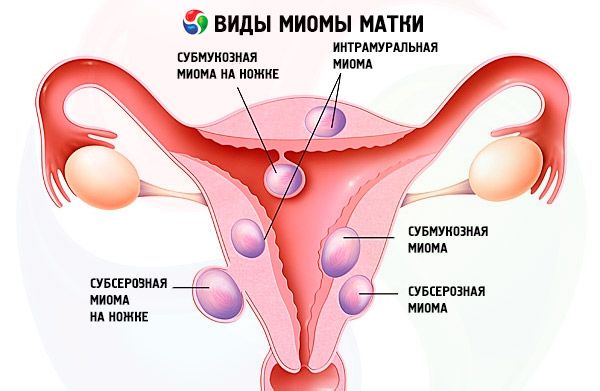
There is another series of reasons associated with the development of fibroids during menopause - this is a group of non-hormonal reasons. The basis of all these reasons is the natural physiological involution of myometrium cells during menopause in women, which is accompanied by changes in the metabolism of myocyte cells, their antigenic changes. In this case, normal processes of cell growth and reproduction with an increased tendency to proliferation can be disrupted, and specific cytokines and vascular growth factors are formed, which additionally stimulate pathological excessive differentiation of these cells. As a result, uncontrolled cell division, their reproduction and an increase in the volume of the myometrium occur, which can be local or diffuse. If the influence of etiological factors continues, then the fibroid grows rapidly and increases in size, which requires some kind of treatment tactics. Depending on where the primary focus of pathological cells that began their abnormal division is located, tumor growth can be diffuse - over the entire surface of the myometrium with uniform enlargement of the entire uterus, as well as local - then a myomatous node is formed. This node can also be located differently - submucous, subserous and intramurally, which affects the clinical features of the disease in these different forms. There can be a different number of such nodes, and depending on this, a single nodular myoma and multiple nodular myoma are distinguished.
These are the main pathogenetic mechanisms that influence the development of uterine fibroids during menopause.
Symptoms menopausal uterine myomas
Uterine myoma can begin in a woman even before the onset of the climacteric period, and with the onset of menopause, the clinical picture can actively manifest itself. Very often, uterine myoma is asymptomatic until the formation becomes enormous in size or until complications arise. Therefore, this diagnosis is often made at the peak of the clinical picture.
It is known that menopause has several stages in its course:
- premenopause – the period from 45 years to the onset of menopause;
- menopause – the period of the last menstruation, average age is about fifty years;
- postmenopause – the period from the last menstruation until the end of a woman’s life.
If uterine fibroids begin in the premenopausal period, then symptoms of menstrual irregularities may develop, which is associated with a disruption of the endometrium structure due to the presence of nodes or with initial changes in hormone levels. At this point, given her age, a woman may not pay due attention to such a condition, since these ovariomenstrual cycle disorders can be explained by the onset of menopause. But it should be remembered that in this case, on the contrary, it is necessary to consult a doctor so that he can confirm or refute thoughts about menopause. After all, early diagnostics of fibroids is much better treated.
The first signs of uterine fibroids during menopause can also be varied - bleeding, pain in the lower abdomen or a feeling of heaviness in the pelvis, impaired sexual intercourse, decreased libido, impaired bladder or rectal function, secondary chronic iron deficiency anemia. These symptoms often appear already with significant fibroid volumes precisely because the course is asymptomatic. There are some clinical features of uterine fibroids during menopause depending on the location and form of the formation.
In the nodular form of uterine myoma, clinical manifestations directly depend on the location of the node. When subserous nodes are formed, menstrual function is not impaired if it is preserved in premenopause. Acute abdomen is often observed, since such nodes are very labile in their position and can shift, forming a torsion or necrosis of the node stalk. Sometimes the pain is not sharp, but dull, aching, constant, if the node irritates the peritoneum or nerve endings, then there may also be heaviness in the abdomen. If the subserous myomatous node is of significant size, it can cause a syndrome of compression of adjacent organs with difficulty in the act of defecation with compression of the rectum, with difficulty in urination or reactivity of the bladder, and compression can also disrupt the outflow of venous blood and lymph with the formation of stagnation in the small pelvis and the development of hemorrhoids. Often, with a subserous location of a fibromatous node in uterine myoma during menopause, local neurological symptoms are observed due to compression of nerve structures with the development of disorders such as paresthesia or osteochondrosis of the lumbar spine. Then it is very important to correctly diagnose the pathology, and not treat these neurological disorders.
With a submucous location of the node, the clinical picture is less pronounced in terms of compression symptoms, but local manifestations are more pronounced. Metrorrhagia may be observed, even if there is no menstruation at all during menopause, then such discharge may appear with uterine myoma during menopause. These discharges are painful, accompanied by aching pain in the lower abdomen. Discharge with uterine myoma during menopause can also be in case of infection of the node, then infectious inflammation develops with yellow-green discharge with an unpleasant odor, which is also accompanied by symptoms of intoxication.
Another common localization of the uterine myoma node during menopause is intraligamentary - between the ligaments of the uterus and ovaries. In this case, the clinical picture of such a node will be accompanied by symptoms of compression of the ureters with the possible development of renal colic, hydronephrosis, pyelonephritis. Diagnosis of such a node is very problematic.
As for the diffuse form of uterine myoma, this form most often proceeds asymptomatically, which is associated with its location in the thickness of the entire myometrium and the same increase in the entire uterus. Then the uterus increases in size and the woman may feel an increase in the abdomen or unpleasant pressure in the small pelvis. Such myoma most often reaches large sizes and its treatment is then radical. Therefore, a comprehensive gynecological screening annual examination is necessary even during menopause.
These are the main clinical manifestations of uterine fibroids during menopause and attention should be paid to any such symptoms for timely diagnosis and treatment.
Where does it hurt?
Complications and consequences
The main complications that may occur with uterine myoma are bleeding with a submucous location of the myomatous node, which requires immediate medical action, infection of the myomatous node, which requires anti-inflammatory therapy. Complications may also occur in the form of the "birth" of a myomatous node located submucously or its necrosis, which is accompanied by symptoms of acute abdomen and requires immediate treatment and timely differential diagnostics.
 [ 12 ]
[ 12 ]
Diagnostics menopausal uterine myomas
Diagnosis of fibroids should be timely, therefore a comprehensive examination of the woman is necessary if this diagnosis is suspected. It is necessary to carefully collect anamnesis with details of complaints and an accurate definition of the obstetric anamnesis. It is necessary to find out when the climacteric period began, the characteristics of the menstrual cycle, the presence of an active sexual life. Then proceed to the examination.
During a bimanual examination of a woman, a tumor-like formation of various sizes and locations is determined, it is painless, mobile - in the case of a nodular uterine myoma. If the myoma is diffuse, then an increase in the entire uterus is observed, which corresponds to a certain period of pregnancy, the uterus is dense, slightly mobile and painless. These are the main objective examination methods that allow us to suspect this diagnosis with further additional research methods.
Instrumental diagnostics is the first choice in diagnosing uterine fibroids during menopause, which is due to the high information content of most methods.
Hysterography is one of the methods of special diagnostics, which is carried out by filling the uterus with a contrast fluid in the volume of 5-7 milliliters with subsequent registration of changes. In this case, a filling defect may be observed, which corresponds to the location of the node, as well as a decrease in the uterine cavity. Another examination is hysteroscopy. This is a special method of examining the uterine cavity with a special device with a video camera at the end, which allows you to see the uterine cavity, as well as conduct a biopsy with further examination of the puncture for accurate verification of the diagnosis.
The "gold standard" for diagnosing uterine fibroids during menopause is ultrasound examination. This method allows you to see an anechoic formation in the case of a myomatous node with an accurate determination of the location of this formation, its size, structure, as well as the degree of enlargement of the uterus in the case of a diffuse form of fibroids.
There are no specific tests for uterine myoma. General tests are performed to determine hemoglobin, hematocrit, and erythrocytes in chronic posthemorrhagic anemia, if the myoma is symptomatic, i.e. bleeding. If there is a suspicion of suppuration of the myomatous node, then the general blood test will determine characteristic changes in the form of leukocytosis, increased ESR, and a shift in the leukocyte formula to the left. Histological examination of a puncture of the myomatous node or postoperative formation is considered a special test. Such a study allows you to accurately establish a diagnosis, exclude its malignant nature, and clarify further treatment tactics.
What do need to examine?
Differential diagnosis
Differential diagnostics of uterine fibroids during menopause in case of clinical manifestation in the form of bleeding should be carried out with malignant tumors of the uterus - endometrial cancer. Endometrial cancer is characterized by the appearance of bloody discharge already several years after the onset of menopause. But uterine fibroids are characterized by periodic bleeding, and the node is clearly defined during examination. In case of doubts about the nature of the formation in the uterus, diagnostic curettage of the uterine cavity is carried out with histological examination of this material, which allows you to accurately determine the benign or malignant nature of the formation. Differential diagnostics should also be carried out with a uterine cyst. During ultrasound, the cyst has an anechoic structure, oval shape, clear edges with a thin capsule and uniform content. The myomatous node is also anechoic, but it is heterogeneous and corresponds to the myometrium in density, often has a stalk and is well supplied with blood, unlike a cyst, which is avascular.
Myomatous node also needs to be differentiated from internal endometriosis, which can also be accompanied by the formation of myomatous areas in the uterine cavity. But with endometriosis there is a characteristic anamnesis in the form of bleeding, which corresponds to menstruation, and uterine myoma during menopause does not have regular bleeding. These two diagnoses can be accurately verified using histology, because they can often be combined in one uterus.
Considering the period of menopause, that is, not a young age of a woman, it is necessary to carefully conduct diagnostics of uterine fibroids and differential diagnostics, since various malignant processes are possible at this age, which must be diagnosed as early as possible with the beginning of appropriate treatment.
Who to contact?
Treatment menopausal uterine myomas
Treatment of uterine fibroids during menopause can be medicinal, using special hormonal and non-hormonal drugs, as well as surgical, which has clear indications that are identified on an individual basis.
Conservative treatment is carried out in the following cases:
- a woman's desire for conservative treatment without surgical intervention;
- low-symptom or asymptomatic clinical course of the pathology;
- uterine myoma less than twelve weeks of pregnancy in case of intramural location and diffuse forms;
- slow growth of nodes or enlargement of the entire uterus;
- localization of the node is subserous or intramural on a wide base without complications and symptoms of compression of adjacent organs;
- uterine fibroids during menopause, which may be accompanied by a high risk of intraoperative complications;
- drug therapy as a preparatory stage for surgery or as part of complex treatment in the postoperative period.
Conservative treatment cannot be considered as an alternative to surgical treatment; if there are indications for surgical intervention, then it must be performed.
Among the drug treatments, non-hormonal and hormonal treatments are distinguished. Non-hormonal treatments include:
- symptomatic therapy in case of complications or pain syndrome, which includes hemostatics and uterotonics in case of bleeding, antispasmodics and NSAIDs in case of pain syndrome, iron preparations, vitamins and microelements in case of chronic posthemorrhagic anemia. Sedative therapy is recommended as a complex therapy in case of pain syndrome.
- Normalization of metabolism in myocytes – antioxidants, antiplatelet agents, and multivitamin complexes are used.
- Measures aimed at correcting those diseases that can contribute to the further development and enlargement of uterine fibroids - diffuse toxic goiter, concomitant inflammatory processes of the internal genital organs.
Hormonal therapy is used to reduce the size of myomatous nodes and regress clinical symptoms. Hormonal therapy for uterine myoma may include several groups of drugs:
- Gonadotropin-releasing factor agonists, of which Diphereline or Triptorelin is a representative, are used from the 3rd day of the menstrual cycle for six months at 3.75 milligrams.
- Goserelin - is used for six months at 3.6 milligrams subcutaneously
- Buserelin - 200 micrograms in the nose twice a day for a six-month course
- Zoladex – from the 1st to the 5th day of the cycle by injection.
- Gonadotropic hormone antagonists, a representative of which is the drug Danazol, are used at 400-800 milligrams per day, also with a course of treatment for six months.
- Progesterone series drugs are various drugs that are able to regulate the ovariomenstrual cycle in case of insufficiency of its second luteal phase. The main representatives of this series are:
- Norethisterone acetate – is used from the fifth day of the menstrual cycle, 5-10 milligrams twice a day for six months.
- Medroxyprogesterone acetate is used in the same dose and for the same course.
- The Mirena system is an intrauterine device that is inserted for five years with monitoring of its condition.
- Norcolut and Primolut are drugs that are used from the 16th to the 25th day of the menstrual cycle for three to six months.
It is also possible to use combined oral hormonal drugs, two-phase, with a large amount of progesterone.
It should be remembered that hormonal therapy can reduce the size of fibroids by regulating hormonal levels, but after the end of therapy, the fibroids may reach their previous size within a year.
Surgical treatment of uterine fibroids in some cases has its own priorities, and in some cases is the only indicated method of treatment. Indications for surgical treatment include:
- symptomatic uterine fibroids, which are accompanied by:
- hemorrhagic syndrome in the form of uterine bleeding or massive discharge;
- intense pain symptoms;
- signs of chronic posthemorrhagic anemia;
- signs of compression and dysfunction of adjacent organs - the bladder, nerves and blood vessels, rectum, ureters.
- The size of the fibroid is 12 weeks or more, even in the absence of any complaints.
- Submucous uterine myoma, regardless of its size, is accompanied by a high risk of complications, therefore it requires immediate surgical treatment without prior drug therapy.
- Rapid tumor growth during menopause can often be associated with the malignant nature of the process. The concept of "rapid growth" is an increase of 2-3 weeks in six months or 4-5 weeks in a year.
- Subserous nodes on a high pedicle due to possible complications in the form of pedicle torsion.
- Necrosis of myomatous node.
- The presence of nodes that are located in an atypical place - intraligamentary
- Nodes that grow from the vaginal part of the uterus due to frequent trauma.
- Combination of uterine fibroids during menopause with other pathologies of the internal genital organs, which also require surgical treatment - uterine and ovarian cysts, polyps, uterine prolapse
- Insensitivity of fibroids to hormonal treatment.
Surgical treatment can be performed in the scope of organ-preserving intervention and radical intervention. Tactics depend on the type of myoma, its size, location, and also the duration of the operation. Organ-preserving operations are myomectomy – removal of the myomatous node itself within healthy tissues – and embolization of the uterine arteries, which disrupts the blood supply to the node and it regresses.
Radical operations include supravaginal amputation of the uterus, subtotal hysterectomy and extirpation of the uterus, which also depends on the size and location of the fibroid and the woman’s age.
There are many traditional medicine methods for treating uterine fibroids during menopause.
The main ones are:
- Aloe leaves, which have a pronounced anti-inflammatory and regenerating effect, are squeezed into a glass and, after wetting a tampon, inserted into the vagina, repeating the procedure once a day for a whole month.
- The membranes or shells of walnuts must be crushed, poured with boiling water and infused for 20 minutes, then boiled over the fire for another 10 minutes and allowed to cool. This decoction should be taken orally three times a day, one tablespoon at a time, for at least a week.
- Burdock juice is excellent for relieving irritation, swelling and has an antiproliferative effect, which increases the ability of the cyst to resolve. To do this, squeeze the juice out of the pre-washed burdock leaves and take one teaspoon three times a day for five days, and then one teaspoon twice a day for another five days.
- Honey has the ability to increase local immunity and stimulate regeneration. To create a medicine from honey, you need to take the core of the onion and place it in a glass of honey so that it is completely filled with it. Leave this solution overnight and in the morning soak a tampon in this solution and insert it into the vagina overnight, repeat this for 10 days, after which the fibroid should decrease.
- Prepare a herbal infusion from currant, nettle, burdock and meadowsweet leaves - take them in equal quantities, pour hot water over them and boil for another 5 minutes, then cool and drink warm, half a glass every other day for a month.
Homeopathic remedies are also used to treat this pathology. Their main effect is aimed at regulating normal hormonal levels, which helps reduce the size of uterine fibroids.
The main homeopathic remedies are:
- Cyclodinone is a homeopathic preparation that normalizes the ovariomenstrual cycle in case of insufficiency of its second phase. The preparation is used 1 tablet in the morning or 40 drops once a day. The course of treatment is not less than three months.
- Dysmenorm is a complex homeopathic preparation that affects hormonal imbalance, including benign uterine formations. The preparation is used 1 tablet 3 times a day half an hour before meals.
Prevention
A method of specific prevention of the development of uterine fibroids is the prevention of the formation of conditions of hormonal homeostasis, in which local hyperestrogenism occurs:
- prevention of ectopic pregnancy;
- constant prevention of chronic stressful situations that contribute to metabolic and ovarian-menstrual cycle disorders;
- timely diagnosis and correction of second ovarian phase insufficiency;
- timely and adequate treatment of ovarian and uterine diseases of inflammatory and non-inflammatory etiology;
- timely correction of hormonal imbalances associated with dysfunction of the hypothalamic-pituitary-ovarian system.
In order to prevent precancerous diseases and tumors of the uterus, it is recommended that women under 30 undergo preventive examinations once a year, and after 30 years - twice a year with a cytological examination of the contents of the cervical canal, ultrasound, and timely treatment of identified diseases.
Forecast
The prognosis for recovery from uterine fibroids is unfavorable, since the fibroid itself is not capable of complete regression, but for life it is favorable, since it does not become malignant and is not dangerous with proper treatment.
Uterine fibroids during menopause are a pathology that often proceeds asymptomatically, but regular preventive examinations allow for timely diagnosis. Sometimes there are serious complications that need to be prevented by timely treatment of uterine fibroids, especially during menopause. Treatment of uterine fibroids during menopause can be medicinal and surgical, which is decided individually in each case. Sometimes complex treatment is used in the form of a combination of several methods. It is necessary to take care of your health and promptly contact a doctor if you have any complaints.

