
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Temporal lobe epilepsy in adults and children
Medical expert of the article
Last reviewed: 12.07.2025
Among the numerous types of epilepsy – a chronic disorder of the central nervous system with paroxysmal manifestation of symptoms – temporal epilepsy stands out, in which epileptogenic zones or areas of local attachment of epileptic activity are located in the temporal lobes of the brain.
Temporal lobe epilepsy and genius: reality or fiction?
The fact that temporal lobe epilepsy and a genius mind are somehow interconnected has no strictly scientific basis. Only individual facts and their coincidence are known…
Some researchers explain the visions and voices that Joan of Arc saw and heard by her epilepsy, although during the 20 years she lived, her contemporaries did not notice any oddities in her behavior, except that she managed to turn the tide of French history.
But a similar diagnosis of Frederic Chopin, who, as is known, had serious health problems, is suggested by his visual hallucinations. The brilliant composer remembered his attacks very well and described them in correspondence with friends.
The Dutch painter Vincent van Gogh also suffered from epilepsy, and at the end of 1888 – at the age of 35 and with his ear cut off – he was admitted to a psychiatric hospital, where he was diagnosed with temporal lobe epilepsy. After this, he lived for only two years, deciding to commit suicide.
Alfred Nobel, Gustave Flaubert, and, of course, F.M. Dostoevsky, in whose works many characters were epileptics, starting with Prince Myshkin, suffered from temporal lobe epilepsy seizures in childhood.
Epidemiology
Unfortunately, there is no information on the prevalence of temporal lobe epilepsy, since confirmation of the diagnosis requires a visit to a doctor and preliminary visualization of the brain with appropriate examination.
Although, as statistics from specialized clinics show, among focal (partial or focal) epilepsies, temporal lobe epilepsy is diagnosed more often than other types of this disease.
About half of all patients are children, since this type of chronic neuropsychiatric disorder is usually diagnosed in childhood or adolescence.
Causes temporal lobe epilepsy
Clinically based and scientifically proven causes of temporal lobe epilepsy correlate with structural damage in the temporal lobes of the brain (Lobus temporalis).
This primarily applies to the most common type of neuropathological damage – hippocampal sclerosis or mesial temporal sclerosis, which involves the loss of neurons in certain structures of the hippocampus, which controls information processing and forms episodic and long-term memory.
Recent MRI imaging studies have shown that temporal lobe epilepsy in children is associated with mesial temporal sclerosis in 37-40% of cases. Temporal lobe epilepsy in adults, which has the same etiology, is observed in approximately 65% of patients.
In addition, this type of epilepsy can be provoked by dispersion of the granule cell layer in the dentate gyrus of the hippocampus (Gyrus dentatus), which is associated with a decrease in the production of reelin, a protein that ensures the compactness of these cells, regulating the migration of neurons during embryonic brain development and subsequent neurogenesis.
Often, the cause of epileptic activity of the temporal lobes are cerebral cavernous malformations, in particular, cavernous angioma or angioma of the brain - a congenital benign tumor formed by abnormally dilated blood vessels. Because of it, not only the blood circulation of brain cells is disrupted, but also the passage of nerve impulses. According to some data, the prevalence of this pathology is 0.5% of the population, in children - 0.2-0.6%. In 17% of cases, the tumors are multiple; in 10-12% of cases, they are present in the family, which may cause familial temporal epilepsy.
Sometimes damage to the lobus temporalis structure is caused by heterotopia of the gray matter, a type of cortical dysplasia (abnormal localization of neurons) that is congenital and can be either a chromosomal abnormality or the result of exposure of the embryo to toxins.
Risk factors
Neurophysiologists see the main risk factors for the development of functional disorders of the temporal lobe of the brain in the presence of congenital anomalies that affect the functions of neurons and brain damage in infants during childbirth (including due to asphyxia and hypoxia).
In both adults and children, the risk of developing secondary temporal lobe epilepsy is increased by traumatic brain injury, infectious lesions of brain structures in meningitis or encephalitis, and parasitic infestations (Toxoplasma gondii, Taenia solium), as well as cerebral neoplasms of various origins.
Among the toxins that negatively affect the developing brain of the fetus, alcohol holds the undisputed “leadership”: the future child, whose father abuses alcohol, develops a deficiency of gamma-aminobutyric acid (GABA), an endogenous neurotransmitter of the central nervous system, which inhibits excessive excitation of the brain and ensures a balance of adrenaline and monoamine neurotransmitters.
Pathogenesis
Millions of neurons, which control all functions of the body, constantly change the electrical charge on their membranes and send nerve impulses to receptors - action potentials. The synchronized transmission of these bioelectric signals along nerve fibers is the brain's electrical activity.
The pathogenesis of temporal epilepsy lies in the disruption of its synchronization and the appearance of local zones with abnormally increased - paroxysmal - neuronal activity. When considering this disease, it should be borne in mind that attacks of electrical hyperactivity are initiated by several zones in the temporal lobes, namely:
- the hippocampus and amygdala, located in the medial temporal lobe and part of the limbic system of the brain;
- centers of the vestibular analyzer (located closer to the parietal lobe);
- the center of the auditory analyzer (Herschl's convolution), the abnormal activation of which causes auditory hallucinations;
- Wernicke's area (near the superior temporal gyrus), responsible for speech comprehension;
- poles of the temporal lobes, when overexcited, self-awareness changes and the perception of the environment is distorted.
Thus, in the presence of hippocampal or mesial temporal sclerosis, a portion of the pyramidal neurons in the CA fields (cornu ammonis) and the subiculum area (subiculum), which receive the action potential for transmitting nerve impulses further, are lost. Disruption of the structural organization of the cells of this part of the temporal lobe leads to expansion of the extracellular space, abnormal diffusion of fluid and proliferation of neuroglial cells (astrocytes), as a result of which the dynamics of synaptic impulse transmission changes.
In addition, it was found that the shutdown of the control over the rate of transmission of action potentials to target cells may depend on the deficiency in the hippocampal and neocortical structures of fast-growing interneurons - multipolar GABAergic interneurons, necessary for the creation of inhibitory synapses. Also, studies of the biochemical mechanisms of epilepsy led to the conclusion about the involvement in the pathogenesis of temporal epilepsy of two more types of neurons present in the hippocampus, subiculum and neocortex: striatal (stellate) non-pyramidal and pyramidal interneurons and smooth non-pyramidal. Striatal interneurons are excitatory - cholinergic, and smooth ones are GABAergic, that is, inhibitory. It is believed that their genetically determined imbalance may be associated with both idiopathic temporal epilepsy in children and a predisposition to its development.
And dispersion or damage of granule cells in the dentate gyrus of the hippocampus entails pathological changes in the density of the dendritic layer. Due to the loss of cells of the processes of neurons, synaptic reorganization begins: axons and mossy fibers grow to connect with other dendrites, which increases the excitatory postsynaptic potential and causes hyperexcitability of neurons.
Symptoms temporal lobe epilepsy
Epileptologists call the first signs of sudden attacks an aura, which is essentially a harbinger of a subsequent short-term focal paroxysm (from the Greek - excitement, irritation). However, not all patients have auras, many simply do not remember them, and in some cases the first signs are all that is needed (which is considered a minor partial seizure).
Among the first signs of an approaching attack is the appearance of an unfounded feeling of fear and anxiety, which is explained by a sharp increase in the electrical activity of the hippocampus and amygdala (part of the limbic system of the brain that controls emotions).
Attacks of temporal lobe epilepsy are most often classified as simple partial, that is, not accompanied by loss of consciousness, and usually manifest themselves no longer than two to three minutes with only abnormal sensations:
- mnestic (for example, the feeling that what is happening has already happened before, as well as a short-term “loss” of memory);
- sensory hallucinations – auditory, visual, olfactory and gustatory;
- visual distortions of the size of objects, distances, parts of one’s body (macro and micropsia);
- unilateral paresthesia (tingling and numbness);
- weakening of the reaction to others - a frozen, absent gaze, loss of a sense of reality and a short-term dissociative disorder.
Motor (movement) paroxysms or automatisms may include: unilateral rhythmic contractions of the muscles of the face or body; repetitive swallowing or chewing movements, smacking, licking of the lips; imperative turns of the head or aversion of the eyes; small stereotypical movements of the hands.
Vegetative-visceral symptoms of temporal epilepsy are manifested by nausea, excessive sweating, rapid breathing and heartbeat, as well as discomfort in the stomach and abdominal cavity.
Patients with this type of disease may also have complex partial seizures – if the electrical activity of neurons in other cerebral areas increases sharply. Then, against the background of complete disorientation, movement coordination disorder and transient aphasia (loss of the ability to speak or understand the speech of others) are added to all the symptoms already listed. In extreme cases, what begins as an attack of temporal epilepsy leads to the development of a generalized tonic-clonic seizure – with convulsions and loss of consciousness.
After the seizure has stopped, in the postictal period, patients are inhibited, feel briefly confused, do not realize and most often cannot remember what happened to them.
Read also – Symptoms of damage to the temporal lobes
Forms
Among the problems of modern epileptology, which includes over four dozen types of this disease, their terminological designation does not lose its relevance.
The definition of temporal lobe epilepsy was included in the International Classification of Epilepsies ILAE (International League Against Epilepsy) in 1989 – in the group of symptomatic epilepsy.
Some sources divide temporal epilepsy into posterior temporal lateral and hippocampal-amygdaloid (or neocortical). Others classify such types as amygdaloid, opercular, hippocampal, and lateral posterior temporal.
According to domestic specialists, secondary or symptomatic temporal epilepsy can be diagnosed when its cause is precisely established. In order to unify terminology, ILAE experts (in the classification revised in 2010) proposed removing the term “symptomatic” and leaving the definition – focal temporal epilepsy, that is, focal – in the sense that it is precisely known which area is damaged causing the disturbances in the functioning of the brain.
The latest version of the international classification (2017) recognizes two main types of temporal lobe epilepsy:
- mesial temporal epilepsy with local attachment of foci of epileptic activity to the hippocampus, its dentate gyrus and amygdala (that is, to areas located in the middle part of the temporal lobe); previously it was called focal symptomatic epilepsy.
- Lateral temporal lobe epilepsy (a rarer type that occurs in the neocortex on the side of the temporal lobe). Lateral temporal lobe epilepsy attacks involve auditory or visual hallucinations.
Cryptogenic temporal epilepsy (from the Greek - "hiding place") implies seizures of unknown or unidentified origin during examination. Although doctors use the term "idiopathic" in such cases, and most often such diseases have a genetically determined etiology, the identification of which causes difficulties.
The classification does not include partial temporal epilepsy, that is, limited (partial) or focal, but uses the term focal temporal epilepsy. And partial are only focal seizures or attacks of temporal epilepsy, reflecting aberrations of the electrical activity of the brain.
In case of simultaneous disturbances in other brain structures adjacent to the temporal lobes, it can be defined as temporoparietal epilepsy or frontotemporal epilepsy (frontal-temporal), although in domestic clinical practice such a combination is most often called multifocal epilepsy.
Complications and consequences
Periodically recurring manifestations of functional disorders of the temporal lobe of the brain have certain consequences and complications.
People with this type of epilepsy experience emotional instability and are prone to depression. Over time, repeated attacks can lead to deeper damage to the pyramidal neurons of the hippocampus and dentate gyrus, which leads to problems with learning and memory. When these lesions are localized in the left lobe, general memory suffers (forgetfulness and slow thinking appear), while in the right lobe, only visual memory suffers.
Diagnostics temporal lobe epilepsy
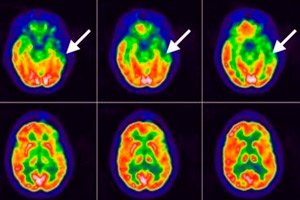
Examination of patients does little to help diagnose this disease; the doctor can only listen to their complaints and description of sensations, and then be sure to send them for an examination, during which instrumental diagnostics are carried out using:
- electroencephalography (EEG), which determines the electrical activity of the brain;
- MRI of the brain;
- PET of the brain (positron emission tomography);
- polysomnography.
Differential diagnosis
Differential diagnosis involves distinguishing between conditions with similar symptoms, including panic attacks, psychotic disorders, crisis manifestations of vegetative-vascular dystonia, transient ischemic attack (microstroke), multiple sclerosis, tardive dyskinesia, occipital epilepsy.
More details in the material - Epilepsy - Diagnostics
Who to contact?
Treatment temporal lobe epilepsy
It is common to treat temporal lobe epilepsy with anticonvulsants, although many of these are now called antiepileptics because not all seizures involve convulsions.
Almost all antiepileptic drugs act by reducing the excitability of neurons through their effects on sodium and calcium presynaptic channels or by enhancing the inhibitory effects of neurotransmitters, primarily GABA.
The most commonly used older generation drugs are: Phenytoin, Carbamazepine, valproic acid preparations (Apileksin, Convulex, Valprocom), Phenobarbital. More information – Tablets for epilepsy
Nowadays, people often turn to newer antiepileptic drugs, which include:
- Lamotrigine (other trade names – Latrigine, Lamitril, Convulsan, Seizar) is a derivative of dichlorophenyl, can be used in children over two years of age; contraindicated in liver failure and pregnancy. Possible side effects include: skin reactions (up to skin necrosis), severe headaches, diplopia, nausea, intestinal disorders, decreased platelets in the blood, sleep disorders and increased irritability.
- Gabapentin (synonyms: Gabalept, Gabantin, Gabagama, Neuralgin, Tebantin) is an analogue of gamma-aminobutyric acid.
- Lacosamide (Vimpat) is used after 16 years of age in doses determined by the doctor. The list of side effects of this drug includes: dizziness and headache; nausea and vomiting; tremors and muscle spasms; sleep, memory and movement coordination disorders; depressive state and mental disorders.
For partial seizures in adults and children over six years of age, Zonisamide (Zonegran) is prescribed, among the common side effects of which are: dizziness and skin rashes; decreased appetite and memory; impaired vision, speech, coordination of movements and sleep; depression and the formation of kidney stones.
Antiepileptic drug Levetiracetam and its generics Levetinol, Comviron, Zenicetam and Keppra are prescribed for temporal epilepsy to patients over 16 years of age with tonic-clonic seizures. They contain pyrrolidine-acetamide (gamma-aminobutyric acid lactam), which acts on GABA receptors. Since Keppra is available as a solution, it is administered by infusion in an individually determined dosage. Its synonym Levetiracetam is tablets for oral administration (250-500 mg twice a day). The use of this drug, like many of the above, can be accompanied by general weakness, dizziness, and increased drowsiness.
In addition, it is necessary to take magnesium supplements and vitamins such as B-6 (pyridoxine), vitamin E (tocopherol), vitamin H (biotin) and vitamin D (calciferol).
Physiotherapy treatment (deep brain and vagus nerve stimulation) is also used – read the article Epilepsy – Treatment
If temporal lobe epilepsy in children causes seizures, a low-carbohydrate, high-fat ketogenic diet is recommended. When prescribing this diet, a child or adolescent must be provided with adequate nutrition and monitored for growth and weight.
Surgical treatment
According to statistics, up to 30% of patients with mesial temporal lobe epilepsy cannot control their seizures with medication.
For some patients, surgical treatment may be considered – selective amygdalohippocampectomy, that is, removal of the amygdala, anterior hippocampus and part of the dentate gyrus.
Such a radical measure is justified only in the presence of hippocampal sclerosis, but there is no guarantee of the effectiveness of this operation. Surgical intervention by lobectomy, stereotactic radiosurgery or laser ablation can lead to a significant decrease in cognitive function of the brain.
Folk remedies
There is no scientific evidence that herbal treatment helps with any type of epilepsy. However, herbalists recommend drinking decoctions and infusions of ragwort (Senecio vulgaris), common peltwort (Hydrocotyle vulgaris) of the Araliaceae family, sedative tinctures of the roots of Baikal skullcap (Scutellaria baicalensis) or medicinal peony (Paeonia officinalis). But the most valuable plant for the treatment of temporal epilepsy - reducing the frequency of focal paroxysms - is considered to be mistletoe (Viscum album), which contains gamma-aminobutyric acid.
In addition, folk treatment of this pathology consists of consuming fish oil, which contains omega-3 fatty acid (docosahexaenoic acid), which helps improve cerebral circulation, and, therefore, the nutrition of brain cells.
Forecast
Pathologies such as mesial temporal sclerosis, cortical dysplasia or tumor predict the prognosis for intractability of temporal lobe-related epileptic seizures and even possible dementia.
Clinical data show that after long-term treatment, complete remission in temporal epilepsy occurs in slightly more than 10% of cases, and in almost 30% of cases, there is an unstable improvement in symptoms with the occurrence of attacks caused by stressful situations. However, temporal epilepsy in children - with its manifestation at the age of 9-10 years - by about 20 years gives a long-term remission in three cases out of ten.


 [
[