
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Endometrial polyp: causes, symptoms, prevention, prognosis
Medical expert of the article
Last reviewed: 05.07.2025
One of the variants of benign neoplasm in the uterine cavity is endometrial polyp. Such tumor is detected relatively often, and can occur as a single formation or multiple polyps of different sizes.
If we are talking about multiple endometrial polyps, then such a pathology is a proliferation of the basal endometrial layer, which has the appearance of polyps.
The structure of the endometrial polyp is made up of epithelial cells, and the polyp itself is constructed from a body on a stalk-like base.
Causes endometrial polyp
Modern specialists still cannot pinpoint the exact cause of endometrial polyp. As a rule, they identify individual risk factors that can influence the development of the disease:
- Disorder or change in the functioning of the ovaries due to increased secretion of estrogens simultaneously with a deficiency of progesterone.
- Mechanical damage to the uterus – for example, during an abortion, curettage, or long-term use of an intrauterine device.
- Habitual miscarriage, complicated childbirth, after which blood clots and particles of the placental layer remain in the uterus.
- Endocrine disorders, extragenital pathologies (thyroid dysfunction, all degrees of obesity, diabetes, hypertension).
- Psycho-emotional imbalance (long-term depression, deep stress conditions).
- Critical decline in immunity.
- Chronic problems with the reproductive system, frequent or long-term inflammatory diseases.
An endometrial polyp after childbirth develops on the mucous uterine tissues with incomplete removal of the placenta. Elements of the placental layer are firmly held on the uterine endometrium, blood clots "cling" to them, which gives rise to the formation of an endometrial polyp. Over time, such a polyp grows and increases in volume.
An endometrial polyp after IVF can develop against the background of strong hormonal transformations - for example, after several courses of hormone stimulation. If this happens, further IVF attempts are postponed, and the polyp is removed.
Psychosomatics plays a significant role in the development of endometrial polyps. It has long been known that a woman's health is directly related to her psychological and emotional balance. Even without focusing on individual points, experts are sure that most gynecological diseases in women are provoked by internal problems - women are often subject to stress, fall into depression, and experience dissatisfaction with certain circumstances. Many psychologists believe that the development of tumors, fibroids, polyps, and erosions in women is associated with the accumulation of negative energy, pain, troubles, and fears in the body. Therefore, in order to prevent the appearance of endometrial polyps, doctors advise, in addition to the usual preventive measures, to pay attention to other practices: you need to start perceiving yourself with dignity, love yourself as a person and as a woman, and achieve harmony in life. Sometimes a woman is able to cope with such tasks on her own, and in some cases she has to turn to specialists.
Pathogenesis
Pathogenetic features of endometrial polyps have been studied only partially.
Just a few years ago, doctors associated the formation of polyps with disorders of the hormonal performance of the appendages - a special role was given to excess estrogens against the background of progesterone deficiency. But today, this condition belongs to a number of hypotheses, since it has no official evidence. Against this hypothesis is the fact that the formation of endometrial polyps is often diagnosed in patients with an adequate ovulatory menstrual cycle, as well as in women with hyperandrogenism (for example, with polycostal ovarian syndrome). The appearance of polyps in patients with endometrial atrophy is also not excluded.
Today, the overwhelming majority of specialists give preference to the theory of the inflammatory origin of the disease. If we believe this theory, then a prolonged inflammatory reaction in the endometrial tissue causes degenerative and proliferative processes with a violation of the reparative function and differentiation of cells, with the formation of hyperplastic zones.
Experts believe that this theory can be supplemented with information about the painful change in the vascular network in the basal layer. The vessels thicken and become sclerotic, up to hyalinization. Tissue metabolism is disrupted, and the receptor perception of the endometrium changes.
An endometrial polyp occurs as a result of proliferative changes in the glandular apparatus of the basal layer of the endometrium. The vascular pedicle of an endometrial polyp consists of fibrous tissue and smooth muscle tissue. The term "stromal tissue" is often used for this structure.
An endometrial polyp without a stalk may occur in the early stages of the disease. As such a polyp grows, it acquires a stalk, through which the formation is nourished, because it is in it that the vessels pass. Only in some cases does the polyp continue to grow on a wide base - this type of growth is considered the most unfavorable. Such a polyp should be removed as soon as possible.
The development of endometrial polyps is associated with the proliferation of tissues of the same name. The most common localization of the disease process is the cervix or uterine cavity (upper or middle segment). A polyp in the bottom of the endometrium is found the least often, but this type of disease development is also possible.
 [ 11 ]
[ 11 ]
Symptoms endometrial polyp
An endometrial polyp does not always manifest itself with any clinical signs. Small polyps develop especially covertly. In most patients, they are diagnosed by chance during a routine ultrasound.
The first signs appear if the endometrial polyp reaches a more pronounced size:
- the monthly cycle is disrupted, spotting or heavy intermenstrual discharge appears;
- in postmenopausal patients, occasional bloody vaginal discharge occurs;
- spastic pains are observed in the lower abdomen (especially severe pain occurs during sexual intercourse);
- additional pathological discharge appears;
- bleeding may occur after sexual intercourse;
- problems with conceiving a child arise.
Endometrial polyp and temperature, contrary to the opinion of many, do not have a close relationship. However, temperature is a sure sign of the presence of an inflammatory reaction in the body, which, in turn, can become an indirect cause of the development of endometrial polyp.
Menstruation with endometrial polyp is almost always disrupted. Even with an asymptomatic course of the disease, various pathological discharges with endometrial polyp occur - from slight "smearing" to dysfunctional uterine bleeding of a cyclic or acyclic type. Menorrhagia is often observed with polyp - heavy menstrual discharge, bloody fluid before menstruation, "smearing" between menstrual bleeding. In many women, spotting with endometrial polyp is detected after sexual intercourse. Such regular blood loss can cause anemia, which is accompanied by pale skin, dizziness, and a state of general weakness.
Delayed menstruation with endometrial polyp is observed against the background of the appearance of extraneous mucous discharge - on any day of the menstrual cycle. The discharge becomes more intense after sexual intercourse, and may contain impurities or streaks of blood.
Pain associated with endometrial polyps can vary from a state of slight discomfort in the lower abdomen to severe spasmodic pain, both at rest and after physical exertion or sexual intercourse.
Diagnostics endometrial polyp
Endometrial polyp must be differentiated from other gynecological diseases. Therefore, it is very important to conduct an accurate and complete diagnosis of the pathology.
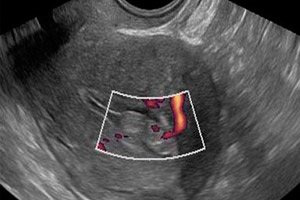
Today, specialists have various diagnostic methods that allow them to detect endometrial polyps. The primary diagnostic procedure is an ultrasound examination, which detects a polyp as a homogeneous tumor with smooth edges. Additionally, the doctor may prescribe a histological examination of endometrial particles, as well as hysteroscopy.
Treatment endometrial polyp
Any treatment plan for endometrial polyps involves the removal of this formation. Removal is carried out in different ways, suitable for each specific case. After removal, the patient undergoes restorative treatment. First of all, it is necessary to restore the impaired menstrual function, correct the hormonal balance, eliminate endocrine problems, etc. Treatment is selected individually, taking into account the patient's age, the presence of reproductive function, the size of the polyps, etc.
Read also:
Prevention
Of course, it is easier to prevent any disease than to look for a way to eliminate the problem later. It makes sense to pay attention to the prevention of endometrial polyps. For this purpose, you should listen to the following advice:
- A visit to the gynecologist should be mandatory and regular for any woman.
- It is important to monitor your weight and prevent the development of obesity.
- It is necessary to use reliable methods of contraception and avoid abortions.
- Any gynecological disease must be treated immediately after its detection, strictly following the doctor's recommendations.
If any woman pays close attention to her health and regularly consults with her gynecologist, this will help to avoid a lot of troubles and diseases, including preventing the development of endometrial polyps.
How to avoid recurrence of endometrial polyp?
If a woman has a predisposition - for example, hereditary - to the formation of endometrial polyps, then preventive measures should be taken even after the removal of the problematic formation. Such prevention will include the following points:
- it is essential to undergo a course of preventive hormonal therapy;
- Additionally, you should strengthen your body's own defenses by taking multivitamin preparations;
- If necessary, the doctor will prescribe specific antimicrobial prophylaxis.
Patients who are prone to endometrial polyps should visit a gynecologist not just regularly, but even more often than other women. This will help, if not to avoid the disease, then to detect it as early as possible.
Forecast
The prognosis can be considered favorable in cases where the endometrial polyp was detected and removed in time. However, it should be taken into account that approximately 6% of patients may develop a polyp again, so it is very important to be regularly monitored by a gynecologist. When diagnosing complications, the prognosis will depend on the severity of the problem and its stage.
What complications can we talk about?
- Reproductive dysfunction, menstrual cycle disorders.
- Pain during sexual intercourse.
- Anemia due to heavy or chronic blood loss.
- Malignancy (cancerous transformation of a tumor).
- Necrosis of the polyp due to twisting of the stalk or disruption of trophic processes.
In any case, the quality of the prognosis depends on the timeliness of seeking medical help.
Sick leave after endometrial polyp removal
Since the patient may experience some discomfort for several days after the endometrial polyp removal, such as pain or discharge, she is given a sick leave for approximately 4 days. During this time, the woman should not go to work or do physical exercises. It is forbidden to take a bath, have sex, lift heavy objects, or bend over sharply. If the patient's temperature rises during the recovery period, severe pain or bleeding occurs, she should immediately consult a doctor. In the event of complications, the doctor will prescribe appropriate therapy and extend the sick leave. An endometrial polyp is a serious disease, which requires all efforts and efforts to eliminate, and only in this case will the disease recede forever.

