
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Esophageal leukoplakia
Medical expert of the article
Last reviewed: 04.07.2025
If the epithelial layer of the mucous tissue of the upper digestive tract begins to intensively keratinize, then we speak of the development of leukoplakia of the esophagus. At the initial stage of the disease, a dense plaque is formed, which can be removed and is practically not accompanied by signs of the inflammatory process. Over time, destructive changes in the mucous membrane appear on the cheeks, tongue, and in the oral cavity. In the absence of treatment, there is a high risk of developing a malignant process. [ 1 ]
Epidemiology
If we consider the general statistics of patients seeking help for esophageal leukoplakia, the disease is most often found among patients aged 30 to 70 years, and more often among males (more than 4% in men compared to 2% in women).
For every hundred cases of patients diagnosed with leukoplakia, there may be up to 6% of precancerous pathologies and up to 5% of early stages of cancer. We are talking mainly about patients with warty and erosive-ulcerative types of esophageal leukoplakia: in such patients, the precancerous condition can be reclassified as an invasive squamous cell carcinoma process.
Initial or growing carcinoma of the mucous tissues of the esophagus due to intensive keratinization is sometimes similar to leukoplakia. Given this, any person with a suspicion of this disease is referred for histological and other studies for timely diagnosis of a precancerous or malignant condition.
It is worth noting that leukoplakia of the esophagus is an extremely rare pathology when compared with leukoplakia of the oral cavity. It can be said that these two diseases are often identified due to the commonality of clinical manifestations. In some countries, for a more accurate formulation of the diagnosis, the term "leukoplakia of the esophagus" is replaced by the term "epidermoid metaplasia of the esophagus".
Causes esophageal leukoplakia
Experts have not yet determined the exact etiology of the development of leukoplakia of the esophagus. However, it is already possible to say with confidence that the pathology arises under the influence of predominantly external damaging factors - in particular, thermal, mechanical or chemical irritation. The risks of the disease are significantly increased by the simultaneous influence of several such factors. For example, leukoplakia of the esophagus and oral cavity is often found in "malicious" smokers: their mucous membrane is regularly exposed to both thermal and chemical effects of nicotine resins and cigarette smoke. [ 2 ]
If we look at it in more detail, the following reasons can lead to the development of leukoplakia of the esophagus:
- neurodystrophic disorders affecting mucous tissues;
- chronic inflammatory processes of the skin and mucous membranes, digestive system;
- genetic predisposition (so-called “familial” dyskeratosis);
- hypovitaminosis of vitamin A;
- involution of mucous tissues;
- hormonal disorders, prolonged or severe hormonal imbalance;
- infectious lesions of the oral cavity and digestive tract;
- harmful occupational influences, including chronic occupational diseases;
- smoking, alcohol abuse;
- eating excessively hot food, overusing hot seasonings and spices;
- systematic consumption of dry food, regular consumption of coarse, dry food;
- dental diseases, presence of dental implants;
- dental problems or missing teeth, which prevents you from chewing food properly;
- pathologically weakened immunity.
Risk factors
People over 30 years of age can be considered at risk for esophageal leukoplakia. In childhood, the pathology occurs much less frequently.
Experts identify a number of factors that can contribute to the occurrence of this disorder:
- viral diseases, carriage of viral infections (in particular, herpes virus, etc.);
- infectious and inflammatory pathologies, especially those with a long or chronic course;
- regular mechanical, chemical or thermal injuries (frequent repeated gastroduodenoscopy procedures, consumption of too coarse dry food or hot food, drinking aggressive liquids – for example, strong alcohol, etc.);
- systematic smoking;
- regular induction of vomiting (for example, in eating disorders);
- professional harmful effects and pathologies (inhalation of chemical vapors, dust, work with acids and alkalis);
- impaired absorption of vitamins, insufficient intake of vitamins into the body;
- a sharp or severe weakening of the immune system (in particular, in patients with HIV and other immunodeficiency conditions);
- hereditary factor (the presence of a similar pathology in close relatives).
In addition to the immediate causes of esophageal leukoplakia, doctors highlight the special significance of risk factors that are associated with genetic predisposition, individual characteristics and the patient's lifestyle. Timely correction or elimination of these factors can become an effective step in preventing this pathology: systematic consultation with a therapist or gastroenterologist helps patients not only learn more about their health, but also detect the pathology as early as possible. If necessary, the doctor will immediately prescribe appropriate diagnostic procedures and conduct targeted treatment. [ 3 ]
Pathogenesis
The formation of pathological foci of leukoplakia of the esophagus is influenced by various etiological factors that have a negative impact on the mucous tissues and the body as a whole. However, the pathogenetic mechanism of the disease has not been thoroughly studied: the involvement of interferons and other immune mediators in the pathogenesis does not prove the specificity of the development of leukoplakia.
Presumably, under the influence of certain irritants, the expression of the adhesion protein specific to epithelial tissue is disrupted. This leads to increased intercellular interaction of epithelial cells, which activates the processes of cellular hyperdifferentiation.
It follows that excessive keratinization occurs, physiologically abnormal, and at the same time cellular “maturity” increases with suppression of apoptosis. As a result of these processes, the keratinized “long-lived” cells “bonded” to each other do not exfoliate, and dense hyperkeratotic layers are formed. [ 4 ]
Over time, as a result of various external influences, destructive changes occur in the tissues, which leads to increased cellular proliferation in the basal layer. It is noteworthy that all the above processes occur without activation of immune reactivity, which is typical for leukoplakia. Given this, the treatment of the pathology should be based on the normalization of intercellular interactions.
Symptoms esophageal leukoplakia
For many patients, leukoplakia of the esophagus is accompanied by a significant decrease in the quality of life, and the risk of malignancy of the disease negatively affects the general psychological status of patients.
The main types of esophageal leukoplakia are:
- flat, or simple leukoplakia of the esophagus;
- warty type of disease;
- erosive-ulcerative type;
- soft leukoplakia.
Simple leukoplakia is the most common. During an external examination, it is usually not possible to detect any pathological abnormalities. There is no enlargement of nearby lymph nodes by palpation. During the examination of the pharynx, the doctor pays attention to the mucous membrane, which should normally be sufficiently moist, shiny, and pale pink. When leukoplakia of the esophagus spreads to the pharynx and oral cavity, limited light spots are formed that have clear configurations, without bulges (a type of whitish film that cannot be separated). Often, keratosis zones spread further - to the inner surface of the cheeks, lips. Important: the whitish spot cannot be removed, even by force.
Verrucous type of esophageal leukoplakia may develop from a simple (flat) type of pathology. Patients complain of a burning sensation behind the breastbone, constant irritation or dryness in the throat, discomfort when swallowing food (especially when eating dry). No pain or other symptoms are detected. During the survey of patients, the presence of bad habits (smoking, alcohol abuse), concomitant diseases of the digestive, endocrine or cardiovascular systems are revealed.
Verrucous type of leukoplakia can occur in two variants:
- plaque leukoplakia of the esophagus (accompanied by the formation of white plaque-like lesions);
- verrucous leukoplakia of the esophagus (dense growths form like warts).
It is possible to notice such changes in the mucous membrane only when performing an endoscopy, or when the process spreads to the back of the tongue and its lateral surfaces, to the oral cavity, alveolar process, and palate.
In the plaque variant, the pathological foci are limited, protrude slightly above the surface of the mucosa, and are characterized by an irregular configuration and clear contours.
In the warty variant, a tubercle appears above the mucous membrane, dense, it is impossible to form a fold on it. The color of the elevation varies from whitish to deep yellow.
The erosive type of esophageal leukoplakia is characterized by the formation of erosive defects and cracks, which is a consequence of the lack of treatment of simple or warty variants of the pathology. Due to obvious tissue damage, the patient experiences pain, a burning sensation, compaction, and pressure. Pain occurs after exposure to absolutely any irritant - in particular, during eating and drinking. Bleeding of wounds is possible.
The first signs of esophageal leukoplakia are not the same in all people. Quite often, the problem appears without obvious symptoms, as it can exist unnoticed for many years.
In other cases, leukoplakia makes itself known through certain sensations of discomfort – for example, difficulty swallowing, a sore throat and burning sensation behind the breastbone, etc. However, these signs usually appear at a relatively late stage of the disease. [ 5 ]
Stages
The stages of leukoplakia of the esophagus and oral cavity are determined by the type of disease:
- At the first stage, light films appear on the mucous membrane, which cannot be removed with a swab. Other pathological signs are usually absent. Treatment at this stage is most effective, since only the submucous layer of the esophagus is affected.
- The second stage is characterized by the appearance of raised tubercles, which can spread and merge. At the same time, the nearest lymph nodes can be affected.
- At the third stage, microdamages in the form of cracks or erosions are formed in the area of the tubercles. Additional painful symptoms appear, such as pain, burning, provoked by food and drink particles getting into the wounds. Against the background of constant discomfort, the patient's psychoneurological state is disturbed, irritability and insomnia occur. Significant narrowing of the esophagus lumen is possible.
The clinical picture at one or another stage of leukoplakia of the esophagus can manifest itself both comprehensively and singly, since it depends on many factors: the presence of other pathologies, the individual characteristics of the patient, the prevalence of the disease process, etc. Therefore, if discomfort occurs during or after eating, a professional consultation with a doctor of the appropriate profile is necessary - in particular, a gastroenterologist or dentist.
Forms
The modern classification presented by the World Health Organization divides leukoplakia into homogeneous and non-homogeneous forms. The non-homogeneous form is also subdivided into erythroplakia, nodular, spotted and warty types.
There is information that some cases of non-homogeneous leukoplakia in every second case are epithelial dysplasia and have a high risk of malignancy.
There is another classification that includes such a concept as "epithelial precancerous condition": it includes erythroplakia and leukoplakia. According to this histological division, leukoplakia is divided into focal epithelial hyperplasia without signs of cell atypicality, as well as low, moderate and severe dysplasia. Dysplasia, in turn, is characterized as squamous intraepithelial dysplasia (has three degrees of severity).
The specified classification is used for pathomorphological description and supplementation of clinical diagnosis.
Complications and consequences
In the absence of necessary treatment, or with improper therapy of leukoplakia, the pathological process grows, tissue compaction occurs, which can subsequently provoke narrowing of the esophagus (persistent stenosis of the lumen). Typical signs of deterioration of the condition are:
- the appearance of hoarseness, wheezing;
- persistent coughing for no apparent reason;
- constant sensation of a foreign body in the throat;
- pain, especially when trying to swallow food.
The patient begins to experience difficulties with eating, loses weight, becomes irritable, sleep is disturbed, and work capacity decreases.
However, the most complex and dangerous consequence of leukoplakia of the esophagus may be a tumor process of malignant etiology. Most often, the complication develops against the background of warty and erosive-ulcerative types of the disease. Two forms of esophageal cancer are determined:
- squamous cell carcinoma, which develops from the epithelial cells lining the esophagus;
- adenocarcinoma that occurs in the lower segment of the esophagus.
Other types of malignant processes in the esophagus are relatively rare.
But at an early stage of development, leukoplakia responds well to therapy, which is carried out simultaneously with the elimination of possible irritating factors, including bad habits.
Diagnostics esophageal leukoplakia
General diagnostics of esophageal diseases usually includes:
- collection of anamnesis;
- visual examination (inspection);
- esophagoscopy;
- electrocardiography (for differential diagnosis of chest pain);
- X-ray examination of the esophagus;
- esophagomanometry.
The tests include general blood and urine tests. If malignant degeneration is suspected, a blood test for tumor markers may be performed – substances that are formed by tumor cells and secreted into biological fluids. Tumor markers are most often found in the blood of patients suffering from oncological pathologies. [ 6 ]
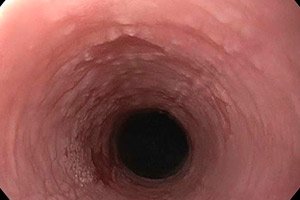
Instrumental diagnostics are always effective when used in combination with other diagnostic methods. The main procedure is considered to be an endoscopic examination of the esophagus: a soft endoscope is inserted into its cavity, with the help of which a complete examination of the entire mucous tissue is performed, and even, if necessary, a biopsy is taken - a piece of tissue for histological analysis.
The endoscopic picture depends on the type of esophageal leukoplakia:
- In the flat form, acanthosis with proliferative changes in the basal and spinous layers, as well as dysplasia with parakeratosis dominance are observed in the epithelial cells. Externally, this is manifested by the formation of limited whitish spots that look like glued films.
- In the warty form, unlike the flat form, hyperkeratosis dominates. A typical cellular enlargement of the spinous and basal layers is observed, against the background of slight atypia and polymorphism. In the underlying structures, the capillary network expands, there are signs of focal lymphoid infiltration with the presence of few eosinophils and plasma cells. Elevations of various shapes and sizes, compacted, light-colored (in the form of plaques or warty growths) are found on the mucosa.
- In the erosive-ulcerative form, all signs of a chronic inflammatory process with the formation of a histiocytic-lymphoid infiltrate are detected. Intensive hyperkeratosis develops in the layer of defective epithelium, dysplasia of the basal layer occurs, and ulcerated foci appear. The underlying tissue is subject to cellular infiltration. Endoscopic examination reveals erosions and/or cracks, sometimes bleeding. Erosive foci can have diameters from one millimeter to two centimeters. [ 7 ], [ 8 ]
Hyperplastic, parakeratotic, hyperkeratotic changes, increased number of mitoses, basal polarity failure, nuclear polymorphism, cellular keratinization, hyperchromatism and other signs are considered by specialists as a precancerous condition. An incorrect ratio of the triad, including proliferative activity, cellular differentiation and biochemical anaplasia processes, is noted. [ 9 ]
Differential diagnosis
The flat type of leukoplakia requires differentiation from the typical course of lichen planus, in which a characteristic morphological structure is found, a symmetrical unification of polygonal papules. The predominant localization of pathological elements in lichen planus is the retromolar zone and the red labial border.
The typical type of leukoplakia is differentiated from limited hyperkeratosis, in which a flat area is formed, lined with dense scales and surrounded by a thin light elevation.
Verrucous type of leukoplakia is distinguished from candidal infection. This disease is characterized by the appearance of whitish-grayish films, tightly "sitting" on the mucous tissue. When trying to forcibly remove the film, a brightly bleeding ulcer surface is revealed. For additional diagnostics, cytological analysis is performed.
The erosive-ulcerative type of leukoplakia requires differentiation from a similar type of lichen planus, in which small nodules appear along the edges of pathological lesions (they may also be present on the skin).
In addition, the disease should be distinguished from manifestations of secondary syphilis, chronic mechanical damage to the mucous membrane and reflux esophagitis, chemical and thermal burns of the esophagus. To identify these pathologies, it is important to consider the configuration of the lesions, their elevation above the surface of the mucous membrane, the presence of shine, separation of particles when scraping, and the presence of background changes.
It is not always possible to base a diagnosis on an external examination and collection of the patient's anamnesis. One should not forget about such a variant of pathology as idiopathic leukoplakia of the esophagus, which develops without any apparent reason. In this case, differential diagnostics are especially important.
Not all specialists note the need to separate such concepts as leukoplakia of the esophagus and oral cavity: in many ways, these terms are copied. And in the histological decoding, such a reporting sign as "leukoplakia of the esophagus" may be completely absent: it is much more important for the attending physician to know the nature of the histological processes - that is, as a result of which the foci of compaction were formed - as a result of atrophy, edema, infiltration, acanthosis of the middle epithelial region, hyperkeratosis of the superficial areas of squamous epithelial tissue of the esophagus. Information on the presence of atypical cells, dysplasia is also necessary. For this, it is necessary to apply an expanded approach to examining patients.
Who to contact?
Treatment esophageal leukoplakia
Esophageal leukoplakia is most effectively treated by surgical intervention using liquid nitrogen, laser or electric coagulator. Cryosurgery is considered the most optimal method, as it has a minimal risk of relapse of the pathology.
During treatment, it is necessary to use a comprehensive tactic. In addition to cauterizing pathological foci, it is necessary to undergo a course of antibiotic therapy, as well as to follow a strict diet for a sufficiently long time with the complete exclusion of alcoholic beverages, hard-to-digest, spicy, sour dishes.
In general, treatment measures for leukoplakia of the esophagus are local and general.
A prerequisite for effective local action is the neutralization of the damaging factor. For example, the patient must stop smoking and drinking alcohol. If this is not done, the disease will not only progress, but the risk of malignancy will also increase significantly. Other important points include compliance with all oral hygiene rules, additional sanitizing measures, the use of medications, and, if necessary, the help of a surgeon.
Specialists practice different methods of therapeutic impact on the affected areas in leukoplakia of the esophagus. The most common and accessible means is considered to be the applicator application of an oil solution of vitamin A to the foci of pathology, as well as the internal use of the combined drug Aevit (a combination of vitamins A and E).
Radical treatment is prescribed if leukoplakia of the esophagus has reached a critical stage, or in cases where the use of medications does not have the necessary therapeutic effect. [ 10 ]
Surgical treatment involves excision of the affected areas using a scalpel, laser beam (CO2 or helium-neon), electrocoagulator, cryodestructor. Several methods of exposure can be used. However, such treatment has its drawbacks: cicatricial changes are formed, tissues are deformed, the functional capacity of the esophagus is impaired. Tissue recovery is usually long, the average period of epithelialization is about 2 months. Serous edema develops in the operated areas, a wet scab is formed, and cellular activity, protein and carbohydrate metabolism processes are slowed down. All this directly affects the duration of the regeneration period. Another important point: even surgical intervention does not guarantee the absence of relapses and does not reduce the likelihood of developing a malignant tumor. [ 11 ]
Other radical techniques are also used, in particular, low-frequency ultrasound, photodynamic treatment based on the selective destruction of altered tissues using stimulation of photosensitive elements.
It is necessary to take into account that the possibilities of surgical treatment are limited: first of all, this refers to the peculiarities of access to the esophagus, the trauma of the intervention, etc. [ 12 ]
Drug treatment of esophageal leukoplakia
For internal use, retinol, tocopherol in the form of oil solutions, and B-group vitamins (in particular, riboflavin, 0.25 g twice a day for a month) are prescribed.
It is possible to use general tonics, biogenic stimulants, and keratoplastic agents.
Aevit |
Take for a long time, about 1.5 months, 1 capsule per day. Repeat the course of treatment - after 3 months. Possible side effects: fatigue, sleep disturbance, loss of appetite. |
Plasmol |
Administer subcutaneously 1 ml daily or every other day. One course of treatment requires 10 injections. Some patients may experience hypersensitivity reactions to the drug (itching, rash, increased body temperature). |
Longidaza |
Administered subcutaneously or intramuscularly in the amount of 3 thousand IU. The course requires from five to 25 injections. The interval between injections is 3-10 days. A repeat course is possible in 2-3 months. Possible side effects: pain in the injection area, slight redness of the skin. |
Lavomax (Tiloron) |
The first two days are taken at 125 mg once a day, and then at 125 mg every other day. The drug has an immunomodulatory and antiviral effect. Some patients may develop an allergy to the components of the drug. |
Solcoseryl |
Used for intravenous infusions with sodium chloride solution or 5% glucose. The dosage and frequency of administration are determined by the attending physician. Side effects are extremely rare, slight pain in the injection area is possible. |
The volume of therapy is determined by the attending physician, depending on the form of esophageal leukoplakia, the size of the lesions and the rate of development of the disease process. Vitamin A is taken orally in the form of a 3.4% oil solution of retinol acetate or 5.5% retinol palmitate, 10 drops three times a day for 6-8 weeks. The treatment course is repeated every 4-6 months.
Physiotherapy treatment
Physiotherapeutic methods include the elimination of esophageal leukoplakia zones using diathermocoagulation or cryodestruction. Diathermocoagulation is performed intermittently, until the hyperkeratosis zones are completely coagulated. The healing process lasts 1-1.5 weeks.
Cryodestruction is currently actively used in the complex therapy of precancerous conditions. The procedure has virtually no contraindications, it can also be prescribed to patients suffering from complex systemic pathologies. During cryodestruction, contact freezing can be used in areas that are difficult to access surgically. Temperature exposure indicators are 160-190 ° C, duration is 1-1.5 minutes. The defrosting period is about three minutes, the healing period is up to 10 days.
Photodynamic treatment of patients with esophageal leukoplakia is considered one of the most advanced methods. It involves the application of photosensitizers to pathologically altered areas. During light exposure to waves of a certain length (in accordance with the absorption limit of the dye), molecular concentration of energy occurs. When released, it affects the transition of molecular oxygen from the external environment into active unstable forms - in particular, into singlet oxygen, which is capable of destroying microbial cells. This is a relatively new physiotherapeutic technique, which is not yet available in all medical institutions.
Herbal treatment
Traditional methods of treatment for leukoplakia of the esophagus are not always appropriate and effective. Their use is allowed only after approval from the attending physician. The fact is that untimely and incorrect use of medicinal plants can worsen the course of the pathological process, aggravate existing problems with the gastrointestinal tract, and cause the development of complications.
Meanwhile, the following folk recipes are used most successfully for leukoplakia of the esophagus:
- Hemlock. [ 13 ] The inflorescences of the plant are crushed, loosely poured into a half-liter jar to the top, filled with vodka and closed with a lid. Keep in the refrigerator for three weeks. Then the tincture is filtered and taken according to the following scheme: the first day, take 2 drops of tincture in 150 ml of water, then the dose of the product is increased daily by one drop, bringing it to 40 drops per dose. After this, the amount of the product is again reduced, to the original 2 drops.
- Infusion of pine needles. Collect fresh pine needles, put them in a thermos and pour boiling water over them (130 g of needles per 500 ml of boiling water). Infuse for 8 hours (optimally leave overnight). Then filter the medicine and start taking it, drinking a couple of sips during the day in several approaches. It is advisable to prepare a fresh infusion every day.
- Carrot and beetroot juice. Prepare and drink freshly squeezed carrot and beetroot juice daily (approximately 50:50), on an empty stomach, an hour before meals, 150 ml.
Traditional medicine is best used as a supplement to traditional treatment methods. You should not rely solely on traditional recipes, especially when it comes to advanced stages of esophageal leukoplakia.
Prevention
Prevention of the development of leukoplakia of the esophagus involves quitting smoking, drinking alcohol, limiting spicy and sour foods in the diet, regularly performing hygienic procedures to clean the oral cavity, and timely treatment of any pathologies of the digestive tract. The listed set of measures is supplemented by long-term use of an oil solution of vitamin A or other vitamin preparations:
- Aevit is a complex of oil solutions of vitamins A and E;
- Asepta is a complex combination of vitamins, coral calcium, coenzyme Q10, and plant extracts.
Extracts of medicinal herbs and essential oils of natural origin have a positive effect on the condition of the oral cavity and the whole body. It is recommended to use high-quality toothpastes with an antibacterial effect, which provide protection of the mucous membrane from pathogenic bacteria and do not have a negative effect on beneficial microflora.
It is useful to regularly rinse your mouth and drink herbal teas based on chamomile, sage, calendula, and other plants with anti-inflammatory and regenerative properties.
Sea buckthorn extract and geranium essential oil are considered excellent preventive measures. These products help maintain the normal condition of the esophageal mucosa and also have fairly strong antiseptic properties.
Forecast
Treatment for esophageal leukoplakia is carried out using various methods. In mild cases, conservative therapy based on taking fat-soluble vitamins (in particular, vitamin A), as well as strengthening the body's natural defenses, can be used. The course of the pathology itself is unpredictable and individual for each patient: some patients live with the initial stage of the disease until the end of their lives, without complaining of discomfort or deterioration of their condition. And in other patients, squamous cell cancer may develop within a year.
If there is a suspicion that conservative therapy is not effective, the doctor prescribes surgical intervention with the removal of pathological foci and their thorough histological examination.
Without treatment, the risk of developing malignant pathology increases significantly. That is why leukoplakia of the esophagus is classified as a precancerous condition. Particularly dangerous in this sense is the ulcerative and warty type of leukoplakia, as well as the spread of pathology to the tongue area.

