
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Coronavirus COVID 19
Medical expert of the article
Last reviewed: 04.07.2025

At the end of 2019, the world was shocked by a little-studied viral infection – the so-called “Chinese virus”, or coronavirus COVID-19. We are talking about an acute viral pathology, which is characterized by predominant damage to the respiratory system and, to a lesser extent, the digestive tract. Coronavirus is a zoonotic infection – that is, one that can be transmitted to humans from sick animals.
The COVID-19 coronavirus is dangerous, first of all, because little is known about it, and there are no specific therapies or vaccines that can save from the infection. Therefore, it is extremely important for people to know as much as possible about the disease: this is necessary for prevention and early detection of cases of pathology. It is not for nothing that they say: forewarned is forearmed.
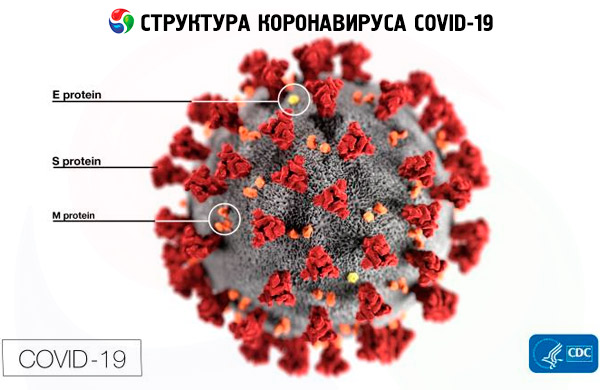
Structure of coronavirus COVID 19
Experts have managed to determine the protein structure of the COVID-19 coronavirus, which allows it to enter cells. This discovery is very important for science, because it makes it easier to work on creating a specific antiviral vaccine.
Previously, scientists discovered that the COVID-19 coronavirus is a direct "relative" of the infectious agent SARS (atypical pneumonia). However, after the experiment, it turned out that ready-made antibodies to the SARS pathogen are not able to bind the "Chinese" coronavirus. What's the matter?
Scientists have described the S-protein structure that covers the viral envelope and acts as the main tool for damaging cells. The proteins are “masked” and take the form of molecules that are essential for cells: this enables them to bind to certain envelope receptors and get inside. In particular, the S-protein of the COVID-19 coronavirus interacts with ACE2 (angiotensin-converting enzyme).
Using the microscopic method of CEM, it was possible to determine the three-dimensional organization of the protein surface of the "Chinese" coronavirus at a resolution of less than 3.5 angstroms. Specialists began to study the original S-proteins that did not penetrate the cell.
As a result, the molecule was practically no different from that of the SARS pathogen. But some differences were still present: for example, the segment that binds to the ACE2 receptor had an increased affinity for the target, which is what causes the rapid and easy infection of cells and the further spread of the pathogen. Antibodies to SARS infection are not able to attach well to the S proteins of the COVID-19 coronavirus, so the expected binding effect does not occur. Nevertheless, studies of the viral structure are ongoing.
Life cycle of coronavirus COVID 19
Coronaviruses have long been known to science. This is a fairly large viral family, capable of causing the development of various pathologies - mild variations like a cold, and the most severe (in particular, such complex coronavirus infections as the Middle East respiratory syndrome MERS-CoV, acute respiratory syndrome SARS-CoV are known). The latest of these known pathogens - coronavirus COVID-19 - is a new culture of microorganisms that has not yet been identified in humans.
The life cycle of the COVID-19 coronavirus does not require DNA, and this is its significant difference from other already studied RNA-containing infections (for example, HIV). This, in particular, explains the ineffectiveness of antiretroviral treatment used to suppress the development of HIV. The carrier of genetic data in the coronavirus is not DNA, but a single RNA chain of 20-30,000 nucleotides. This means that the virus protein is produced by the affected cell directly on RNA, which disguises itself as the carrier's matrix RNA. After penetrating the cell, the virus produces a specific enzyme substance - RNA polymerase, which creates copies of the virus genome. Then the affected cell produces the remaining proteins, and new virions begin to develop on it.
When viewed under a microscope, the virus particle has the appearance of an oval with a mass of tiny spikes formed by the S protein. This special protein acts as a kind of magnet, binding to a target on the cell surface of the affected organism.
According to the World Health Organization, the incubation period of the COVID-19 coronavirus disease is on average 2-14 days. However, Chinese doctors have already stated that there have been cases where this period was extended to 27 days. At the same time, an infected person is capable of spreading the infection from the first day of incubation.
Other interesting facts about the COVID-19 coronavirus:
- The coronavirus received its name due to the specific configuration of the protein compound, which resembles a crown.
- The COVID-19 coronavirus is recognized as less pathogenic than the previous similar SARS virus, which “raged” in 2003 and led to the death of 10% of people who became ill (for comparison: approximately 3% of those who become ill with COVID-19 die).
- According to experts, the incidence rate should decrease with the arrival of warm weather, since the coronavirus develops and survives better in cold conditions.
- The main danger of the COVID-19 coronavirus is the high probability of lung damage. Most often, death occurs from severe pneumonia.
- There is no information yet on immunity after a coronavirus infection. At the very beginning, doctors talked about the formation of acquired immunity, but then several cases of relapse were registered in people who had recovered from the COVID-19 coronavirus. Therefore, the issue of immunity remains open today.
The information provided by the Ministry of Health states that this type of coronavirus is transmitted by airborne droplets, from one infected organism to another.
People are considered most contagious when they show symptoms. It is possible to spread the virus before people show symptoms.
How easily does the virus spread? Spread by contact with contaminated surfaces or objects. It is possible that a person can become infected with COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth or nose.
The feco-oral type of transmission is also possible: for example, in Hong Kong, people became infected through the sewage system and unwashed hands.
There is no evidence to suggest that any animal, including pets, can be the source of infection for this new coronavirus. To date, the CDC has not received any reports of pets or other animals becoming ill with COVID-19. There is currently no evidence that pets can spread COVID-19. However, because animals can spread other diseases to people, it is always a good idea to wash your hands.
Coronavirus spreads faster. The common flu has a reproductive number of about 1.3, meaning that each person infected can infect an average of 1.3 people. This number is used to measure the potential of an epidemic. When it is greater than one, the disease tends to spread. In 2009, during the H1N1 flu pandemic, the virus had a reproductive number of 1.5. Available research suggests that the reproductive number of the coronavirus is between 2 and 3.
Like the flu virus, coronaviruses are enveloped viruses, making them sensitive to environmental conditions such as high temperatures, desiccation, and sunlight. The virus survives in a droplet for 28 days if the temperature is below 10 degrees, and only one day when the temperature exceeds 30 degrees.
Symptoms
According to data from the European Centre for Disease Prevention and Control, the COVID-19 coronavirus is characterized by the following basic symptoms:
- increase in temperature;
- cough of varying intensity;
- difficulty breathing, shortness of breath;
- muscle pain;
- a strong feeling of fatigue.
Nausea and diarrhea are other possible signs of coronavirus: they are reported in 10% of cases, and can even precede other symptoms. In early reports from Wuhan, 2–10% of patients with COVID-19 had gastrointestinal symptoms such as diarrhea, abdominal pain, and vomiting. [ 1 ], Abdominal pain was reported more often in patients admitted to the intensive care unit than in those who did not require ICU care, and 10% of patients had diarrhea and nausea 1–2 days before the development of fever and respiratory symptoms.
Some patients experience conjunctivitis. It can be noted that the symptoms generally have much in common with influenza infection. However, there are some differences from influenza:
- coronavirus infection begins literally suddenly - the patient becomes ill, although just a minute ago nothing foreshadowed trouble;
- the temperature rises sharply and strongly – often above 39°C;
- cough is dry, does not bring relief, debilitating;
- shortness of breath may be accompanied by chest pain, which indicates the development of viral pneumonia;
- The weakness in patients is so pronounced that people often cannot even lift an arm or leg.
When the COVID-19 coronavirus enters the body, it primarily affects the lower respiratory tract. With influenza, the upper respiratory system is affected first.
If any suspicious symptoms appear, you should immediately contact an infectious disease specialist or your family doctor.
Diagnostics
If you suspect you have been infected with the COVID-19 coronavirus, you should see a doctor. If your suspicions are justified, doctors will take biological material from the patient and send it to a laboratory equipped with special test systems to detect the virus. These systems are available in sufficient quantities in key medical institutions and laboratories: there is no shortage of them.
The action of such tests is based on the well-known PCR method – polymerase chain reaction. This technique has many advantages: it is widespread, highly sensitive, and the result can be obtained quite quickly. To determine an infectious disease, biomaterial is most often taken from the patient's nasopharynx, but mucus, sputum, urine, blood, etc. can also be used as research material. [ 2 ], [ 3 ]
Several test systems have already been developed to date. Some of them are aimed at detecting exclusively the COVID-19 coronavirus, while others can also detect the SARS pathogen - severe acute respiratory syndrome. It is important that all tests can detect pathology even at the earliest stages of development.
As for other methods of diagnosing coronavirus, they are auxiliary and can be used to assess the degree of damage to internal organs and the respiratory system. For example, X-rays are used to rule out or confirm the development of pneumonia.
Differential diagnosis
Differential diagnostics of coronavirus infection is carried out with rhinovirus infection, viral gastroenteritis, respiratory syncytial infection.
Treatment
To date, there is no specific treatment for the disease caused by the COVID-19 coronavirus. The main therapy is aimed at supporting the patient's body in accordance with his clinical condition.
Chinese doctors are testing a combination of several antiviral drugs at once. High doses of the well-known anti-flu drug Oseltamivir are used, as well as HIV drugs such as Lopinavir and Ritonavir. Many patients have successfully undergone treatment with the antiviral drug Abidol: [ 4 ] this drug is included in one of the treatment regimens for COVID-19 coronavirus, in combination with Ribavirin and Chloroquine phosphate, [ 5 ] interferon, or Ritonavir (Lopinavir). A clinical trial of Remdesivir, [6 ] Baricitinib for the treatment of COVID-19 has begun.
The use of a combination of three antiviral drugs with an immunostimulant (lopinavir-ritonavir plus the antiviral drug ribavirin and beta-interferon injections) in the early stages has been shown to be effective, alleviating symptoms and shortening the duration of viral shedding and hospital stay in patients with mild to moderate disease.
Results of a preliminary study show that remdesivir improves recovery time for coronavirus patients from 15 to 11 days.
The FDA-approved antiparasitic drug ivermectin inhibits SARS-CoV-2 (COVID-19) replication in vitro. A single treatment was able to cause a 5,000-fold reduction in virus over 48 hours in cell culture. Treatment with ivermectin resulted in a 99.8% reduction in cell-bound viral RNA (indicating unreleased and unpackaged virions). [ 7 ] Ivermectin is widely available due to its inclusion on the WHO Model List of Essential Medicines.
In addition to antiviral drugs, symptomatic therapy is mandatory. Medicines are prescribed to normalize the temperature, relieve cough, relieve swelling, etc. It is also possible to use specific immunoglobulins and corticosteroids - with increasing deterioration of the patient's condition, with prolonged lymphopenia, with reduced blood oxygen saturation.
If there is a risk of complications from coronavirus, antibiotic therapy and artificial ventilation are administered.
Read this article for the latest and most current treatment options for COVID-19 patients.
Prevention of coronavirus COVID 19
There is currently no specific prevention for COVID-19 coronavirus infection, although work on creating vaccines is underway quite actively. However, there are general methods for preventing viral diseases that also apply to coronavirus infection. So, how can you protect yourself from coronavirus infection?
It is important to regularly wash your hands and disinfect objects of systematic use (phones, remote controls, computer mice, keys, door handles, etc.).
Avoid touching your face, eyes, etc. with unwashed hands.
Every person should always have disinfectants with them – first of all, for hand disinfection. The coronavirus dies when exposed to alcohol.
It is necessary to exercise caution when visiting areas with large gatherings of people (transport, supermarkets, etc.) - it is better to touch surfaces and objects of common use with your hands as little as possible, or wear protective gloves.
You cannot take food from a common container or package, shake hands, or interact closely with people you don’t know well – at least until the epidemiological picture of the coronavirus stabilizes.
For prevention, you can wear a protective bandage (mask), although it is more indicated for people who are already sick. Disposable masks should be changed every 2-3 hours. Re-wearing them is prohibited.
At home and at work, it is necessary to systematically ventilate all rooms.
You should not take any medications “for prevention”: such actions will not protect you from coronavirus, but they can “blur” the clinical picture in case of illness, which will negatively affect the prognosis.
During the epidemic, it is not advisable to go on long trips and travel. However, if you cannot do without it, it is important to follow these rules:
- Even at the planning stage of the trip, you need to inquire about the epidemiological situation regarding coronavirus;
- It is necessary to take with you and use devices to protect the respiratory system;
- During trips, you can only drink water purchased in stores in closed containers, and eat only food that has been pre-heat-treated;
- You should wash your hands regularly, including before eating and after visiting public areas.
It is necessary to avoid markets where animals and seafood are sold, as well as various events in which animals that can be a source of infection with coronavirus participate in large numbers.
Other important preventive recommendations:
- Try to stay away from other people – at least 1 m away.
- Eat well, lead a healthy lifestyle, and walk in the fresh air more often.
- If someone in the house is sick, tell your family doctor. If possible, allocate a separate room for the sick person, limit contact with them, wear a medical bandage. Wash your hands more often with detergent, disinfect objects, ventilate the rooms.
If you suspect that you have been in contact with someone infected with COVID-19 or have recently returned from another country, call your family doctor and explain the situation. You should not go to a medical facility on your own, so as not to put others at risk. Then, strictly follow your doctor's instructions.
What are COVID-19 vaccines, their types and differences, read in this article.
Forecast
On average, the total duration of the COVID-19 coronavirus disease, including the incubation period, is just over one month. In the absence of treatment, as well as under other unfavorable circumstances, complications may develop:
- severe intoxication of the body;
- increasing acute respiratory failure;
- pulmonary edema;
- multiple organ failure.
If complications develop, the prognosis for coronavirus pathology is unfavorable - in many cases the patient dies.
According to the WHO, 2% of identified patients have died in Wuhan and about 0.7% outside Wuhan. The death rates are 15 times higher than the common flu (0.13%) and H1N1 flu (0.2%).
A study published in the medical journal The Lancet Infectious Diseases on March 30, 2020, found that the fatality rate from the coronavirus is lower than previously reported, but still more deadly than seasonal flu, at about 0.66%. This fatality rate from the coronavirus is lower than previous estimates because it takes into account potentially milder cases that often go undiagnosed, but it is still much higher than the 0.1% of people who die from the flu.
As for the forecast of the spread of the viral infection, experts voice two options. The first of them assumes the spread of coronavirus to a pandemic level. The second option talks about outbreaks of the disease in different parts of the planet with further establishment of control over the pathogen and gradual fading of the spread.
To improve the incidence forecast, timely quarantine measures should be introduced and mass gatherings of people should be limited. Most experts are confident that with the onset of warming, the COVID-19 coronavirus will lose its activity, and the percentage of cases will become significantly lower.

