
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
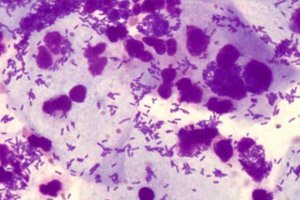
Intracellular and extracellular diplococci in the smear
Medical expert of the article
Last reviewed: 05.07.2025
Diplococci in a smear can be pathologies regardless of the localization of the process, and their identification indicates a disease or carriage, even if there are no symptoms. These bacteria can be pathogens of various pathologies - meningitis, pneumonia, gonococcal process of the genitals, and depending on this, diagnostic and treatment tactics differ.
Morphology of diplococci
Diplococci are parasites that belong to the family Lactobacteriaceae. Diplococci are characterized by a round cell structure in which two cells are joined together in pairs. These doubled cells are always together, but sometimes they may be in a small chain. Based on the degree of staining during examination, the parasites can be gram-positive and gram-negative. Gram-negative is the term used for these bacteria, which means that the purple dye is not retained (during the Gram staining process) by these organisms within the thickness of the cell. Those bacteria that retain this dye are known as gram-positive. Examples of gram-negative diplococci are Neisseria spp., Moraxella catarrhalis, and Acinetobacter spp. Examples of gram-positive diplococci are Streptococcus pneumoniae and Enterococcus spp.
These parasites threaten the development of serious infections of internal organs. Their presence in the normal flora of the body is not a normal indicator.
What causes diplococci? Since these bacteria should not be present under normal conditions, they only appear as a result of human infection. Therefore, the norm for diplococci in a smear is when they are not there at all. When they are present, the person is infected, even if there are no clinical manifestations yet.
Pathogens in the body can be at different stages in different forms - outside the cell and inside the cell. The extracellular phase does not have a pathogenic effect and cellular structure, but is harmful to humans because the cell is a parasitic pathogenic organism. This form has a very dense membrane, which helps it adapt to external conditions. It can be damaged only with the active use of disinfectants or laser radiation.
Causes diplococci in the smear
The reasons for the appearance of diplococci in a smear are contact with an infected person who is sick, or contact with a carrier of the infection, but he has no symptoms. Therefore, pathologies are considered dangerous, because they are easily spread between people. Diplococci in a smear from the nose can be cultured in many people, but they may never have pneumonia or meningitis. Such people are called carriers or potential sources of infection.
But not all people get such diseases caused by diplococci. Risk factors include decreased activity of the immune system, the use of suppressive drugs, the presence of concomitant infections or immunodeficiencies. Therefore, children and the elderly are more prone to developing diseases when in contact with diplococci.
Pathogenesis
How are diplococci transmitted? It all depends on the specific type of infectious agent. There are different types of such pathogens in the environment, but the most dangerous ones are characterized by the potential risk of developing serious, life-threatening inflammatory reactions. Being in the body, they will not cause much harm, but they can become a factor in infectious damage to the brain (or cortex), in the lungs (affect the entire respiratory system) and cause harm to the reproductive and urinary systems. Accordingly, diplococci are transmitted either by air or by contact.
Moraxella Catarrhalis is a diplococcus that is common among humans. It is non-motile in nature and causes various types of bacterial infections of the respiratory system, central nervous system, middle ear, and joints of the body. These bacteria are placed in the Moraxellaceae family, in the order Pseudomonadales. Talking specifically about diseases, bronchitis, sinusitis, otitis, and laryngitis are few conditions caused by these microbes. This microorganism is also associated with the disease of bronchopneumonia. Heavy smokers and elderly patients should be especially aware of such problems caused by Moraxella catarrhalis. Beta-lactamases produced by this organism make it resistant to penicillin. These bacteria are also resistant to tetracycline, trimethoprim sulfamethoxazole, and trimethoprim. Some strains produce a protein that confers resistance to complement by preventing the formation of the membrane attack complex. M catarrhalis also expresses specific proteins for iron uptake that act as receptors for transferrin and lactoferrin. M catarrhalis has been shown to have increased cell adhesion and proinflammatory responses to cold shock (26 C for 3 hours). Physiologically, this may occur with prolonged exposure to cold temperatures, resulting in cold symptoms.
Neisseria Meningitidis is one of the most important Gram-negative diplococci, and is responsible for causing meningitis. The mortality rates caused by its infection are high. Young children (less than 5 years) are at greater risk of infection caused by these bacteria. These microbes attack only humans, as they can obtain iron from humans (from lactoferrin and transferrin sources).
The outer membrane of this microbe contains lipooligosaccharide and in chemical form it acts as an endotoxin, which is responsible for septic shock and fever. In some cases, lipooligosaccharide also causes the destruction of red blood cells and leads to hemorrhage. The sputum of an affected person can be tested in a laboratory to confirm the presence of this bacterium.
Neisseria Gonorrhoeae is the cause of gonorrhea, a sexually transmitted infection. This bacterium moves by jerking motion with the help of locomotor organs called pili. In laboratories, the bacterium can grow on chocolate agar. In the case of gonorrhea, local manifestations of the inflammatory process can be observed, which occur when the epithelial cells of organs are damaged and leukocytes are formed. All this is accompanied by characteristic manifestations, up to the development of complications. It is not just an infection caused by this microbe, but other health problems caused by this diplococcus are troublesome. Symptoms caused by its infection include pharyngitis, conjunctivitis, urethritis, orchitis and prostatitis. Neisseria gonorrhoeae has been found to be resistant to antibiotics from the penicillin group.
Symptoms diplococci in the smear
The symptoms that diplococci cause when they infect a person depend on the disease they cause, that is, on the type of pathogen.
Moraxella catarrhalis is a gram-negative, aerobic diplococcus. The various clinical manifestations of this infection depend on the site of infection and the underlying conditions. Transmission is thought to occur through direct contact with contaminated saliva and air droplets. The preferred location of the diplococcus determines where the inflammatory process will develop. If the bacteria enter the middle ear cavity, otitis develops, and if they descend to the lungs, pneumonia develops.
The first signs of otitis media caused by this diplococcus include otoalgia (severe ear pain), fever, and hearing loss. Otitis is a very common disease, especially in children. Approximately 70% of children experience at least one episode of otitis during childhood. Symptoms develop acutely, and against the background of an increase in body temperature, ear pain increases, the child is restless, and the inflammation can be as much as a perforation of the eardrum.
A patient with sinusitis will typically present with headache, maxillary or frontal pain, fever, and cough. In young children, persistent nasal discharge (lasting more than 2 weeks) and cough, especially at night, are present.
Symptoms of lower respiratory tract infection caused by this diplococcus may include: cough, large amounts of sputum, headache, shortness of breath. As an upper respiratory tract infection, Moraxella Catarrhalis infections cause symptoms similar to common infections such as pneumonia, ear infections, and sinusitis. It should be noted that symptoms that persist for more than 10 days are most often caused by Moraxella Catarrhalis infections and require antibiotic therapy.
Diplococci in a child's sputum or ear discharge can confirm the diagnosis with an accurate determination of the causative agent. Moraxella Catarrhalis is not diagnosed individually in the usual way, but as a general bacterial infection. If the usual antibiotics do not work, the doctor will conduct some special tests to find out which antibiotic will be most effective in treating or reducing symptoms in Moraxella Catarrhalis infections. Polymorphic diplococci in a sputum smear can be determined in pneumonia, in such cases the causative agent may not be one pathogen of the Moraxella species, but also other factors, such as pneumococcus. Some diagnostic tests for Moraxella Catarrhalis may include, in addition to sputum culture, the determination of antibodies in the blood serum to the causative agent Moraxella Catarrhalis.
Cocci and diplococci in a smear of sputum or discharge from the ear may be evidence of streptococci, which require complex treatment.
Meningitis is an inflammation that occurs in the membranes of the brain and can cause swelling in the future. In addition, pathological processes can also occur in other organs when the pathogen spreads through the blood. Symptoms can be very visible and obvious, or asymptomatic in the early stages. Meningococcal disease can refer to any disease that occurs when Neisseria meningitidis enters the blood or spinal cord and brain. Meningococcal infection is an infection that spreads through close contact with an infected person. Prompt medical attention is extremely important if meningococcal disease is suspected.
When a person develops meningococcal meningitis, the bacteria infect the protective membranes that cover the brain and spinal cord, causing swelling. Symptoms of meningococcal disease can vary depending on the type of disease that develops. The first signs of pathology may be typical of any inflammation, such as fever, headache, and neck tension. Additional symptoms often occur, such as nausea, vomiting, photophobia (eyes are more sensitive to light), and altered mental status (confusion). Newborns and children may not have or may have difficulty noticing the classic symptoms of fever, headache, and neck tension. Instead, infants may be slow or inactive, irritable, and may vomit. In young children, doctors may also look at the child's reflexes for signs of meningitis.
When meningococcal septicemia develops, bacteria enter the bloodstream and multiply, damaging the walls of blood vessels. This causes bleeding into the skin and organs. Symptoms may include: fever, fatigue, vomiting, cold hands and feet, severe aches or pains in the muscles, joints, chest or abdomen. In later stages, a dark purple rash appears.
Meningococcal disease is very serious and can be fatal within hours. Early diagnosis and treatment are very important. Meningococcal disease can be difficult to diagnose because the signs and symptoms are often similar to those of other diseases. If a doctor suspects meningococcal disease, diagnosis involves examining samples of blood or cerebrospinal fluid (fluid around the spinal cord). Doctors then test the samples to see if there is an infection. Gram-negative diplococci in a smear are direct confirmation of the diagnosis. If Neisseria meningitidis bacteria are found in the samples, lab technicians can grow (culture) the bacteria. Growing the bacteria in the lab allows doctors to know the specific type of bacteria causing the infection. Knowing this helps doctors decide which antibiotic will work best.
Gonorrhea is a pathology of the reproductive system that develops due to damage by diplococcus. In women, the main symptoms of such damage include varying degrees of discharge. The most common symptom of gonorrhea is vaginal discharge due to the development of endocervicitis when the bacteria multiply in the cervix. Usually, the discharge is small in quantity, purulent, but many patients have minimal symptoms or no symptoms of gonococcal cervicitis. Other symptoms may include urinary disorders, intermenstrual bleeding, dyspareunia (painful intercourse), mild pain in the lower abdomen. If the infection progresses to pelvic inflammatory disease, symptoms may include increased vaginal discharge, fever, chills, nausea and vomiting (less common).
In men, the main symptoms of infection with this diplococcus include the development of urethritis. The main manifestation of gonococcal infection in men is a characteristic sensation of heat during urination; after a few days, copious, green discharge appears, sometimes stained with blood.
Men and women may also have classic manifestations of disseminated gonococcal infection - this is arthritis-dermatitis syndrome. Joint or tendon pain is the most common complaint in the early stage of infection. The second stage is characterized by septic arthritis. The knee is the most common site of purulent gonococcal arthritis.
Newborns who develop bilateral conjunctivitis (ophthalmia neonatorum) often develop it from a mother with a gonococcal infection. Symptoms of gonococcal conjunctivitis include the following: eye pain, redness, purulent discharge.
Extracellular gram-positive diplococci in a smear in women during a routine gynecological examination can confirm the diagnosis, since only gonococci have such a structure in such a localization. If leukocytes and diplococci are detected in the smear, this indicates active endocervicitis, which requires treatment.
Asymptomatic gonorrhea is more common in men, so the diagnosis can be confirmed if polymorphic diplococci are detected in a swab from men. If the bacteria are detected, both partners should be tested. The tests used to detect systemic gonococcal infection are polymerase chain reaction (PCR, also called nucleic acid amplification) to identify genes unique to N. gonorrhoeae. These PCR-based tests require a urine specimen, urethral swab, or vaginal swab. Culture (growing colonies of bacteria to isolate and identify them) and Gram stain (staining the walls of bacterial cells to detect morphology) can also be used to detect the presence of N. gonorrhoeae in specimens other than urine. All individuals who test positive for gonorrhea should be tested for other sexually transmitted diseases, such as chlamydia, syphilis, and human immunodeficiency virus.
Diplococci during pregnancy indicate gonorrhea, so the pathology must be treated with approved antibiotics, since there is a risk of infection of the fetus if the woman becomes ill before giving birth.
Complications and consequences
The consequences of a past infection caused by diplococci can be very serious and depend on the type of pathogen and timely treatment. Complications of a respiratory tract infection can be in the form of spread of the infection to other organs. Complications of M catarrhalis infection can include the following: bacterial sepsis, meningitis, mastoiditis, hearing loss, formation of pleural effusion, infectious shock.
Even with antibiotic treatment, 10 to 15 out of 100 people infected with meningococcal disease die. The consequences of meningitis can include deafness, problems with the nervous system, or brain damage.
The consequences of untreated gonococcal infection can become a problem in conceiving a child.
Treatment diplococci in the smear
Treating Moraxella Catarrhalis infections requires good home care. There are specific ways you can improve the treatment process with home care methods for this infection.
Fever is one of the symptoms of Moraxella Catarrhalis infection. If you suffer from a fever above 38 degrees, you need to take medications such as ibuprofen or paracetamol.
It is important to ventilate the room frequently as Moraxella Catarrhalis is easily transmitted through respiratory secretions; it is important to be careful and keep the room clean. Sinus infections and coughs are relieved by moist air.
It is important to remember that smoking in the home can transmit or increase the likelihood of Moraxella Catarrhalis infection in the room if the smoker suffers from it. It is important for every home to wash hands properly and stay away from the infection.
Proper nutrition is very important for treating Moraxella Catarrhalis infection. Eat fresh foods and drink plenty of fluids.
Drug treatment usually involves treating the individual symptoms seen with Moraxella Catarrhalis infection. However, the overall treatment for Moraxella Catarrhalis involves antibiotic treatment. This pathogen requires newer and stronger antibiotics because there is a high rate of antibiotic resistance with this strain. The most effective antibiotics prescribed by doctors to treat Moraxella Catarrhalis include the following:
- Cephalosporins (including Zinacef, Ceftriaxone).
- Amoxicillin-clavulanate (penicillin preparations).
- Azithromycin (Macrolide preparations).
- Erythromycin (Macrolide preparations).
- Clarithromycin (Macrolide preparations).
- Trimethoprim-sulfamethoxazole.
- Fluoroquinolones (Ciprofloxacin, Levofloxacin).
Because meningitis caused by N meningitidis cannot be distinguished from other types of meningitis at onset, empirical treatment with an antibiotic with effective CNS penetration is used. Pending definitive identification of the causative organism, immunocompetent adults suspected of having meningococcal infection receive a third-generation cephalosporin and dexamethasone. A 7-day course of intravenous ceftriaxone or penicillin is adequate for uncomplicated meningococcal meningitis.
Once the diagnosis of meningococcal meningitis has been established, appropriate modifications can be made. Currently, a third-generation cephalosporin (ceftriaxone or cefotaxime) is the drug of choice for the treatment of meningococcal meningitis and septicemia. Penicillin G, ampicillin, chloramphenicol, fluoroquinolone, and aztreonam are alternative therapies. The use of dexamethasone in the treatment of bacterial meningitis in adults remains controversial. It may be used in children, especially in those with meningitis caused by Haemophilus influenzae. In adults with suspected bacterial meningitis, especially in high-risk cases, adjunctive dexamethasone may be helpful.
- Cefotaxime is an antibiotic used to treat diplococcal infections of any localization. The dosage of the drug is 2 g 4 times a day, the method of administration is intravenous infusion. The drug can be administered together with detoxification therapy. Side effects can be in the form of anaphylactic reactions and allergic skin rashes. Precautions - if patients are allergic to penicillins, the drug should be used only after testing.
- Ceftriaxone 2 g is a broad-spectrum drug, especially effective in the treatment of diplococcal infection. The dosage of the drug is 2 g per day, three or four times a day. The method of administration is intravenous or intramuscular. Side effects may be allergic in nature, and there may also be headache, nausea.
- Vancomycin is a reserve antibiotic used in immunocompromised or elderly individuals at risk of severe concomitant infection. The dosage of the drug is 30 to 60 mg/kg per day. The route of administration can be intramuscular at a small dose or intravenous. Side effects include allergic disorders, visual impairment, dysbacteriosis.
- Corticosteroids reduce the incidence of neurological complications in children and adults. When corticosteroids are used, they should be given before or after the first dose of antibiotics. Dexamethasone is a hormonal drug that acts through anti-inflammatory activity. The dosage of the drug is 0.15 mg / kg per administration, possibly repeated after 6 hours. The dosage in children is given for 4 days. The route of administration can be any - intramuscular, intravenous or rectal. Adverse reactions with short-term use are uncommon.
Depending on how severe the infection is, people with meningococcal disease may need other treatments, including: breathing support, medications to treat low blood pressure, wound care for body parts with broken skin.
How to treat diplococci in a smear with genital lesions? Treatment of gonorrheal inflammation has its own characteristics. Due to resistance to oral cephalosporins, only 1 regimen is recommended - this is dual therapy with ceftriaxone and azithromycin for the treatment of gonorrhea. Therapy with ceftriaxone and azithromycin should be administered together on the same day, preferably simultaneously and under direct observation. The combination with azithromycin compared to doxycycline is preferable due to more convenient dosing, probably better patient compliance.
Uncomplicated urogenital, anorectal and pharyngeal gonococcal infection has the following treatment regimen: Ceftriaxone 250 mg intramuscularly single dose plus
Azithromycin 1 g once. Ceftriaxone is safe and effective in pregnant women.
In disseminated gonococcal infection, it is important to evaluate for meningitis and endocarditis. Inpatient treatment is recommended for people who have purulent arthritis or who have other complications.
Recommendations for the treatment of gonococcal meningitis and endocarditis are to use Ceftriaxone 1-2 g every 12-24 hours plus Azithromycin 1 g for 1 dose. Antimicrobial susceptibility testing and the patient's clinical response to empirical therapy are of key importance.
Traditional methods of treatment and homeopathy are not used in such cases, since this is a very serious infection that quickly leads to complications if antibacterial therapy is delayed.
Surgical treatment is used very rarely, only when complications form in the form of abscesses that need to be cut.
Prevention
Prevention of diplococcal infection can be specific only to meningococcus. If a person wants to prevent such a disease, a vaccine against this pathogen is recommended. The prognosis for this infection is positive only in case of timely therapy, since in the absence of treatment the mortality rate is high.
Prevention of gonococcal infections is based on education, mechanical or chemical prophylaxis, and early diagnosis and treatment. Condoms offer partial protection, while effective antibiotics given in therapeutic doses immediately before or shortly after exposure may mediate infection. Preventive measures also include attention to partner notification. Patients should be advised to notify their sexual partners of their exposure and encourage them to seek medical care. If patients are unwilling or unable to notify their partners, then state and local health departments may be called upon to assist.
Prophylaxis in neonates born to mothers with untreated gonococcal infection consists of prophylactic treatment with a single dose of ceftriaxone (25-50 mg/kg not to exceed 125 mg). All neonates should receive ophthalmic syndrome prophylaxis with aqueous silver nitrate (1%) once or erythromycin ophthalmic ointment (0.5%) in both eyes once.


 [
[