
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Bacilli and cocci in the smear: causes of appearance, norms
Medical expert of the article
Last reviewed: 05.07.2025
Cocci in a smear can be detected for various reasons. They can be representatives of normal microflora, or pathogens of infectious diseases. Normal human microflora is a qualitative and quantitative ratio of microbial populations that normally colonize individual, non-sterile forms and systems of the macroorganism and actively participate in supporting its biochemical, metabolic and immune homeostasis, which is necessary for maintaining health.
Normal microbial biocenoses are relatively stable biological structures that remain extremely sensitive to many factors of the internal and external environment. When these factors exceed the compensatory capabilities of the microbial ecosystem, a pathological change in the composition and functions of the endogenous microflora occurs, its symbiosis with the microorganism is destroyed, and dysbiosis of varying severity develops.
Microorganisms act as pathogenic forms when there is a violation of the normal microbiocenosis. This most often occurs against the background of hormonal disorders, decreased immunity, and diseases of internal organs. The microbiota of various biotopes is formed by representatives of various genera and families of microorganisms. Among them are both rod-shaped and bacilli-shaped forms, as well as cocci.
What does it mean?
Cocci are a designation of bacteria that have a round shape. This group includes a large species diversity of microorganisms, and unites various taxonomic units: staphylococci, streptococci, enterococci, peptococci and others. They are opportunistic microorganisms, that is, normally they do not cause diseases, but perform protective functions of the body, whereas in pathology, they can become pathogens.
In most biotopes they are representatives of indigenous, that is, permanent microflora, their number fluctuates within 3-4%. In some biotopes they are representatives of transient microflora, that is, temporary, or that which accidentally entered the body. When exposed to unfavorable factors of the external and internal environment, dysbacteriosis develops, which leads to the fact that the number of opportunistic microflora increases sharply, which can lead to the occurrence of diseases.
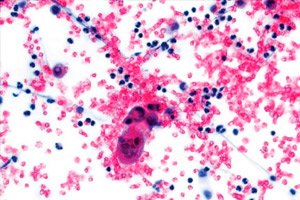
Most of them can be detected in a smear due to their unique shape and color. They are all very similar in morphology: spherical and oval cells. They can be single, or located in pairs, or short chains. Gram-positive, do not form spores. Most are facultative anaerobes, chemoorganotropes with fermentation-type metabolism. They ferment various carbohydrates with the formation of lactic acid as the main fermentation product. They grow within 10-45 degrees, catalase-negative.
Norm of cocci in smear
Cocci are isolated from all biotopes in various quantities, in absolutely all smears, in all 100% of cases. Their quantity varies depending on the biotope. Thus, in the cavity microflora of the stomach, intestines, one can find from 10 8 to 10 12 CFU/ml, in the oral cavity cocci are found no more than 10 8 CFU/ml. Vaginal microflora should normally not exceed 10 3 -10 4 CFU/ml. In the microflora of the respiratory tract, no more than 102 -10 3 CFU/ml is normally present. Microflora should be completely absent in biological fluids such as urine, blood, cerebrospinal fluid, tear fluid, which should normally be sterile.
Smear for infections
If a bacterial infection is suspected, a smear is taken for infection for further bacteriological testing. The smear is taken by a laboratory technician. The material to be tested depends on the specific disease and the location of the pathological process. The laboratory technician collects the sample in sterile containers, observing all aseptic rules. The material is then delivered to the laboratory as quickly as possible for the actual testing.
First of all, the primary seeding of the material under study is performed on artificial nutrient media. Universal media are used. Then, incubation is performed under optimal conditions (in a thermostat) for 3-5 days. Every day, Petri dishes are checked and the growth of microflora is recorded.
After colony growth is detected, when they reach a sufficiently large size, the largest and most specific colonies are reseeded. After reseeding, a separate seeding is made in test tubes with slanted agar. This allows for the isolation of a pure culture of the pathogen. Incubate in a thermostat for another 3-5 days. After the culture has grown, it is identified, that is, the species and genus of the pathogen, its main characteristics are determined. This is done using biochemical, immunological, serological tests. As a result of such a study, a conclusion is issued indicating the species that are pathogens and their quantitative indicator.
Does it hurt when they take a smear?
Taking a smear is completely painless, since no invasive interventions are performed, the integrity of the skin and mucous membranes is violated. In order to take a smear, it is necessary to run a special cotton swab or another pre-prepared instrument along the surface of the mucous membrane, collect its contents. Then it is quickly placed in a sterile test tube with a saline solution or primary nutrient medium.
Despite the relative simplicity of the study, taking a smear is quite difficult, and only a qualified specialist can handle it. A mandatory condition is maintaining sterility. It is also necessary to do everything as quickly and carefully as possible so as not to damage either the human mucosa or the obtained biological material. It is very important to observe all the nuances and details, since they have the greatest impact on the result. It is necessary to remember that microflora is extremely sensitive to various external influences, so it is necessary to strictly follow the rules for its transportation, storage, and research.
Reasons for the appearance of cocci in a smear
It is not entirely correct to talk about the reasons for the appearance of cocci in a smear. This is due to the fact that they are representatives of normal microflora, and therefore their allocation in a smear is the norm, they are always allocated, in all 100% of cases. It is appropriate to talk about the appearance of a high degree of cocci in a smear when their quantitative indicators significantly exceed the norm.
There can be many reasons for the disruption of the microbial status of a person. In particular, the etiology of primary dysbiosis is associated with the deterioration of the reproductive health of women and men, with artificial feeding of infants and irrational use of drug therapy in neonatology. This is the primary stage, which is laid down initially, and on the basis of which further microecological disorders are formed.
The influence of unfavorable environmental factors on the state of microbial ecosystems is of great importance. Man-made pollution, which is accompanied by increased toxicity of atmospheric air, natural waters, and food products, has an extremely negative effect on the state of microflora. This is especially true for industrial poisons, pesticides, heavy metals, and other chemical compounds that, when they enter the human body with food, air, and water, can cause microecological disorders.
Toxic substances that enter the body with polluted air penetrate into the internal environment of the body mainly through the lungs. From there, polluted air molecules are easily carried throughout the body through the blood. Normal functioning of the body implies the mandatory maintenance of homeostasis of the entire body, and an extremely important role in this is played by the mucous membranes and skin, which directly or indirectly react with the internal environment.
The body's defenses are directly related to the state of these barriers and the state of their microflora. Given that the external environment changes the conditions for the existence of microorganisms extremely quickly, not only the microbiota itself but also the immune system reacts. As a result, there is a rapid evolution of microorganisms in the direction of adaptation to changing environmental conditions, as well as various dysfunctions of the immune system.
Significant factors of exogenous origin are unfavorable sanitary and hygienic living conditions and climatic and geographical changes.
Of the endogenous factors, age-related changes, antibiotic therapy, and chemotherapy have the most negative impact. Hormonal drugs, cytostatics, and expectorants have the most unfavorable impact.
Cocci in a nasal smear
Microorganisms mainly enter the upper respiratory tract with dust and are suspended in its particles. They settle primarily on the ciliated epithelium of the nasal cavity, which is the first defense mechanism on the path of infection. Normally, they are excreted by the movements of the villi of the epithelium.
One part of the microflora is retained by microvilli and excreted, the other part dies under the action of the secreted mucous secretion (lysozyme), which provides a high level of colonization resistance. It is due to these properties that the mucous membrane of the trachea, bronchi, alveoli usually remain sterile. Microorganisms such as streptococci, lactobacilli, coryneform bacteria are found in the nasal cavity. Bacteroides, peptococci, peptostreptococci, staphylococci, and other microorganisms are present in smaller quantities.
Cocci in a smear from the urethra
The microflora of the urogenital tract of men is represented mainly by anaerobic microflora, which mainly includes bifidobacteria, lactobacilli, propionic acid bacteria. Clostridia and bacteroids are present in much smaller quantities.
Anaerobic and facultative-anaerobic microflora are represented mainly by coccal forms of microorganisms, such as: peptococci, peptostreptococci, staphylococci and streptococci. They form the basis of facultative microflora, in percentage terms the number of microorganisms of this group does not exceed 3-4%. These are opportunistic forms, which under unfavorable conditions can colonize mucous membranes and cause various diseases of the genitourinary system.
Cocci in a vaginal smear
Vaginal biocenosis plays an extremely important role, since it determines not only the microecological state of the mother, but is also the basis of the primary microbiocenosis for the newborn child. Violation of the normal microflora of the female genital organs primarily entails an increase in the number of microbiotic disorders in the population as a whole.
The normal vaginal biocenosis of a woman is very specific. It is vitally important, since it performs a wide range of protective, metabolic, and regulatory functions of the body. The composition and properties of the vaginal microbiocenosis are in dynamic equilibrium with the general biological characteristics of the female body and are determined by many internal factors. First of all, the vaginal microflora depends on the hormonal background, since it determines the species composition of microorganisms and determines the predominance of one or another type of microorganism.
The vagina of a woman has an acidic environment, as it contains a large amount of lactic acid, which is present in significant quantities due to the high activity of estrogen. The acidic environment prevents the colonization of the biotope by acid-sensitive microorganisms. Lactic acid bacteria make up approximately 97% of the vaginal microbiota. They are the ones that maintain the colonization resistance of the vaginal mucosa, as a result of which they do not allow the development of pathogenic microflora in the body.
After lactic acid bacteria, bifidobacteria and propionibacteria come in quantitative indicators. Their quantitative indicators vary from 10 4 to 10 7 CFU/ml.
Thus, these three groups of microorganisms form the main, or indigenous microflora, which is basic and physiological for a woman. It is this that determines the protective mechanisms, stimulates local immunity, protects against pathogenic forms of the disease, including fungal infection.
At the same time, vaginal secretion normally always contains obligate microflora, which is represented by opportunistic microorganisms. Cocci predominate in this group. Normally, their number should not exceed 10 3 CFU/ml. If their number exceeds these indicators, an infectious disease of bacterial origin may develop.
Depending on the type of cocci that predominates in the smear, one or another pathology develops. For example, with the predominance of peptostreptococci, septic abortions, tubo-ovarian abscesses, endometritis, and postoperative infectious complications develop. If microorganisms of the genus staphylococcus predominate, bacterial vaginosis, sepsis, urogenital infections of various localizations, and toxic shock syndrome develop. With the development of enterococci and streptococci, sepsis, peritonitis, pyelonephritis, cystitis, urethritis, salpingitis, postoperative complications, chorioamnionitis, and premature birth develop.
Risk factors
The risk group includes people with reduced immunity, after recent infectious, viral, somatic diseases, serious operations, organ transplantation. Antibiotic therapy, chemotherapy, treatment with hormonal drugs, cytostatics also have a negative effect on the state of the microflora. The development of coccal infection can be observed in the postoperative, postpartum period, since the body is weakened, and nosocomial infection is present in almost all maternity hospitals and surgical departments. For the same reason, newborns, whose immune system is not yet formed, are also at risk.
The risk group also includes people who, due to their professional duties, constantly encounter biological material, tissue cell cultures. These may be laboratory technicians who examine human samples, research workers, microbiologists, bacteriologists, mycologists, whose work is inevitably associated with biological material and microorganisms.
Symptoms
Symptoms may be varied and are determined primarily by the localization of the infectious process. If the microflora of the gastrointestinal tract is disturbed and a high content of cocci is found in the smear, the person will feel nausea, stool disturbance. Vomiting, stomach pain, bloating, heartburn may appear. Later, an inflammatory process develops.
If cocci predominate in the respiratory system, nasal congestion, runny nose, and sore throat develop. Pain and swelling in the throat appear, and an inflammatory process develops. If treatment is insufficient or immunity is reduced, a person may experience progression of the infection. It can move downwards along descending pathways, causing inflammation in the bronchi and lungs.
If a large number of cocci are detected in a urogenital smear, urethritis and vaginitis develop predominantly. White or cloudy discharge from the genitals appears, itching and an unpleasant odor develop. Later, pain in the perineum and rectum may develop.
Long before the level of opportunistic microflora reaches a critical limit and a bacterial disease occurs, precursors, or first signs, appear in the body. Their manifestation is determined by the gradual growth of microflora, the increase in the body's antibody titer in response to a bacterial infection.
Thus, the increase in the number of cocci in the body can be predicted by the appearance of rapid heartbeat, slight shortness of breath, chills. The temperature may rise without reason. Most often, this does not occur in high limits - up to 37.2, without any accompanying pathologies. A person feels increased fatigue, decreased endurance and performance, weakness. Quite often, weakness is accompanied by trembling in the limbs, increased sweating.
Single cocci in smear
Usually, single cocci in a smear indicate dysbacteriosis, in which other forms of microorganisms develop and less competitive forms are displaced. This is how the number of cocci in a smear decreases. Single cocci can also be found in fluids that are normally sterile.
Single cocci in sterile fluids are an extremely alarming sign and indicate the development of bacteremia, in which the infection from the site of inflammation penetrates into other fluids, such as blood and urine. Such a pathology requires urgent treatment, since bacteria will begin to actively multiply. The next stage will be the development of sepsis, in which a high content of bacteria is detected in sterile fluids, blood poisoning occurs, and the infection spreads throughout the body. A major problem is the development of intoxication with endotoxins, which are produced in this case. If urgent measures are not taken, such a pathology will end in death.
Cocci in smear in moderate quantity
In fact, in bacteriology there is no such thing as a "moderate amount". Laboratory studies love precision, and all indicators must have a clear quantitative expression. Conventionally speaking, a moderate amount can be taken to be 10 4 -10 6 CFU/ml cocci, at which the indicators already significantly exceed the norm, but are not yet a critical indicator, against which the development of a bacterial infection occurs. This indicator can be characterized as a critical level, a limit, above which there is an absolute pathology.
Many cocci in the smear
Of course, the test results will not say "many" cocci. And this concept is very conditional, since the only reliable indicator is a numerical characteristic expressed in CFU/ml, that is, the number of colony-forming units of bacteria in 1 milliliter of the suspension being studied. Conventionally, a large number can be taken as an indicator over 10 5 -10 6 CFU/ml, at which a disease of bacterial etiology develops. This indicator will vary depending on the biotope and type of microorganism. In some biotopes, the norm is 10 9 -10 10. This applies, for example, to peptostreptococci, which are found in such quantities in the intestinal microflora of a healthy person.
Cocci and increased leukocytes in smear
The number of leukocytes increases sharply in the presence of an inflammatory process. Any inflammation usually causes a disturbance of the microflora. The number of opportunistic flora (cocci) significantly exceeds the norm. These two processes are interconnected and interdependent. Inflammation provokes increased growth of bacterial microflora, mainly opportunistic and pathogenic. Also, a high number of bacterial microflora can lead to an inflammatory process.
Cocci and clue cells in smear
Key cells are the main formed elements of the blood, which are found in the blood plasma. In the smear, cocci and leukocytes are most often found, which indicates the development of an inflammatory, purulent-inflammatory process. The appearance of erythrocytes in the smear indicates bleeding, the development of anemia and blood diseases, including cancer. Platelets in the smear rarely appear, but they can indicate the development of an inflammatory process in the vessels, microcirculatory bed, increased permeability of the vascular walls.
Types of cocci in a smear
A smear may contain a wide variety of microorganisms. Thus, despite the fact that cocci are opportunistic forms of microorganisms, the percentage of which does not exceed 3-4%, their species diversity is very wide, with over 28 species in each biotope. Let's consider the main representatives that are found in all biotopes and are universal.
Peptostreptococci are strictly anaerobic gram-positive forms of microorganisms that are often found in very high concentrations in the body of a healthy adult. They are virtually absent from the biotopes of infants who are breastfed. They are often isolated from sources of infection in septicemia, osteomyelitis, purulent arthritis, appendicitis, gingivitis, periodontosis and other diseases. They ferment carbohydrates to form a wide range of acids and gas.
Peptococci are small spherical cells, the diameter of which does not exceed 1.2 µm. They are located in pairs, tetrads, groups or short chains, gram-positive, non-motile, and non-spore-forming.
They are chemoorganotrophs with fermentation metabolism, requiring enriched nutrient media. They do not ferment carbohydrates, they decompose peptone with the formation of hydrogen. The concentration of peptococci in human biotopes under normophysiological conditions is insignificant. Provided that the population increases, peptococci are an etiological factor in the development of the infectious and inflammatory process.
Enterococci are the main representatives of the colon biotope. Morphologically, all representatives of the genus are very similar to each other. The cells are oval or spherical. All of them are facultative anaerobes, chemoorganotrophs with fermentation-type metabolism. They ferment various carbohydrates with the formation of lactic acid as the main fermentation product. Catalase-negative, grow at temperatures ranging from 10 to 45 degrees. They differ from streptococci in their high resistance to bile and sodium chloride.
Differential features that allow them to be distinguished from other cocci, as well as from streptococci, are the ability to reproduce at temperatures from 10 to 45 degrees, resistance to high concentrations of sodium chloride, resistance to penicillin, and an acidic environment.
Until recently, enterococci were considered exclusively as symbionts of the human intestine, but today their etiological role in the development of infectious pathology has been established. In addition, they are permanent inhabitants of other biotopes, such as the oral cavity, vagina, urethra. They are distinguished by high resistance to antibacterial drugs, which tends to constant, steady growth.
Gram-positive cocci in smear
Gram-positive cocci are round or spherical microorganisms that give a positive result when stained using the Gram method. They are normal representatives of microflora, but under unfavorable conditions, they can become pathogens of many infectious diseases.
Most often, they cause the development of diseases of the liver, kidneys, blood, abdominal cavity and genitals, soft tissues and mucous membranes. They cause postoperative complications, postpartum infections, purulent-inflammatory and septic diseases of newborns. They are dangerous hospital infections, the resistance of which is constantly progressing.
Gram-positive microorganisms are well adapted to life in various biotopes of the human body, and also have a wide range of aggressive factors, which allows them to migrate into the external environment of the body under certain conditions, causing infectious and inflammatory diseases, and in people with immunodeficiency - bacteremia, sepsis and septicopyemia. It is known that in 21% of cases they are the cause of neonatal infection, almost half of which ends in death. In 5-10% of cases they are the causative agents of gynecological diseases.
It is known that under the influence of certain antibiotics, many gram-positive microorganisms can increase their natural ability to suppress phagocytosis and protect against immunoglobulins. In addition, gram-positive cocci cells can transform into resistant L-forms, which allows them to persist in the human body for a long time.
Numerous studies have shown that most cases of microecological disorders are accompanied by an increase in the level of gram-positive microflora. Such changes are especially dangerous for newborns, since the risk of developing defective microbiocenoses, biofilms, associations with the predominance of opportunistic microflora and altered functions increases significantly. In newborns, such conditions are characterized by a high rate of development and quickly lead to the development of bacteremia and sepsis.
In 35% of cases, bacteremia in newborns is fatal. Given the ever-increasing amount of data on the role of gram-positive cocci as dangerous nosocomial pathogens with increasing multidrug resistance, the aggressive potential of these microorganisms cannot be underestimated. Among the representatives of gram-positive flora, the most dangerous are Staphylococcus aureus, Pseudomonas aeruginosa and Enterococcus faecalis.
The high risk of infection is associated with increased resistance of microorganisms to drugs. Rapid mutation contributes to the accelerated acquisition of artificial resistance, which complements the natural one. No less dangerous are such virulence factors as the synthesis of cytolysins. The mechanism of protection from the host immune system is very significant from the point of view of the genetics of microorganisms. The ability to protect against neutrophil-mediated phagocytosis and killing, as well as the cytotoxic effect on polymorphic neutrophils and macrophages, has been described.
They are able to protect themselves from the action of molecular oxygen and peroxide by synthesizing certain enzymes. Due to these properties, they can persist for quite a long time in the lesion. Strengthening occurs due to the presence of a mechanism for obtaining, accumulating and transmitting extrachromosomal elements.
Thus, the excess of gram-positive microflora in the smear, above physiological norms, indicates the development of dysbacteriosis, which is a dangerous condition that requires treatment. The most effective are probiotic drugs.
Gram-negative cocci in smear
Gram-negative microorganisms are mostly aerobic or facultative-anaerobic representatives of the normal microflora of the large intestine. But they can also be found in other biotopes. Some representatives are capable of synthesizing vitamins, in particular, groups B and K, antibacterial substances, fatty acids. However, with a decrease in the population and weakening of the protective properties of obligate microorganisms, their number increases sharply, as a result of which numerous pathological phenomena will develop.
Microorganisms are round and small in size. Many of them move by peritrichous flagella. They have a wide range of enzymatic activity. They are capable of fermenting a large amount of alcohols to form pyruvate, which is then converted into acids.
One of the most dangerous complications caused by gram-negative flora is the ability of these microorganisms to migrate, which is accompanied by infection of parenchymatous organs with the development of numerous extraintestinal infections, such as sepsis, meningitis, pyelonephritis, peritonitis and others.
It should be noted that infectious complications caused by gram-negative forms are one of the most serious problems today. This is usually observed with a decrease in the colonization resistance of the macroorganism due to a decrease in the concentration of obligate microflora representatives and immune system insufficiency. In such conditions, the level of the aerobic population of the biocenosis and its aggressive properties usually increase, which allow this microflora to overcome the barrier of the preepithelial layer and promote the translocation of their cells into the internal environment of the body. The process is observed with massive antibiotic therapy, chemotherapy, which suppress the indigenous flora and promote selective proliferation of bacteria with high drug resistance.
Fungi and cocci in smear
Any growth of fungal microflora occurs against the background of dysbacteriosis, which is inevitably accompanied by an increase in bacterial microflora at the same time. First of all, active growth of cocci occurs.
Of the fungi in the human body, the most common are Candida albicans and Candida tropicales. The main biotope is the intestine. In a healthy person, no more than 104 CFU/ml is detected. An increase in the concentration of fungi, especially in immunocompromised individuals, can be accompanied by the development of mycoses.
Candida is widespread in the environment. Viable cells of these microorganisms can be found in soil, drinking water, food, skin, and human mucous membranes. That is, constant human contact with representatives of the genus Candida is inevitable, but the result of this contact is not the same for different individuals and is determined by the state of the colonization resistance system in the body.
In recent years, mycoses caused by excessive growth of Candida fungi in biotopes have acquired the status of a serious clinical problem. Oropharyngeal and vaginal candidiasis, intestinal candidiasis, oral candidiasis, and lung candidiasis are becoming more widespread. A serious problem is the increase in cases of visceral candidiasis, which affects the lungs, intestines, liver, pancreas, and other organs, leading to the development of candidal sepsis, which often ends fatally.
Actinomycetes are also quite often found in the smear. These fungi are widespread in nature, so they constantly enter the human digestive tract. Some have adapted to existence in certain biotopes during phylogenesis and ontogenesis. Actinomycetes are especially often isolated from the oral cavity.
In terms of their level of organization, they occupy an intermediate position between bacteria and fungi. Morphologically, they are extremely polymorphic. The cells are straight, slightly curved rods, rye threads with pronounced branching. They often form clusters. They are similar in many ways to propionic acid bacteria. They are gram-positive, non-motile, asporogenous, facultatively or obligately aerobic, with varying acid sensitivity.
They are distinguished by their low demands on the composition of the environment due to their high biosynthetic capabilities. Enzymatic activity is quite diverse. Among these microorganisms, there are saccharolytic forms that ferment a wide range of carbohydrates using various pathways of anaerobic metabolism and their combinations. It is known that among actinomycetes there are superproducers of antibiotics, which are quite successfully used in industrial microbiology.
Despite the beneficial properties of many actinomycetes, an increase in their concentration in human biotopes should be considered as pathological changes in the composition of the microbiota, since actinomycetes, especially their obligate anaerobic groups, have quite a lot of pathogenic forms. The danger of a pathological increase in actinomycete populations in human biotopes is the high viability of these organisms, which is not inferior to the resistance of spore-bearing pathogens to unfavorable changes in environmental conditions.
Polymorphic cocci in smear
Almost all cocci have polymorphism – the ability to change their shape in the process of adaptation to the conditions of existence. Basically, their shape varies from round to spherical. Some of them can combine into complexes, forming diplococci, chains, threads and even clusters.
Rods and cocci in a smear
The smear may contain cocci, the number of which increases sharply during the development of the inflammatory process, against the background of decreased immunity. They have a round or oval shape. Normally, they are representatives of normal microflora, in pathology - they cause various infectious diseases.
An increase in the number of cocci is often accompanied by an increase in other opportunistic flora, in particular, rods. These forms of microorganisms received this name due to the fact that they look like rods. They can be of different sizes, density, and color. A typical representative of rod-shaped forms is the intestinal bacillus – Escherichia coli. Representatives of the genus Bacillus are also included here. Normally present in the large intestine, are part of the normal microflora. They are facultative anaerobic forms.
In the treatment and diagnosis of intestinal dysbacteriosis, the primary role is given to determining the quantitative and qualitative indicators of E. coli. Normally, it stimulates immunity, normalizes intestinal peristalsis and motility, normalizes digestive processes, improves absorption and assimilation of nutrients, synthesizes hormones and other active components.
The rods are usually mobile, move with the help of peritrichous flagella, and are stained negatively by Gram. They are located separately or in pairs. They have a wide range of enzymatic activity.
If the concentration exceeds the permissible level, infectious diseases develop: diseases of external and internal organs, kidneys, liver, spleen. In case of massive damage or infection, severe infectious processes are possible, which often end in death. Many representatives of this group are capable of synthesizing toxins that are released into the internal environment, as well as into the external space.
Cocci and diplococci in a smear
Cocci in a smear often combine with each other, forming pairs. Such doubled cocci are called diplococci, where the prefix "diplo" means two, that is, two cocci. Their properties do not change from this. They still remain representatives of normal microflora, providing reliable protection of the corresponding biotope. If the norm is exceeded in quantitative terms, an infectious disease develops.


 [
[