
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Escherichia coli in a smear culture: symptoms, how to treat
Medical expert of the article
Last reviewed: 05.07.2025
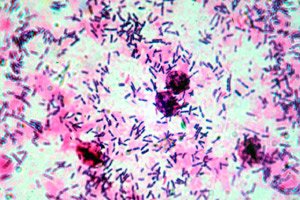
The rod-shaped microorganism called E. coli (or Escherichia coli) belongs to the series of facultative anaerobes. This bacterium is one of those that represent the natural microflora of the human intestine: its important mission is to prevent the proliferation of pathogenic flora and promote the synthesis of vitamin K and other useful substances. It is clear that the intestine is a familiar environment for such bacteria; but should E. coli be in the smear?
Norm of E. coli in smear
In a healthy organism, E. coli is represented by safe strains, the average number of which fluctuates between 10 6 and 10 8 CFU/g of contents in the distal intestinal section. The concentration of E. coli in other parts of the intestine should not exceed 1%.
Normally, this bacterium maintains the necessary function of the intestine, takes part in the synthesis of vitamin K and B vitamins. Lactose-negative rods should not be present in quantities exceeding 10 5 CFU/g, and hemolytic rods should not be present at all.
E. coli can be present in a completely normal vaginal environment, but in minimal quantities, since its development is normally restrained by lactobacilli living inside the vagina. If the content of lactobacilli decreases for various reasons, then E. coli can successfully reproduce, and along with it, other microorganisms (staphylococci, candida, etc.).
Causes of E. coli in the smear
It is worth noting that in minimal concentrations, E. coli cannot be detected in a smear. If the bacteria is detected, then in most cases it is already present in large quantities. How can E. coli be found in vaginal smears? Here are several possible reasons:
- with insufficient hygiene of the genitals;
- when changing underwear infrequently;
- during mixed sexual intercourse (anal-vaginal contact);
- during sexual intercourse on the beach, in water, etc.;
- when using other people's washcloths, towels, and linens.
E. coli may appear in urine and smears for the following reasons:
- during anal sex in men (bacteria enter the urethral canal);
- at low pH of urine fluid;
- in case of rare urination (in case of kidney diseases, prostate adenoma, etc.);
- in inflammatory processes in nearby organs (infection can spread through the lymphatic vessels, etc.);
- if hygiene rules are not followed correctly;
- during pregnancy (due to weak immune defense and changes in hormonal activity).
E. coli in a throat swab is found via the oral-fecal route. With feces, the bacteria enters water bodies or soil, onto plants. After that, infection can occur in several directions. For example, a person can rinse their mouth with dirty water, chew unwashed vegetables or greens, or take food with unwashed hands. Thus, E. coli ends up not only in the throat, but also in the digestive tract.
E. coli may appear in a cervical canal smear for the same reasons and in the same ways as in the vagina.
Risk factors
As is known, E. coli is a microbe that is necessary for the body. However, it can become pathogenic under the influence of certain risk factors:
- in case of a sharp weakening of the immune system (for example, with frequent colds, acute respiratory viral infections, after operations, against the background of various chronic diseases);
- after long-term antibiotic therapy with the use of powerful drugs (or a combination of antibiotics);
- with frequent consumption of unwashed plant foods (greens, vegetables, berries, fruits);
- when ignoring hygiene rules.
How is E. coli transmitted to a partner?
E. coli can be transmitted to your partner through the feco-oral or contact-household route.
The fecal-oral method involves the bacteria getting into the soil or water with feces. Then the microbe enters the human body - for example, with contaminated water, when eating unwashed plant food, with unwashed hands, etc.
The contact route of infection is the use of common towels, linen, etc. However, most often E. coli is transmitted from one partner to another sexually - during sexual intercourse. The risk factors in this case are:
- failure to observe personal hygiene rules;
- anal sexual contact.
There are known cases when E. coli was transmitted to a partner during sexual intercourse with a man who has chronic prostatitis, orchitis or epididymitis, the causative agent of which is this bacterium. In this situation, E. coli enters the vagina along with the sperm.
Symptoms of E. coli in the smear
In most patients, the presence of E. coli in a smear is not accompanied by any symptoms. Bacteria are detected during a routine preventive examination. However, with the intensive development of pathogenic flora, an inflammatory process can start, affecting the urinary and reproductive organs.
E. coli is often the "culprit" of cystitis: in this case, it is detected in the urine and urethral canal. Symptoms may include:
- frequent urination;
- the presence of urges even with a small amount of urine in the bladder;
- general malaise, fever, muscle pain;
- pain when urinating.
If E. coli is detected in a vaginal smear, vaginitis develops with active bacterial reproduction. Its symptoms are most often as follows:
- the appearance of foreign discharge from the vagina;
- painful, itchy sensations, irritation of the vaginal mucosa;
- discomfort during sexual intercourse;
- external swelling of the external genitalia, unpleasant odor.
Against the background of vaginitis, other inflammatory diseases affecting the pelvic organs can develop (for example, salpingitis, endometritis, endocervicitis). The listed pathologies reveal themselves by pain in the lower abdomen, the appearance of vaginal discharge, menstrual cycle disorders, and difficulties with conceiving a child.
In the ascending type of infection, E. coli can cause the development of pyelonephritis.
In men, the bacteria most often provokes the development of urethritis. The first signs of this disease are:
- the appearance of urethral discharge;
- painful urination;
- pain during sexual intercourse;
- redness around the external urethral opening.
 [ 11 ], [ 12 ], [ 13 ], [ 14 ]
[ 11 ], [ 12 ], [ 13 ], [ 14 ]
E. coli in smear and secretions
As the inflammatory process develops, the nature of vaginal discharge changes noticeably. If healthy secretion is small in volume, transparent, odorless, and not accompanied by pain or discomfort, then pathological discharge is cloudy and has an unpleasant odor. Its color can fluctuate between yellowish and greenish. The smell is extremely unpleasant, sharp, and cannot be eliminated using regular hygiene procedures.
Pathological discharge is often accompanied by other painful symptoms:
- redness, itching in the genitals;
- a nagging pain in the lower abdomen;
- pain during sexual intercourse;
- general weakness;
- discomfort when urinating.
If you experience any of the above symptoms, you should definitely seek medical help.
 [ 15 ]
[ 15 ]
E. coli and staphylococcus in a smear
Both E. coli and staphylococcus in a smear do not always mean the presence of an infection. In cases where the content of these microbes does not exceed 1% of the total microflora, then it is not necessary to prescribe treatment.
However, given favorable circumstances, both E. coli and staphylococci are capable of starting rapid growth, which is revealed by the following symptoms:
- the appearance of painful, unpleasant discharge;
- itchy discomfort;
- discomfort during sexual intercourse;
- general deterioration of health, irritability;
- redness of the mucous membrane of the genitals, swelling.
If such symptoms are present, then treatment is necessary. To clarify its features, the doctor may prescribe additional diagnostics in the form of the PCR method. The treatment regimen is selected individually and depends on the characteristics of the disease.
E. coli in a smear in women
When E. coli gets inside the vagina and urethral canal, under certain circumstances it causes acute colpitis or urethritis. If timely treatment is not started, the bacteria lingers on the mucous tissues, causing constant relapses of the disease. The mechanism of ascending infection is also not excluded: there is a high probability of developing cystitis, pyelonephritis, endometritis, salpingo-oophoritis. According to statistics, in 80% of cases of female patients, cystitis is provoked by E. coli. Approximately the same percentage of E. coli detection in pyelonephritis and bacteriuria during pregnancy.
In women, inflammatory processes caused by E. coli last a long time and tend to become chronic. Chronic diseases are much more difficult to treat, so it is better not to neglect the disease and consult a doctor as soon as possible.
E. coli in a smear in men
If E. coli gets into the urethra - for example, after anal sex or if hygiene rules are not followed, acute urethritis can develop, which has every chance of becoming chronic if left untreated. In the urethra, the bacteria are tightly attached to the mucous membrane, so regular and even frequent urination is not able to "wash" it out of the canal.
After the process becomes chronic, E. coli moves into the structures located above – the bladder, kidneys, prostate, testicles, also provoking the development of inflammation in them.
It is typical that in men any infection more often affects the reproductive system, and not the urinary system. Therefore, cystitis or pyelonephritis in the male population occurs less often: instead, the strong half of humanity often suffers from sluggish, difficult to cure prostatitis or orchiepididymitis. According to statistics, about two thirds of cases of chronic prostatitis in male patients over 40 years old are provoked by the effects of E. coli.
Even without any painful symptoms, a man can be a carrier of E. coli. Under favorable conditions - stress, hypothermia, the infection can become active and worsen.
E. coli in a child's smear
In small children, E. coli in a smear can be detected in two variants: hemolytic and lactose-negative bacteria. In theory, hemolytic bacilli should not be present in the baby's body - it is a pathogenic microbe capable of causing infectious and inflammatory processes.
But, having found such E. coli, you should not immediately prescribe antibiotics to the child. If the child does not complain about anything, has normal stool, adequate appetite and well-being, then there is no need for antibiotics. But if symptoms such as diarrhea, weight loss and appetite appear, antibiotic therapy is mandatory.
The presence of lactose-negative bacilli is not considered a pathology, since this bacterium should be part of the normal flora. However, this microbe can also cause disease if its quantity becomes excessive. In such a case, the child will have unpleasant symptoms indicating the onset of an inflammatory process. If this happens, then treatment is mandatory.
Complications and consequences
E. coli is of invaluable benefit to the human body. But under certain conditions, this bacterium can also provoke disease, cause intoxication, and weaken local immune defense. Such activation of the bacterium is especially dangerous in a child's body, because it becomes vulnerable to all damaging factors of an aggressive external environment for some time.
With active, rapid growth, microbes cause dysfunction of the affected organ.
The hemolytic strain (one of the varieties of E. coli) produces verotoxins that can cause inflammation and tissue necrosis. The bacteria affect the vascular network, impairing blood circulation in the organ.
When penetrating from the external environment, E. coli damages the tissues of the genitourinary system, causing inflammatory processes in the prostate gland, testicles and appendages in men, or vaginitis, endometritis, salpingo-oophoritis in women.
In newborn babies, exposure to E. coli can lead to the development of meningitis.
A separate disease is hemolytic-uremic syndrome, which develops against the background of weakened immunity. The basic role in the formation of this pathology belongs to enterohemorrhagic intestinal bacteria, which produces a specific Shiga-like verotoxin, which has the property of damaging the vascular epithelium in the kidneys and brain. This pathology is most dangerous for children from the neonatal period to 3 years.
Treatment of E. coli in the smear
If E. coli is present in the smear, but there are no signs of an inflammatory process, then therapy is not prescribed. If there are symptoms of a genitourinary disease, then antibiotic treatment is mandatory.
First, a bacterial culture is done to assess the sensitivity of bacteria to drugs. This is done to understand which antibiotic will be most effective for a particular patient.
Antibiotic therapy is prescribed in a course of 5-14 days. After about 4-8 weeks, a control smear should be taken again to ensure that the pathogen is absent. If the inflammatory process relapses, the antibiotic course is repeated.
The most effective drugs for neutralizing E. coli in a smear may be the following:
- Cephalexin for adult patients is prescribed in a daily amount of 1 to 4 g. Taken every six hours. Duration of treatment is from one to two weeks. For children, a dosage of 25-50 mg / kg of weight is appropriate. Possible side effects include diarrhea, weakness, and allergies.
- Cefotaxime is administered intramuscularly, after dissolving 0.5-1 g of the drug in 2-4 ml of water for injection. Cefotaxime is administered every 12 hours. Possible side effects include allergies, headaches, and inflammation at the injection site.
- Ceftazidime is administered intramuscularly, 1-2 g per day (in two administrations). For children, starting from 2 months of age, a dosage of 25-50 mg/kg per day (in two administrations) is appropriate. Side effects: candidiasis, vomiting, skin rashes, burning when administering the drug.
- Imipenem is administered intramuscularly at 500-750 mg once every 12 hours. Side effects may include: allergy, nausea, convulsions, candidiasis.
- Amikacin is administered intramuscularly: for adult patients and children, a daily dosage of 10 mg per kilogram of weight is used (divided into 2-3 doses). The duration of therapy is from seven to ten days. The drug may have an ototoxic or nephrotoxic effect (impair the quality of hearing and renal function).
- Levofloxacin tablets are taken 60-30 minutes before meals, once a day, with water. Standard dosage for adults: for prostatitis - 500 mg / day, for a month; for uncomplicated urinary tract infections - 250 mg / day for three days. Side effects: nausea, decreased blood pressure, sleep disturbance, headache.
- Ciprofloxacin is taken at 0.125-0.5 g twice a day for 7-14 days. Treatment may be accompanied by nausea, sleep disturbances, changes in taste sensations, and increased skin sensitivity to sunlight.
- Macmiror complex in the form of a suppository is administered intravaginally once a day, at night. The duration of therapy is 8 days (unless the doctor has prescribed otherwise). Suppositories are well accepted by patients: only in isolated cases is it possible that allergies may occur (skin rashes, itching).
Non-pregnant women may be prescribed vaginal antibacterial drugs in the form of suppositories and gels:
- Metrogyl is administered intravaginally 1-2 times a day for 10 days. It is advisable to avoid sexual intercourse during treatment.
- Cleocin is inserted into the vagina at night, one suppository at a time. The duration of therapy is three days in a row. Side effects may include: menstrual cycle disorders, candidiasis, itching, nausea. An analogue of this drug is Klindess.
Also, to suppress the development of a pathogenic strain of E. coli, the doctor often prescribes Miramistin, an antiseptic that enhances the effect of the antibiotic and stimulates local immunity.
To further restore normal healthy flora after antibiotic therapy, medications such as probiotics, antifungal drugs, vitamins, and immunomodulatory agents are prescribed:
- probiotics (Vagilak, Laktogin, Ginoflor) – normalize the quality of the vaginal environment, stabilize the microflora;
- Immunomodulatory agents (Viferon, Likopid, Kagocel) – help strengthen the immune system.
Additionally, it is recommended to adhere to a dietary diet with a predominance of fermented milk products, with the exclusion of sweets. In case of damage to the urinary tract, diet No. 7 should be followed.
Is it necessary to treat E. coli in a smear?
As we have already said, E. coli in a smear taken from the vaginal mucosa may be present in minimal quantities. For example, if the obtained indicator corresponds to 10 3 CFU/g, then no special treatment is required. It is enough to adhere to the rules of personal hygiene, eat right, and maintain an adequate state of immunity.
If rapid development of bacteria is registered, with signs of an inflammatory process, then treatment is prescribed without fail.
Even if the number of bacteria is not very large - for example, E. coli is found in a smear of 10 to the 6th power, but there are clear signs of colpitis, then treatment is essential.
Treatment of a partner when E. coli is detected in a smear
If E. coli is detected in a partner during an examination, but no pathological symptoms are observed, then there is no need to treat such carriage with antibiotics.
If a man suffers from prostatitis, urethritis, or other inflammatory diseases, they must be treated in accordance with generally accepted treatment regimens.
Coliproteus bacteriophage
Coliproteophage is a medicinal product based on live microorganisms capable of normalizing the microflora. The drug can be administered rectally or taken orally (for intestinal or urethral dysbiosis), or inserted into the vagina (for bacterial vaginosis).
The main active substance of coliproteophage is special viruses that have the ability to suppress the activity and development of pathogenic microorganisms. Such viruses are introduced into microbial DNA, causing a destructive effect.
In addition to viruses, the drug contains oxyquinoline, an antibacterial substance that inhibits the development of pathogenic microorganisms (for example, fungal infections).
Coliproteus bacteriophage can be used when detecting Proteus vulgaris, Proteus mirabilis, and Escherichia coli in a smear. Indications for taking bacteriophage include diseases such as cystitis, colitis, enteritis, pyelonephritis, salpingo-oophoritis, pyelitis, and endometritis. In addition to treatment, this drug also has a preventive effect.
The drug is taken orally twice a day, and in the form of rectal or vaginal administration - once a day. The course of treatment is one week.
 [ 25 ], [ 26 ], [ 27 ], [ 28 ]
[ 25 ], [ 26 ], [ 27 ], [ 28 ]
Treatment of diseases accompanied by the appearance of E. coli in a smear, with folk remedies
Recipes offered by traditional medicine can alleviate or minimize painful signs of infection. However, such methods are unlikely to completely eliminate E. coli in a smear.
At the same time, herbal remedies help strengthen the body's own immune defenses and restore the balance of microflora.
To stabilize the composition of the vaginal flora, douching is often used. For example, irrigation and douching with a weak solution (2-3%) of boric or lactic acid give a good effect. The vaginal treatment is repeated every evening for 7 days. Other means are also suitable for douching:
- Take 1 tbsp of the goose cinquefoil plant and the flowers of medicinal chamomile, pour 1 liter of boiling water, keep under the lid for 30 minutes. Then filter the liquid and use for irrigation, washing or douching.
- Pour 1 tbsp of boiling water into a thermos, leave for 3 hours, filter. Douche with warm infusion every night for one week.
- Pour 1 ½ tbsp of bird cherry fruit into a thermos with 0.5 l of boiling water, leave for 20-30 minutes, filter. Use the warm infusion for washing and douching. The course of treatment is daily for a week.
Herbal treatment
If E. coli is detected in a smear and in urine, then you can try the effectiveness of the following folk methods:
- Prepare a mixture based on 2 tablespoons of St. John's wort and 4 tablespoons of meadowsweet. Pour 1 liter of boiling water over the raw materials, leave for an hour and a half, filter. Drink 200 ml three times a day 15 minutes before meals.
- Take an equal collection of chamomile flowers, cornflower, knotweed, corn silk, St. John's wort. Pour boiling water (300 ml) over 1 tbsp. of the collection, leave for an hour. Filter and take 100 ml three times a day, between meals.
- Pour boiling water (0.5 l) over 2 tbsp of dried violet, leave for an hour, filter. Take 1-2 tbsp three times a day.
If the appearance of E. coli in a smear is accompanied by the development of urethritis, the following recipes will help:
- Take 2 tbsp. of cornflower flowers, pour 200 ml of boiling water, leave for an hour. After filtering, drink the remedy during the day, dividing it into three or four portions.
Homeopathy
Homeopathic preparations for detection of E. coli in a smear are prescribed in accordance with the painful symptoms. In the acute period (unless the doctor has prescribed otherwise), preparations are taken in dilutions of 30C, 6X, 12X, 6C, three to four times a day.
- Aconitum napellus - taken for rapid development of the inflammatory process, general anxiety, discomfort.
- Arsenicum album - taken for burning sensation and irritation of the mucous membrane.
- Belladonna - can be prescribed for right-sided pain, with fever and general deterioration of health.
- Ferrum phosphoricum is prescribed for unpleasant sensations in the genitals, against the background of general normal well-being.
- Hepar sulfuris is taken for general weakness and irritability against the background of all the signs of an inflammatory process.
Treatment with homeopathic medicines is safe and does not have any negative side effects. However, such medications should be taken with caution, periodically monitoring laboratory indicators of bacterial activity.
Prevention
Of course, it is much easier to prevent the appearance of E. coli in a smear than to try to get rid of the bacteria later. For prevention purposes, it is necessary to adhere to generally accepted hygiene rules. Such rules are expressed as follows:
- mandatory daily water procedures, washing, shower;
- mandatory daily change of underwear;
- regular hand washing with soap (especially before eating and after walking or using the toilet), if this is not possible, thoroughly wipe your hands with an antibacterial wet wipe;
- avoidance of using other people's underwear and personal hygiene items;
- use of barrier contraceptives during casual sexual intercourse.
The listed rules are not complicated and can be followed without problems. However, if any unpleasant symptoms from the urogenital system appear, self-medication should not be practiced. You need to see a doctor and undergo all necessary diagnostic tests. Early medical attention is the key to a quick and effective cure.
Forecast
With timely treatment of bacterial presence, the prognosis is positive in most cases. But only on condition of further compliance with all required rules for the prevention of infectious diseases. If E. coli in the smear was found in insignificant quantities, without any pathological symptoms, then prescribing prophylactic antibiotics is more than inappropriate. It is enough to undergo regular check-ups with a doctor, lead a healthy lifestyle, eat healthy and high-quality food. The practice of self-medication significantly worsens the prognosis of the disease.

