
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Intestinal diverticulosis
Medical expert of the article
Last reviewed: 12.07.2025
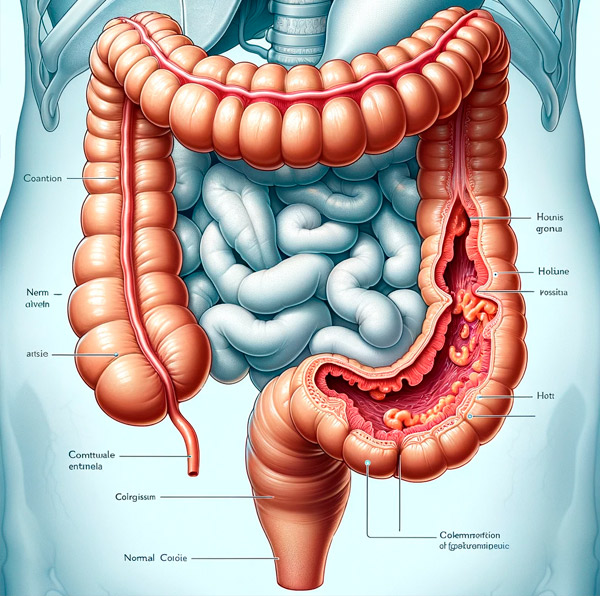
Diverticulosis is a clinical condition in which numerous sac-like protrusions (diverticula) develop throughout the digestive tract. Although diverticula can form at weak points in the walls of both the small and large intestines, most occur in the large intestine (most commonly in the sigmoid region).
Most people with diverticulosis are asymptomatic. Diverticulitis occurs when there is symptomatic diverticulosis (eg, bleeding from diverticula); diverticulitis (eg, acute or chronic inflammation that may be complicated by abscess and fistula formation,[ 1 ] bowel obstruction, or perforation); or associated segmental colitis (eg, inflammation in the segments of colonic mucosa between diverticula).[ 2 ],[ 3 ]

Meckel's diverticulum is a congenital protrusion in the terminal ileum, a remnant of the embryonic yolk-intestinal duct.
Epidemiology
The prevalence of diverticulosis is highest in the Western world. Diverticulosis affects between 5% and 45% of the population in the Western world. Overall, the prevalence of diverticulosis increases with age from less than 20% at age 40 to 60% at age 60. Approximately 95% of patients in the Western world with diverticulosis have diverticula in the sigmoid region. Of all patients with diverticulosis, 24% have diverticula primarily affecting the sigmoid region, 7% have diverticula uniformly distributed throughout the entire colon, and 4% have diverticula located only proximal to the sigmoid region.[ 4 ],[ 5 ]
In Asia, diverticulosis has a prevalence of approximately 13% to 25%. People with diverticulosis in this region also have predominantly right-sided colonic diverticula (in contrast to the Western world, where left-sided diverticula are much more common). Approximately 5% to 15% of patients with diverticulosis experience bleeding. One third of these experience profuse bleeding. In 50% to 60% of patients experiencing diverticulum bleeding, the source is from right-sided diverticula, possibly due to the thinner wall of the right-sided colon or the wider neck and dome of right-sided diverticula (eg, increased surface area for injury of the rectal vessels). [ 6 ]
Diverticulitis occurs in approximately 4% to 15% of patients with diverticula, and the incidence increases with age. On average, patients hospitalized with diverticulitis are approximately 63 years old. The overall incidence of diverticulitis continues to increase, jumping 26% from 1998 to 2005, with the largest increases seen in patients aged 18 to 44 years. Under age 50, diverticulosis is more common in men, while between ages 50 and 70, the disease is slightly more common in women. After age 70, the incidence of diverticulosis is significantly higher in women. [ 7 ]
Causes intestinal diverticulosis
Diverticulosis is thought to occur due to peristaltic disorders (eg, intestinal spasms), intestinal dyskinesia, or high segmental intraluminal pressure. Although the exact cause is unknown, several environmental and lifestyle risk factors have been associated with this condition.[ 8 ] Several studies have shown that a diet low in fiber and rich in red meat may be associated with an increased risk of diverticulosis,[ 9 ] although a diet high in fiber does not reduce symptoms of uncomplicated diverticular disease. In patients with symptomatic complicated diverticular disease (eg, inflammation or bleeding), a diet high in fiber may be beneficial as it reduces overall inflammation and favorably alters the gut microbiota.
The risk of diverticulitis and bleeding is significantly higher in patients who are obese or have a large waist circumference. Smokers have been noted to have an increased incidence of diverticular abscesses or perforations. Drugs associated with an increased risk of diverticulitis or bleeding include nonsteroidal anti-inflammatory drugs, opioids, and steroids.
Pathogenesis
Diverticula occur at weak points in the colonial wall where the vasa recta penetrate the muscularis annularis. The vast majority of colonic diverticula are usually "false" diverticula, which are mucosa and submucosa protruding through a defect or weakness in the muscularis, covered externally only by serosa. True diverticula are much less common (eg, Meckel's diverticulum) and involve protrusion of all layers of the intestinal wall (eg, mucosa, muscularis, and serosa).[ 10 ]
The main predisposing factor for the formation of colonic diverticula is abnormal colonic motility (eg, intestinal spasms or dyskinesia), resulting in increased segmental muscle contractions, increased intraluminal pressures, and division of the intestinal lumen into separate chambers. Because the sigmoid region of the colon has the smallest diameter, it is also the segment with the highest intraluminal pressures. Tissue disorders of ligaments, such as Marfan syndrome, Ehlers-Danlos syndrome, or hereditary polycystic kidney disease, may also predispose to the formation of colonic diverticula, as these diseases often involve structural changes (eg, weakness) in the intestinal wall.
Diverticula are prone to bleeding due to the proximity of the vasa recta to the intestinal lumen due to the mucosa and submucosa protruding through the muscularis propria. With the formation of diverticula, the vasa recta are separated from the intestinal lumen only by the mucosal layer and are at greater risk of injury. This results in eccentric intimal thickening, medial liquefaction, and ultimately segmental weaknesses along these arteries, predisposing the vasa recta to rupture and bleeding into the intestinal lumen. Diverticular bleeding usually occurs in the absence of inflammation or infection of the diverticula (i.e., diverticulitis).
Diverticulitis usually results from microscopic or macroscopic perforation of a diverticulum, which may or may not be due to obstruction (eg, faecalitis). Increased intracolonic pressures or insipidated (thickened and compacted) food material, with subsequent inflammation and focal necrosis, eventually lead to perforation of the diverticulum. The associated inflammation is usually mild, and pericolic fat and omentum tend to separate the diverticulum perforations. This may or may not lead to abscess or fistula formation, or to bowel obstruction. Rarely, perforations may be large and unconfined and lead to peritonitis.
Histopathology. The mucosa of the diverticulum and surrounding colonic area exhibit changes at the histologic and tissue levels. The mucosa of the diverticulum undergoes expansion of the lamina propria due to accumulation of lymphoplasmacytic infiltrates. Histologic changes also include mucus depletion, development of lymphoglandular complexes, and focal Paneth cell metaplasia. Acute inflammation manifests itself in the form of cryptitis and crypt abscesses. Bleeding may be seen in the diverticula and surrounding tissue. In the area of the mucosa surrounding the diverticulum openings, we see additional changes including pseudohypertrophy of the orbicularis muscle leading to increased mucosal folds and muscularization of the lamina propria, glandular hyperplasia, and hemosiderin deposits that are visible in the submucosa. These features are usually indistinguishable from those of inflammatory bowel disease.
Symptoms intestinal diverticulosis
Most people with diverticulosis have no symptoms, and the condition itself is not dangerous. However, some patients may experience unexplained abdominal pain or cramping, changes in bowel function, or blood in the stool. Any bleeding associated with diverticulosis is asymptomatic. Diverticulosis is suspected if a patient has a history of unprecedented rectal bleeding or unexplained abdominal pain or cramping, or changes in bowel function.
Acute diverticulitis (eg, inflammation, infection, or perforation) is usually suspected when a patient presents with lower abdominal pain (especially on the left side). Patients may also present with abdominal tenderness and an elevated white blood cell count (leukocytosis). A CT scan of the abdomen will help differentiate complicated from uncomplicated conditions in this setting.
Forms
Classification of intestinal diverticula
- Congenital (eg, Meckel's diverticulum) and acquired diverticula.
- True and false diverticula.
- By localization: diverticula of the small intestine; diverticula of the large intestine.
Complications and consequences
- acute (chronic) diverticulitis occurs as a result of microperforation of the diverticulum wall and the addition of an infectious process, and develops in 10-25% of patients with diverticular disease;
- peridiverticulitis - a localized inflammatory process, an intermediate stage between diverticulitis and abscess formation; [ 11 ]
- abscess (intramural microabscess is possible); intestinal stenosis and intestinal obstruction (the adhesion process around the diverticulum, unlike other complications, develops gradually);
- perforation of the diverticulum with the development of peritonitis; intestinal bleeding; fistulas; bacterial overgrowth syndrome.
Diagnostics intestinal diverticulosis
Diverticulosis is suspected based on clinical presentation (eg, history of rectal bleeding or unexplained abdominal pain and cramps, changes in bowel function) and can be confirmed by colonoscopy [ 12 ] or X-ray after barium enema. [ 13 ] However, if the patient has severe abdominal pain, abdominal CT is preferred to avoid the risk of bowel perforation in the setting of bowel infection or inflammation.
Colonoscopy in a prepared bowel remains the best investigation to identify the source of bleeding when blood is present in the stool. If colonoscopy is inconclusive, as in cases of acute or severe blood loss, angiography, CTA, or radionuclide scanning may be considered to identify the source.[ 14 ]
Patients with acute diverticulitis may require additional treatment. Uncomplicated diverticulitis is treated conservatively with intravenous or oral antibiotics. Complicated diverticulitis (eg, with associated fistula, abscess, obstruction, or perforation) may require hospitalization and/or surgery to treat complications in addition to antibiotic therapy. Similarly, patients with sepsis, immunosuppression, advanced age, significant comorbidities, high fever (greater than 103.5 °F [39.2 °C]), significant leukocytosis, inability to tolerate oral intake, noncompliance, or failure of outpatient treatment may require hospitalization for appropriate management.[ 15 ]
What do need to examine?
What tests are needed?
Differential diagnosis
Diverticulosis presents with bleeding from the rectum, and most of the time this is the only symptom. Differential diagnosis includes:
- Haemorrhoids.
- Ulcers in the intestinal wall.
- Inflammatory bowel disease.
- Anal fissure.
- Anal abscess or fistula.
- Colonic polyps.
- Colon cancer.
- Constipation.
- Radiation therapy.
- Angiodysplasia.
- Colitis.
- Proctitis.
Who to contact?
Treatment intestinal diverticulosis
Treatment is usually aimed at reducing intestinal spasms, which can be achieved by increasing dietary fiber and fluid intake. Large intestinal bulk reduces the amount of spasms and therefore reduces intestinal pressure. Studies have shown no positive or negative associations between diverticular disease and the consumption of nuts, grains, potassium, β-carotene, vitamin C, and magnesium. The evidence regarding the association between diverticular disease and alcohol and red meat consumption is controversial. Most bleeding associated with diverticulosis is self-limited and does not require intervention. However, in some cases, endoscopic, radiologic, or surgical intervention may be required to stop persistent bleeding (eg, injection, coagulation (cauterization, argon plasma coagulation), or mechanical devices (clamps, bands, slings)). If the source cannot be identified in cases of recurrent bleeding, surgery to remove portions of the diseased bowel (eg, coectomy) may be considered. Similarly, in the case of a giant diverticulum, with an increased risk of infection and rupture, surgical intervention is more likely.[ 16 ],[ 17 ]
Prevention
Diverticulosis of the intestine can be prevented by taking preventive measures against constipation: sufficient dietary fiber, therapeutic exercise, massage.
Forecast
Intestinal diverticulosis has a favorable prognosis in most cases, but in some situations it can lead to the development of severe and life-threatening complications. This can be explained not only by the severity of the complications themselves, but also by the predominant lesion of elderly people, who often already have concomitant diseases.
Acute diverticulitis occurs in 10-25% of patients with diverticular disease. The success rate of conservative therapy for acute diverticulitis is 70% for the first episode and only 6% for the third episode.
On average, 20-30% of patients with diverticular disease complicated by bleeding experience recurrent bleeding after several months or years. Preventive symptomatic treatment of uncomplicated disease with increased intake of dietary fiber in some cases (5-10%) reduces the incidence of complications and improves the course of the disease.

