
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Congestive prostatitis
Medical expert of the article
Last reviewed: 12.07.2025
For various reasons, pathological processes can occur in the prostate gland, including inflammatory ones, and one of the clinical types most common in men under 50 years of age is congestive prostatitis.
Epidemiology
In the absence of general epidemiological information on chronic nonbacterial prostatitis and chronic pelvic pain syndrome, experts – based on clinical statistics over the past decade – state that chronic congestive prostatitis affects men of all ages, but is most common in men aged 35–50 years (affecting 9–16% of men of all ethnic groups), and accounts for 80–90% of all cases of chronic prostatitis.
It is estimated that 5 million new cases of prostatitis are diagnosed annually with a prevalence of 2.2–9.7% worldwide, with chronic nonbacterial prostatitis accounting for 5.4% of cases.
According to foreign urologists, in general, some symptoms similar to prostatitis are experienced by about 10-14% of men from time to time. [ 1 ]
Causes congestive prostatitis
The development of a special form of pathological reaction in the form of congestive prostatitis, defined in modern terminology as non-bacterial chronic prostatitis, prostatodynia, prostatosis or non-inflammatory chronic pelvic pain syndrome (according to the classification of the American National Institute of Health, prostatitis type III B), is not associated with damage to the gland by pathogenic microorganisms, that is, an invasive infectious agent is absent. Thus, there is no formulation of the diagnosis - congestive bacterial prostatitis, despite the possibility of infection during the progression of congestive processes. [ 2 ]
For more information on the classification of chronic prostatitis and its variants, read the publication – Prostatitis: types
Although the exact etiology of this disease has not yet been established, experts believe that the causes of congestive prostatitis (in Latin, congestio means “accumulation”) are problems with blood circulation in the prostate – disturbances in regional venous hemodynamics, as well as stagnation of secretions produced by the prostate, which leads to edema and prostatosis syndrome.
There is a causal relationship between this type of prostatitis and tissue irritation and disruption of the integrity of the urothelium caused by the accumulation of urine entering the prostate gland as a result of urethroprostatic reflux; with insufficient testosterone levels (androgen deficiency) or defects in its receptors; with dystrophic or diffuse changes in the parenchyma of the prostate gland; with a previously existing bacterial infection that is not detected in the relevant tests at the time of the patient's visit; with inflammation of the nerve endings of the prostate.
Risk factors
Among the factors predisposing to circulatory disorders and secretory congestion in the prostate gland, the following are noted:
- lack of physical activity and sedentary work;
- frequent hypothermia;
- sexual abstinence and lack of regular sex;
- incomplete emptying of the gland during ejaculation;
- interruption of sexual intercourse;
- frequent long-term sexual contacts, masturbation;
- the presence of a cyst or stones in the gland (with the development of pathological changes in the parenchyma);
- dilation of veins in the pelvic organs, accompanied by venous congestion;
- intestinal problems (tendency to constipation, inflammation of the colon, etc.);
- cystic formations of the urinary tract and impaired blood supply to the lower urinary tract;
- abdominal obesity and insulin resistance;
- immune system disorders;
- high stress levels.
Prostate congestion can be caused by excessive consumption of caffeine (which increases urination), spicy foods (which increase urine acidity) and, of course, alcohol, which can cause vascular ectasia (persistent dilation of blood vessels) of the prostate gland with subsequent ischemia and deterioration of its tissue trophism.
Pathogenesis
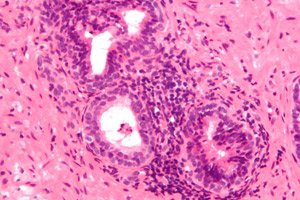
Today, the pathogenesis of chronic congestive prostatitis/nonbacterial chronic prostatitis is explained by compression of the excretory ducts, acini and prostatic part of the urethra due to enlargement of the prostate gland and swelling of its parenchyma with stagnation of blood or accumulation of secretion.
Several pathophysiological and biochemical mechanisms may be combined in the development of pain syndrome accompanying non-infectious chronic congestive prostatitis. Thus, researchers have identified the involvement of the autoimmune response to prostate gland antigens (PAg) in the inflammatory process, which results in an increase in the level of inflammation mediators (proinflammatory cytokines) and immunocompetent prostate cells (Th1 helpers, B-lymphocytes, mastocytes), which promote the activation of cellular immunity; increased oxidative stress, which damages prostate tissue and sperm proteins; increased secretion of neurotrophin, which stimulates neurons and causes nervous sensitization, which probably causes chronic pelvic pain. [ 3 ]
Symptoms congestive prostatitis
Symptoms of chronic congestive or congestive prostatitis may concern the urethra, genitals and their functions, rectum and general condition. This is urological pain or discomfort in the pelvic area associated with urination and/or sexual dysfunction.
And the first signs in most patients are difficulty urinating and a feeling of incomplete emptying of the bladder, as well as pain during urination and pressure in the perianal area. [ 4 ]
The list of the most characteristic symptoms also includes:
- frequent urination (pollakiuria), including at night;
- imperative (unbearable) urge to urinate;
- constant or periodic dull and aching pain - in the perineum and groin, in the lower abdomen, in the penis and scrotum, in the rectum, in the coccyx area and lower back;
- sexual dysfunction (lack of erection); [ 5 ]
- decreased libido, premature ejaculation, pain or burning during ejaculation, partial anorgasmia;
- hemospermia (blood in semen).
Periodically slightly elevated temperature with congestive prostatitis; general weakness and sleep disturbance; chronic fatigue syndrome; depression and anxiety disorders are not excluded.
In case of stagnation and the presence of prostate stones (which can block the gland ducts), congestive prostatitis with calcifications is determined. It also manifests itself as painful urination, discomfort in the perineum and penis, aching pain in the prostate during defecation and ejaculation.
See also - Symptoms of Chronic Prostatitis
Complications and consequences
Chronic congestion in the prostate not only causes genitourinary problems, but can have significant consequences and complications both for its morphology and functions, and for male fertility (causing infertility).
It is possible to develop intrapelvic venous congestion syndrome, dystrophy and neuromuscular pathology (atony) of the prostate gland, ischemia or sclerotic changes in tissues, formation of parenchymal cysts or diverticula.
According to oncologists, chronic prostatitis is closely associated with the development of prostate adenocarcinoma and colorectal cancer. [ 6 ]
Diagnostics congestive prostatitis
Diagnosis of congestive prostatitis/non-bacterial chronic prostatitis/prostatosis begins with obtaining anamnesis, recording the patient's complaints and characteristics of his sexual life, physical examination of the genitals and digital rectal examination of the prostate gland.
The following tests are performed: general and biochemical blood tests; tests for STDs; PSA test – the level of prostate-specific antigen in the blood; testosterone levels in the blood serum; urine analysis (including bacterial culture); microscopic analysis and bacterial culture of prostate secretion; ejaculate analysis. [ 7 ]
Instrumental diagnostics include: transrectal ultrasound examination (TRUS) of the prostate gland; Doppler sonography of the pelvic organs and ultrasound Doppler sonography of the prostate gland vessels; ultrasound of the bladder and cystotonometry; retrograde urethrography and uroflowmetry; electromyography of the pelvic floor muscles. In complex cases, endocystoscopy, CT or MRI of the bladder, urinary tract, prostate and pelvic organs are used.
For more details see – Diagnosis of chronic prostatitis
Differential diagnosis
Differential diagnostics is designed to exclude other pathologies that cause similar symptoms: chronic cystitis, urethritis, neurogenic dysfunction of the bladder, stenosis of the bladder neck, strictures of the urethra, prostatic hypertrophy, inflammation of the seminal follicle (colliculitis), etc. In addition, in the absence of bacteriuria and pathogenic microflora in the prostatic secretion, symptoms similar to those of prostatitis are possible due to myalgia of tension of the pelvic floor muscles - myofascial pelvic syndrome.
Who to contact?
Treatment congestive prostatitis
In the symptomatic treatment of congestive prostatitis – urogenital pain in the absence of uropathogenic bacteria – drugs of various pharmacological groups are used. Thus, to normalize urination and reduce its pain, drugs of the group of α-adrenergic receptor antagonists (alpha-blockers) are prescribed, which reduce the tone of the smooth muscles of the prostate gland, bladder neck and prostatic part of the urethra: Adenorm (other trade names – Tamsulosin, Bazetam, Omix, Omnix, Ranoprost, Tamsonic, Urofri), Alfuzosin (Dalfaz, Dalfusin), Prazosin, Terazosin (Alfater, Cornam), Phentolamine hydrochloride (Alfinal), Doxazosin. These drugs are contraindicated in case of low blood pressure and liver failure. Their side effects include nausea, vomiting, constipation, diarrhea, dizziness, headache, tachycardia, visual impairment, rhinitis, urticaria, etc. The dosage is determined by the attending physician. [ 8 ]
For the same purpose, anticholinergic agents (muscle relaxants) Tolperisone (Tolisor, Mydocalm), Baclofen, Fesoterodine can be used. Their use, in addition to nausea and vomiting, can cause headaches, muscle weakness, and a hypotensive effect in patients.
To reduce dysuric symptoms in congestive prostatitis with calcifications and prostate enlargement, medications that suppress the activity of the enzyme 5-α-reductase may be prescribed: Finasteride (Prosteride) or Avodart (Dutasteride) - one capsule per day. [ 9 ]
Can Ibuprofen be taken for congestive prostatitis? This non-steroidal anti-inflammatory drug with analgesic action - due to the potential side effects of drugs in this group (irritation and ulceration of the stomach walls) - can be used occasionally: for intense pain. For a detailed description of contraindications for this drug and other side effects, see - Ibuprofen.
Tricyclic antidepressants (in minimal dosage) can relieve discomfort or pain; antispasmodics (No-shpa, Bencyclane or Galidor) help relieve pain and normalize blood flow in the prostate vessels.
Pumpkin seed oil or Tykveol capsules (Garbeol, Granufink Uno) reduce swelling, stimulate metabolism and promote normal hemodynamics in the prostate.
More useful information in the material – Pathogenetic treatment of chronic prostatitis.
In the complex therapy of congestive prostatitis, physiotherapy is also used, aimed at improving blood circulation in the prostate gland and trophism of its tissues. Details in the publications:
- Physiotherapy for prostatitis
- Treatment of chronic prostatitis: microwave ultra-high frequency therapy
- Treatment of chronic prostatitis: magnetic therapy
- Laser therapy in the treatment of chronic prostatitis
- Prostate massage
The effectiveness of hyperbaric oxygenation in the treatment of patients with chronic congestive prostatitis has been proven. [ 10 ]
Traditional medicine recommends taking aloe juice internally (or eating fresh leaves of the plant), onion juice diluted in half with water, and eating raw pumpkin seeds.
Some patients find that herbal and other medicinal plants help reduce the intensity of symptoms of congestive prostatitis. For example, herbalists recommend treatment with an aqueous extract of bearberry (Arctostaphylos uva-ursi) and wintergreen (Pyrola umbellate) leaves; a decoction or extract of nettle roots and leaves; an infusion of plantain seeds (Plantago major) and white mustard (Sinapis alba); an infusion of galangal root (Alpínia officinarum), a decoction of the above-ground parts of carnation (Dianthus superbus), knotweed (Polygonum aviculare), and fireweed (Epilobium).
In addition, herbal therapy for dysuric symptoms may be recommended using an extract of saw palmetto or saw palmetto (Serenoa repens or Sabal serrulata), which is contained in capsules Prostamol Uno, Prostaplant, Palprostes, etc.
Used in therapy and homeopathy:
- drops Berberis-Homaccord, Populus compositum SR, Sabal-Homaccord, Gentos, Ursitab Edas-132;
- Bioline Prostate sublingual tablets with extracts of wintergreen (Chimaphila umbellate), straight clematis (Clematis erecta), common goldenrod (Solidago virgaurea) and saw palmetto fruits.
Surgical treatment by transurethral interventions – laser incision of the prostate gland or its resection – is carried out only when conservative therapy is ineffective. And prostatic stones are removed by lithotripsy (crushing stones with ultrasound, electromagnetic waves or laser).
Prevention
There is no surefire way to prevent this condition, but some lifestyle changes can help reduce your risk. Those who have sedentary jobs should take short breaks to stand up and walk around for a few minutes.
For general prevention of prostate problems, sports activities (except weightlifting and cycling), simple physical activity (except lifting weights) and regular sex are useful.
It is important to control your weight, drink enough water, follow healthy eating habits, and stay away from alcohol, caffeine, and spicy foods.
Forecast
It is difficult to give a prognosis for a disease whose exact etiology is still unclear, but doctors are confident that congestive or stagnant prostatitis does not pose a threat to life. However, the quality of life due to chronic pelvic pain, which is difficult to treat, is significantly reduced, and patients have to fight it for months and even years.

