
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Chronic cystitis: causes, signs, prevention
Medical expert of the article
Last reviewed: 12.07.2025
If the infection of the bladder is constantly repeated, that is, relapses of its inflammation are periodically observed, chronic cystitis can be diagnosed, which has the ICD-10 code N30.1-N30.2.
Urologists believe that if inflammation of the bladder occurs either at least three times during the year, or twice in six months, then the patient most likely has chronic recurrent cystitis.
Epidemiology
According to WHO, almost 150 million people experience bladder and urinary tract infections each year. For example, in the US, approximately 8-10 million people visit urologists each year.
As clinical statistics show, chronic forms of cystitis are more often diagnosed in women aged 30-50 years, but women in the post-menopausal period are most susceptible to this disease - up to 5% (among women in North America - up to 20%).
According to experts from the International Urogynecological Association, half of all women experience symptoms of bladder inflammation, and 20-30% experience relapses, that is, repeated infection.
Among older European men, chronic prostatitis and cystitis occurs in almost a quarter of urological patients.
Chronic cystitis in children most often occurs before the age of two; in boys and young men, this pathology is diagnosed in rare cases. Read more in the material - Chronic cystitis in children
Causes chronic cystitis
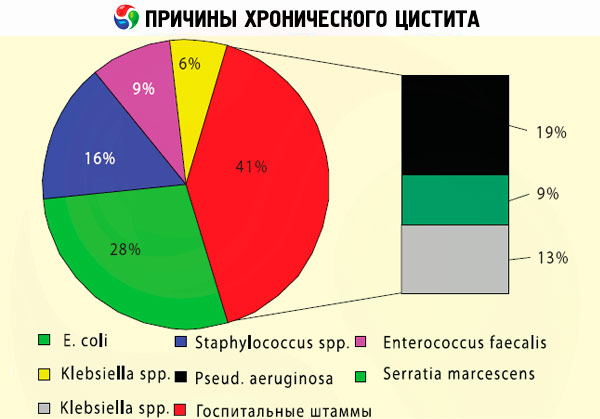
The predominant causes of chronic cystitis are infectious. For example, when Escherichia coli (E. coli) that live in the colon enter the urethra and migrate to the bladder, they begin to multiply there and cause inflammation. In addition, chronic bacterial cystitis can result from persistent infection, including Enterobacter (E. cloacae and E. agglomerans), Proteus mirabilis, Klebsiella sp., Pseudomonas aeruginosa, Chlamydia trachomatis, Streptococcus faecalis, Staphylococcus saprophyticus.
Due to the shorter urethra, chronic cystitis is much more common in women than in the male population. Often, chronic inflammation of the bladder in women is combined with bacterial vaginosis. Cystitis is also possible against the background of chronic ureaplasmosis - damage to the urethra, mucous membranes of the cervix or vagina by the bacteria Ureaplasma urealyticum and Ureaplasma parvum. It is significant that in all cases there is a decrease in the level of intravaginal acidity, which facilitates the activation of microorganisms. And physiologically conditioned immunosuppression (suppressing the rejection of the embryo) explains why chronic cystitis and pregnancy are associated. This topic is dedicated to a separate publication - Cystitis during pregnancy
One of the causes of chronic cystitis in women, localized in the area of the bladder neck, may be a violation of the trophism of its mucous tissues due to poor blood supply associated with a change in the position of the vagina and/or uterus after childbirth or with gynecological pathologies.
The infection can be descending: during inflammatory processes in the kidneys, it enters the bladder cavity with urine, which provokes the simultaneous course of such urological diseases as chronic cystitis and pyelonephritis.
Repeated bladder infections – chronic cystitis in men – are detected ten times less frequently than in women. Among the causes of this pathology, the leading ones are sexually transmitted infections, especially chlamydia, as well as benign enlargement of the prostate gland or its inflammation – prostatitis. Chronic prostatitis and cystitis usually appear in men after 50 years of age. In addition, infections often develop first in the urethra (which can be the result of frequent installation of catheters), and then affect the bladder, so chronic urethritis and cystitis are related by a common pathogenesis. In any case, stagnation of urine in prostatitis or urethritis creates conditions for chronic inflammation of the bladder in men.
Chronic hemorrhagic cystitis is induced by radiation or chemotherapy for pelvic cancer, but may be a consequence of urolithiasis or activation of polyomavirus (BKV and JCV).
Risk factors
Urologists consider the following to be risk factors for the development of chronic inflammation of the bladder:
- weakened immunity;
- long-term treatment with antibacterial drugs that suppress the protective obligate intestinal microbiota;
- chronic inflammation of the kidneys (pyelitis, pyelonephritis);
- gynecological diseases (vaginal and cervical inflammatory processes);
- changes in hormone levels in women due to pregnancy and menopause;
- chronic form of prostatitis, prostate adenoma in men;
- bladder or kidney stones;
- the presence of congenital anomalies of the urinary tract or bladder that prevent it from being completely emptied;
- metabolic diseases such as diabetes or uric acid diathesis;
- scars and diverticula in the bladder;
- any urological manipulations and surgical interventions (including the installation of cystostomy drainage);
- history of autoimmune diseases;
- bladder tumors.

Patients undergoing immunosuppressant therapy are at risk of hemorrhagic cystitis due to direct exposure to cytotoxic anticancer drugs or activation of persistent infection in urinary tract organs, including the bladder.
It is also known that attacks of chronic cystitis can occur with prolonged hypothermia of the body and frequent sexual intercourse.
Pathogenesis
The pathogenesis of inflammation in the bladder affected by E. coli that has penetrated its cavity is explained by the fact that this bacterium can bind to glycolipids of the cell membrane and penetrate into the urothelial cells. Due to the proliferation of the microorganism, accompanied by the release of toxins, protein synthesis ceases, which leads to the destruction of the cells of the mucous membrane of the bladder and the development of an inflammatory reaction.
The pathogenesis of ureaplasma-associated cystitis has also been well studied. Without causing symptoms, these bacteria live extracellularly in the urogenital tract of sexually active women and men and rarely penetrate cells, except in cases of immunosuppression. When the immune system is weakened, U. urealyticum damages the cells of the mucous epithelium, causing their morphological changes and increased activity of proinflammatory cytokines, leukocytes and prostaglandins, as well as expression of tumor necrosis factor (TNF-α).

Hypotheses regarding the etiology and pathogenesis of rare encrusting chronic cystitis are controversial, but the most popular of them suggest the involvement of the gram-positive bacillus Corynebacterium urealyticum. This commensal skin bacterium with strong urease activity breaks down urea, creating an alkaline environment in the bladder that is favorable for the deposition of inorganic salts (struvite crystals and calcium phosphate) on its mucosa.
The role of decreased estrogen production in the pathophysiology of urinary tract infections and chronic cystitis in older women has been determined. The female sex hormone stimulates the proliferation of Lactobacillus cells in the vaginal epithelium, and lactobacilli reduce pH and prevent microbial colonization of the vagina. In addition, in the absence of estrogen, the volume of vaginal muscles and the elasticity of the ligaments supporting the fundus of the uterus decrease, and prolapse of the internal genital organs causes compression of the bladder and stagnation of urine.
Symptoms chronic cystitis
According to urologists, how often or how severe the symptoms of chronic cystitis are depends on a number of factors. But the first signs in 80% of cases are associated with increased frequency of urination (pollakiuria) and small volumes of urine excreted with each urination.
As a rule, the course of chronic cystitis occurs in several stages, but some types of this disease occur continuously.
The infection usually presents with a gradual onset of inflammation that worsens over months, with one or more symptoms including:
- discomfort in the bladder;
- imperative urge to urinate (both day and night);
- pain and burning when urinating;
- bladder spasms;
- fever.
According to clinical observations, 60% of patients in the acute stage have nagging pains with chronic cystitis, felt in the lower abdomen (above the pubic bone), in the perineum and pelvis, in women - also in the area of the uterus and appendages. Another symptom is dyspareunia, that is, sex with chronic cystitis can be painful for women.
A sharp cold snap, as well as the season from late autumn to early spring, is the main time when chronic cystitis can become aggravated. Moreover, as it turned out, chronic bacterial cystitis in 90% of cases becomes aggravated due to a new infection that occurs after a break of more than two weeks after the previous inflammation.
After the remission stage, when the intensity of symptoms significantly decreases, there are asymptomatic periods, perceived as remission of chronic cystitis, after which a relapse occurs again after some time.
Most patients with chronic cystitis have cloudy urine, and tests show significant bacteriuria. Some may have pus in their urine or blood in it ( hematuria ).
Forms
First of all, a distinction is made between chronic bacterial cystitis and the much rarer non-bacterial cystitis.
When defining chronic latent cystitis, that is, not manifesting itself with obvious symptoms, they mean hidden, that is, latent periods, which characterize the course of chronic cystitis in many patients.
If there is blood in the urine, chronic hemorrhagic cystitis is diagnosed. In cases where the inflammatory process is localized in the neck of the bladder (cervix vesicae) - the area of its narrowing and transition to the urethra - chronic cervical cystitis of the bladder in women and men is diagnosed.
Depending on the morphological features of the damage to the tissues of the inner lining of the bladder, revealed during cystoscopy, the following types of this disease are distinguished:
- chronic catarrhal cystitis (superficial, affecting the upper layers of the mucous epithelium; accompanied by exudation).
- Chronic follicular cystitis is a rare non-specific inflammation of the bladder of uncertain etiology; it is characterized by the presence of lymphoid follicular tissue infiltrates in its mucous membrane. Usually, pathological changes with edema and hyperemia are localized in the basement membrane of the trigonal zone (vesical triangle) or at the base of the bladder.
- Chronic cystic cystitis is a rare form of the disease with formations (the so-called Brunn's nests) that grow into the basement membrane (lamina propria) of the bladder mucosa and in the urothelium of the bladder wall are transformed into cystic cavities (often with liquid contents).
- Chronic polypous cystitis also refers to rare forms of non-specific mucosal reaction with polypous lesions and edema. In 75% of cases, it is detected in men with frequent catheterization of the bladder.
- Chronic bullous cystitis is a reversible inflammation with extensive submucous edema of the bladder, simulating tumor formations. A variant of polypous cystitis, but with larger lesions. It may be asymptomatic, but acute attacks of chronic cystitis are also possible.
- Chronic granular cystitis is a diffuse inflammation of the bladder mucosa with multiple small focal infiltrates in the form of granules.

Some experts distinguish chronic glandular cystitis, which affects the lamina propria with formations of columnar epithelial cells, as well as chronic glandular cystitis (also called intestinal metaplasia), which has the appearance of papillary formations of cells similar to intestinal epithelium and is localized in the area of the bladder neck and trigonal zone.
In clinical urology, chronic interstitial cystitis or painful bladder syndrome is distinguished. Its etiology, pathogenesis, symptoms and treatment methods are discussed in the publication – Interstitial Cystitis.
 [ 22 ]
[ 22 ]
Complications and consequences
A chronic disease, including a urological one, always has certain consequences and complications.
What is the danger of chronic cystitis? Damage to the deep layers of the bladder wall and its deformation, leading to a decrease in bladder capacity and its partial dysfunction. As a result, problems with urine excretion appear - up to enuresis.
The infection can spread to the pelvic organs; in women, this can lead to menstrual irregularities and inflammation of the reproductive organs, so they often ask whether it is possible to get pregnant with chronic cystitis. Indeed, problems can arise if the inflammatory process affects the appendages and/or uterus.
In addition, possible complications of chronic cystitis include reverse urine flow (vesicoureteral reflux), pyelitis, and pyelonephritis.
The risk of obstruction of the ureteral orifice by a blood clot in chronic hemorrhagic cystitis (with rupture of the bladder) or the urethra in chronic bullous cystitis (when the inflammatory focus is located in the trigonal or periurethral zones of the bladder) cannot be ruled out.
Patients with chronic polyposis cystitis have an increased risk of developing bladder tumors (urothelial carcinoma).
Diagnostics chronic cystitis
For laboratory research the following tests are submitted:
- general blood test;
- blood test for STDs;
- general urine analysis;
- urine tests for leukocytes, erythrocytes, and protein;
- urine culture for bacteria.
Instrumental diagnostics are carried out:
- contrast cystography (x-ray of the bladder);
- visualization of the bladder and urinary tract by ultrasound scanning; chronic cystitis on ultrasound - for details see Ultrasound of the bladder
- micturition cystourethrography (X-ray examination during urination);
- cystoscopy with biopsy (endoscopic examination is performed exclusively during the remission stage of the disease).
Differential diagnosis
Only differential diagnostics can exclude all pathologies in which urination disorders are observed. For example, overactive bladder, chronic prostatitis, urethritis or pelvic pain in endometriosis are erroneously diagnosed as bladder infection.
Chronic recurrent cystitis may also be a sign of bladder cancer, especially in older patients with hematuria and urinary tract infection (hence the need for biopsy).
Treatment chronic cystitis
Read about effective treatment regimens for chronic cystitis in this article.
Prevention
Preventing a bladder infection is not always possible. What can you do to minimize the risk? Urologists advise:
- drink more water;
- maintain hygiene (general and intimate);
- do not wear tight underwear;
- increase the amount of vegetables and fruits in the diet. This will give the body more vitamins that boost immunity, and the intestines more fiber that promotes the work of beneficial lactobacilli, which suppress the growth of pathogenic microorganisms;
- do at least 10 minutes of exercise every day;
- Do not smoke or abuse alcohol.

