
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Cervical metaplasia
Medical expert of the article
Last reviewed: 12.07.2025
Cervical metaplasia is one of the precancerous diseases that has serious consequences if left untreated or with incorrect diagnostic and treatment tactics. This pathology is common in women over 50, although it can occur earlier. But not all women have an idea of what is at stake if this diagnosis is made. Since cervical metaplasia tends to become 100% malignant in the future when diagnosed late, it is better to prevent this pathology at the stage of initial changes. For this purpose, all women undergo a screening examination for metaplasia during their routine gynecological examination.
Causes cervical metaplasia
When talking about the development of cervical dysplasia, it is very important to highlight the main risk factors and etiological causes of the development of this process.
Among the etiological factors, that is, the probable causes of the development of pathology, infectious agents are in the first place. Among the possible pathogens, there may be both viruses and bacteria. Among the viral agents, this is most often a woman's infection with the human papilloma virus. This virus has a tropism for female genital organs and causes the development of another disease - condylomas or papillomas of the cervix. But the infection may not make itself known for a long time, and its course may be asymptomatic, and in some cases, cervical dysplasia may develop. Other possible agents are herpes viruses of all types. These viruses also have a tropism for the epithelium of the cervix and a fairly high oncogenicity, so they can be a trigger for the development of dysplastic processes in the cell.
Bacteria play a lesser role in the development of this disease, since they do not penetrate the nuclear apparatus of the cell and do not induce changes in the genetic material. But among possible bacterial infections, only intracellular ones are of greater importance - these are ureaplasmas, toxoplasmas, chlamydia, gonococci. These microorganisms penetrate the cell and remain there for a very long time, while protecting themselves from immune cells and maintaining a chronic focus of inflammation. This is not the true cause of dysplasia, but against its background, similar changes can develop that will further lead to dysplasia.
It is quite difficult to establish the exact causes of cervical metaplasia, but today, one of the proven etiological factors is infection with the human papillomavirus, which plays a key role in the further progression of changes inside the cell.
Risk factors
Risk factors can be divided into general and local. General ones include bad habits, smoking, alcohol consumption, dietary disorders and consumption of carcinogenic products, and the influence of environmental factors. All these changes are accompanied primarily by a decrease in the reactivity of the entire organism, and against this background, functional and then morphological changes in organs and systems develop.
Among the risk factors for the development of cervical dysplasia are local ones - early onset of sexual activity, frequent change of sexual partners, as well as infectious and inflammatory diseases of the female genital organs, frequent surgical interventions - abortions, hormonal imbalances, traumatic injuries.
Pathogenesis
Speaking about the process of development of dysplastic processes, it is very difficult to single out the period when they develop and the duration of such changes. Since pathology can also occur in women under 40, it is important to be alert when suspecting metaplasia.
The structure of the cervix in a healthy woman is an alternation of epithelial cover:
- flat multilayered non-keratinizing epithelium - located in the endocervix closer to the vaginal canal and is a continuation of it;
- the intermediate zone is located further and is the border on the way to the cervix; both types of epithelium are absent here;
- Columnar epithelium – lines the cavity of the cervix and the cervical canal.
Normally, these balls do not mix and there is a clear boundary between them.
The pathogenesis of cervical metaplasia development begins with a trigger factor, which may be a viral agent. In this case, the virus penetrates the cell, where its nucleic acid enters the nucleus by violating the integrity of the nuclear membrane.
As a result, the genetic apparatus of a normal cell is disrupted and the virus initiates the synthesis of its own proteins, which are necessary for its vital functions. This disrupts the normal life cycle of an epithelial cell and its division and reproduction processes. This is how abnormal cell divisions are formed, which contributes to the appearance of epithelial cells with nuclear atypia. That is, the process of cell division can stop at a certain phase of mitosis, and then the development of numerical cells with an incorrect set of chromosomes can be initiated. Such cells cannot ensure normal protein synthesis and metabolism in the cytoplasm, which is the cause of dysplastic processes in the cell. Such cells multiply and can move from their main location - for example, the columnar epithelium goes beyond the intermediate zone and zones of columnar epithelium appear among the normal flat epithelium of the endocervix, which is the phenomenon of metaplasia. Such a disruption of the normal structure of the epithelial cover does not reach the basal membrane.
Today, the definition of metaplasia or dysplasia is outdated, and a new term is used - CIN - cervical intraepithelial neoplasia. This concept allows us to clarify that this process is not so much dysplastic as precancerous.
Symptoms cervical metaplasia
Considering that this pathology often occurs without symptoms, it is necessary to know the main symptoms that allow you to pay attention and suspect this problem.
Cervical metaplasia is a dangerous condition precisely because the morphological changes that develop often far outpace the development of even minimal clinical symptoms. This is one of the reasons for the introduction of mandatory screening for this pathology.
Symptoms of cervical metaplasia can manifest themselves most often with some provoking factor. This can be with concomitant condylomas, erosions, infectious lesions. Less often, the clinical picture occurs without such conditions and is characterized by pain during sexual intercourse, disruption of the normal menstrual cycle, if there are hormonal imbalances, vaginal discharge. Discharge can be in the form of leucorrhoea - cheesy, abundant, white or milky discharge with an unpleasant odor, as well as in the form of bloody discharge before menstruation, after it or after sexual intercourse. Local pain with metaplasia is not typical if it is a purely dysplastic process.
The first signs that appear most often and are not specific, but should alert - this is painful sexual intercourse. Unpleasant sensations arise due to trauma to the dysplastic epithelium, which can also be accompanied by bloody discharge. This does not happen very often, but can be one of the first manifestations. As for older women, the first symptoms of metaplasia can often not be expressed due to involutional processes in the uterus and cervix, which suggests premenopausal changes. So, the symptoms that appear in a woman, she explains by the onset of menopause and does not consult a doctor.
Considering that clinical symptoms are not sufficiently expressed, it is necessary to take any changes in health very seriously, especially in older women.
Where does it hurt?
Forms
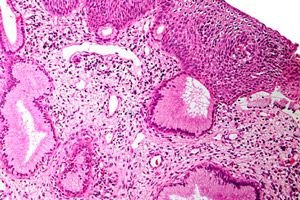
Since the cervical epithelium has several types of cells, metaplasia can also be different. The histological picture of changes in the smear is studied to establish the correct diagnosis and choose treatment tactics. In this case, not only the degree of spread of atypical cells is indicated, but also the nature of these changes and the morphological features of the smear.
There are several types of dysplasia:
- immature metaplasia of the cervix;
- squamous cell metaplasia of the cervix with dyskaryosis;
- squamous cell metaplasia of the cervix.
As for immature metaplasia, this is considered the most unfavorable option, since the lower the level of cell differentiation, the greater the risk of malignancy. The picture of immature dysplasia is characterized by the appearance in the smear of cells that are small in size, have unclear, unequal boundaries, and are also located chaotically in the smear itself. As for the internal structure of the cells, the cytoplasm is changed with a violation of the location and structure of the structural elements of the cell. Various changes in mitosis are observed in the nucleus. Sometimes it is difficult to attribute such cells to any type of epithelium, since they do not have characteristic distinctive features.
Squamous cell metaplasia of the cervix with dyskaryosis is a more differentiated type, compared to immature forms. Such cells already have a certain shape, the same size and sufficient size. Inside the cell, the cytoplasm is not changed, and the structural elements are located correctly, in sufficient quantity, which characterizes the cytoplasm of a normal epithelial cell. The only differences from normal cells are abnormal divisions in the nucleus in the form of pathological mitoses. This is what characterizes the term "dyskaryosis".
Squamous cell metaplasia of the cervix is the most differentiated variant, since the epithelium has all the characteristics of normal cells, except for the location. Thus, in squamous cell metaplasia of the cervix, the flat multilayered epithelium is determined beyond the intermediate zone in the cervical canal among the columnar epithelium.
These histological types do not affect the course of the disease, but have different prognosis, therefore such classification is mandatory in cytological examination.
Diagnostics cervical metaplasia
Since the course of this pathology is often asymptomatic, an important element of timely diagnosis and prevention of complications is preventive examinations by a gynecologist, which a woman should undergo annually. During the examination, the doctor examines the woman's cervix in mirrors, which makes it possible to see changes that can be seen without additional methods. Several cells of metaplastic epithelium among the normal cover are usually not visible, so a mandatory stage of the examination is taking a smear with a special brush for histological examination and detection of dysplasia.
The correct technology must be followed - a smear is taken from three zones of the cervix - the endocervix, the intermediate zone and the cervical canal, i.e. all three types of epithelium must be present. This is where the objective examination ends. Then all smears are sent to the laboratory for cytology and histology.
The tests that the doctor receives from the laboratory allow one to suspect dysplastic changes. There are six main types of smears:
- histological picture of a healthy woman;
- inflammatory and benign changes in the smear;
- cervical intraepithelial neoplasia
- mild metaplasia (CIN-I) – altered dysplastic cells extend into no more than one third of the epithelial layer;
- moderate metaplasia (CIN-II) - altered dysplastic cells extend in depth by no more than two-thirds;
- severe metaplasia (CIN-III) - altered dysplastic cells extend into the tissue by two-thirds or more, but without invasion of the basement membrane;
- suspected cancer;
- Cancer;
- uninformative smear (not all types of epithelium are represented).
If the smear comes back and the woman is healthy, everything is fine, but in all other cases, the woman is called in for a follow-up consultation and undergoes additional examination.
If metaplasia is suspected, that is, if the smear is of the third type, then instrumental research methods are carried out.
Colposcopy is a diagnostic test of the cervix using a special device that has a magnifying power of 2 to 32 times, depending on the power. This magnification allows you to see those areas of metaplasia that are not determined during a normal examination in mirrors. In addition to simple colposcopy, an extended one is also performed. In this case, the area of the examined epithelium of the cervix is stained with trichloroacetic acid, iodine or Lugol's solution, and the degree of staining is looked at. Areas of metaplastic epithelium will be pale against the background of normally stained epithelium. Such diagnostics allow you to confirm the presence of metaplasia, even if nothing can be detected visually.
In case of a doubtful diagnosis, a repeated histological examination is performed during colposcopy with targeted aspiration biopsy, and also possibly diagnostic curettage of the cavity and canal of the cervix.
These are the main research methods that allow us to establish a diagnosis.
How to examine?
What tests are needed?
Differential diagnosis
Since metaplasia is often asymptomatic, the main diagnostic is histological verification, which allows for an accurate diagnosis. But metaplasia should also be differentiated from other precancerous conditions and benign formations of the cervix: polyps or condylomas, erosions, leukoplakia without atypia, adenomatosis.
Cervical polyps or condylomas are benign neoplasms of viral etiology. The cause of cervical polyps, as in some cases metaplasia, is the human papilloma virus. This neoplasm is characterized, as well as metaplasia, by the proliferation and growth of cells. But with polyps, these formations are visible to the naked eye and rise above the surface of the epithelial cover. There are flat condylomas - similar to wart-type growths on the skin, and pointed condylomas on a stalk in the form of cauliflower.
Cervical erosions during colposcopy have a characteristic appearance - this is a defect of the mucous membrane. There are also pseudo-erosions, which occur in girls under 25 years old, as a result of hormonal imbalance. In any case, they are bright red, slightly swollen due to the inflammatory component.
Leukoplakia is the appearance of keratinized epithelium in areas where it should not be. This is a form of dysplasia, but in this case, it is not intraepithelial neoplasia. These areas look like whitish islands among the epithelial cover. Histological examination allows us to establish the presence of cellular atypia and accurately distinguish leukoplakia from neoplasia.
Considering all possible changes in the epithelium of the cervix, the morphological examination of the epithelial smear comes to the forefront for accurate diagnosis, which also allows for differential diagnosis with other precancerous diseases.
Who to contact?
Treatment cervical metaplasia
Treatment of cervical metaplasia is mandatory and should be carried out at the earliest possible stage and in a timely manner, since it is a precancerous disease and there is a high probability of malignancy. As for the treatment method, the choice depends on the degree of CIN and the type of smear. With the second type of smear, the woman undergoes etiological therapy, symptomatic anti-inflammatory therapy. With the third type of smear (CIN-I), when dysplastic cells occupy up to one third of the epithelial cover, treatment can be conservative with the use of medications and local drugs. In case of CIN-II, CIN-III or the fourth and fifth types of smear, treatment is only surgical, since conservative treatment increases the risk of malignancy.
Conservative treatment of cervical metaplasia involves complex treatment using various approaches.
The regimen for this disease is general, dietary recommendations are without special features, healthy nutrition is recommended. During the treatment period, it is necessary to abstain from sexual activity.
As for medications, to conduct etiological treatment it is necessary to identify the human papilloma virus, which is most often found in metaplasia, and to use antiviral drugs. Today, there are two main drugs that are used to influence the virus - "Genferon" and "Panovir". These drugs inhibit the activity of the virus by influencing the nucleic acid and disrupt the process of reproduction of viral particles.
If concomitant bacterial flora is detected in the smear, antibacterial therapy is mandatory. Preference is given to complex preparations that contain not only an antibiotic, but also a corticosteroid and an antifungal drug. Such complex preparations include Neotrizol and Terzhinan. Course doses are used with further additional research after the treatment.
Symptomatic anti-inflammatory therapy is also carried out in the form of vaginal anti-inflammatory suppositories.
The treatment complex also includes immunomodulatory drugs.
Surgical treatment of cervical epithelial dysplasia is performed at CIN-II and CIN-III. This tactic is due to the fact that conservative treatment at this stage is ineffective, and during this time malignancy is possible.
There are several methods of surgical treatment: laser vaporization, cone excision, scraping of the cervical canal, electrocoagulation.
Scraping of the cervical canal is the most “rough” method and can be used in cases where there are no technological possibilities for other treatment methods or there are concomitant conditions that require such a method.
Cone excision is the excision of the cervical epithelium in the form of a cone, depending on the depth of the lesion. This method has its advantages, since the risk that any cells will remain deeper is minimal, since the area is excised to the basement membrane or even deeper if necessary. But this method is more invasive and traumatic than others. After excision, the material is sent for histological examination and it is possible to exclude cell atypia once again.
Electrocoagulation is the use of an electrical charge to create high temperatures that can coagulate protein and thus destroy dysplastic cells.
Laser vaporization works on the same principle as electrocoagulation, but it uses laser energy.
The choice of treatment method depends mainly on the technological capabilities of the hospital and does not prioritize one method over another. It is also necessary to focus on the volume of affected tissue and the depth of changes.
Traditional treatment of cervical metaplasia
There are many folk methods of treating this pathology, and all of them have some justification. But it is necessary to remember that this disease is quite serious and requires the same approach to treatment, therefore folk treatment can be carried out only with CIN-I and in combination with medications.
There are many recipes for treating cervical metaplasia with folk remedies. The main methods are:
- Pine treatment - half a glass of pine buds should be poured with hot water, infused, and then boiled for five minutes, after which the warm solution can be used for douching twice a day. This treatment can be carried out for a long time until complete recovery.
- The juice from the nettle leaves must be squeezed into a glass, then a tampon must be soaked in this juice and inserted into the vagina for several minutes, this procedure must be repeated once a day for a month.
- Aloe leaves, which have a pronounced anti-inflammatory and regenerating effect, are squeezed into a glass and, after wetting a tampon, inserted into the vagina, repeating the procedure once a day for a whole month.
- Propolis - use propolis ointment, which is prepared by boiling ten grams of propolis in one hundred grams of olive oil, then cooling and making vaginal tampons.
The treatment of cervical metaplasia with celandine deserves special attention. Use celandine infusion: half a glass of dry celandine leaves is poured with a liter of boiling water and taken orally two teaspoons twice a day.
You can also make an alcohol tincture and take 10 drops for ten days.
The boiled solution can be used for douching.
Homeopathic preparations used in the treatment of cervical metaplasia act primarily on the possible etiologic factor, and also stimulate epithelial regeneration and reduce inflammatory manifestations. These preparations include Allokin-alpha, Papillokan and Immunovita vaginal suppositories. The latter preparation also has a local immunomodulatory effect.
More information of the treatment
Prevention
Prevention of metaplasia development can be specific and non-specific. Non-specific prevention is a lifestyle modification with the exclusion of risk factors. Such risk factors that are subject to modification are the exclusion of bad habits, proper nutrition, exclusion of women's work in industry with hazardous substances. It is also necessary to monitor the hygiene of sexual life, because its early onset and frequent change of sexual partners is a risk factor not only for cervical metaplasia, but also for cervical cancer and breast cancer. Sexual life should be safe in terms of possible infections - infection with the human papilloma virus should be avoided as much as possible.
As for specific prevention, this is the use of vaccines. Since the only proven etiological factor in the development of cervical metaplasia in women can be considered HPV, timely vaccination against this virus reduces the risk of developing both metaplasia and malignant oncological diseases of the cervix. There is a vaccine against the human papilloma virus, which is used for girls aged 9-14 years before the onset of sexual activity. It provides immunity for a long time, which is already at least some kind of preventive measure.
Forecast
The consequences of cervical metaplasia can be very serious in case of untimely diagnosis and lack of treatment. Metaplasia is a precancerous condition that has the ability to rapidly malignize, as there is a predisposition in the form of cell dysplasia. Therefore, the prognosis in the absence of treatment is unfavorable. In case of timely diagnosis, complete reduction is possible, both conservatively and surgically, and then the prognosis is positive.
Cervical metaplasia is a serious disease that requires treatment to prevent future complications, as there is a direct risk of malignancy. It is better to prevent this condition through periodic medical examinations, as well as eliminating risk factors. If this diagnosis is established, do not worry, because it responds well to therapy, the main thing is not to delay it. Treatment depends on the stage, but, in any case, is mandatory. You need to monitor your health and start worrying in time.


 [
[