
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Bacterial vaginitis
Medical expert of the article
Last reviewed: 27.07.2025
Among inflammatory diseases of the female genital organs, the most common is inflammation of the mucous membrane lining the vagina (Latin: vagina, Greek: colpos), caused by a bacterial infection, defined as bacterial vaginitis or bacterial colpitis.
Epidemiology
Most often, inflammation of the vaginal mucosa caused by a bacterial infection is observed in women of reproductive age, and, according to some estimates, at least a third of women experience this problem at least once in their lives.
Causes bacterial vaginitis
Bacterial vaginitis (colpitis) is the result of the activation of opportunistic bacteria of the resident vaginal microbiota against the background of a violation of its homeostasis.
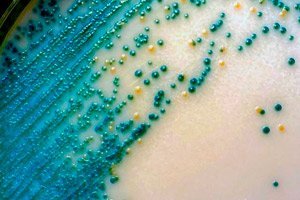
Such bacteria include obligate anaerobes of various families, including: Gardnerella vaginalis, Prevotella spp., Clostridium spp., Mobiluncus spp., Mycoplasma hominis, Fusobacterium spp., Leptotrichia spp., etc.
The vagina can also be contaminated with such intestinal commensal bacteria as Echeriсhia coli, Klebsiella aerogenes, Enterobacter cloacae, and Citrobacter freundii.
In addition, bacterial vaginitis caused by common pyogenic flora (pyogenic bacteria Staphylococcus aureus and Streptococcus pyogenes) may occur in the presence of a history of chronic inflammation of the inner lining of the uterus (endometritis) or pyelonephritis (infectious inflammation of the kidneys), due to a secondary infection during gynecological procedures, after using non-sterile intravaginal tampons, etc.
Is bacterial vaginitis sexually transmitted? No, the gonococcus Neisseria gonorrhoeae and the obligate intracellular bacterium Chlamydia trachomatis, which cause STDs – gonorrhea and chlamydia, are sexually transmitted. But trichomoniasis is not caused by bacteria, but by the protozoan (simplest) flagellate parasite Trichomonas vaginalis. Some experts define trichomoniasis in women as trichomonas vaginitis, apparently due to the similarity of the clinical picture or significant asymptomatic carriage of this pathogen: when it is present in the vaginal microflora in a dormant state for a long time.
Risk factors
Gynecologists consider the following to be risk factors for the development of bacterial colpitis:
- imbalance of vaginal microbiota;
- insufficient level of intimate hygiene;
- mechanical damage or chemical irritation of the vaginal mucosa (in particular, during douching);
- immunosuppressive conditions;
- the presence of infectious diseases (primarily of the bladder and urethra);
- hormonal imbalance with decreased estrogen levels, which can lead to a shift in the normal vaginal pH to the alkaline side (up to pH ˃6).
- menopause (postmenopausal women are at higher risk because hormonal changes also alter the pH of the vagina);
- long-term antibiotic therapy.
Pathogenesis
The pathogenesis of bacterial vaginitis is based on an inflammatory reaction and immune response to the action of bacterial toxins. How the inflammatory process develops is described in detail in the publication - Inflammation
The general condition of the vaginal microflora plays a key role in the mechanism of colpitis of bacterial etiology.
Of the total number of unicellular microorganisms, 95% are lactic acid bacteria Lactobacillus spp. (L. crispatus, L. gasseri, L. inners, L. jensenii) that live on the vaginal mucosa. They produce hydroxypropanoic (lactic) acid, hydrogen peroxide, which provide normal vaginal pH (3.8-4.5) – the main obstacle to the excessive development of opportunistic microorganisms (listed above).
A decrease in the concentration of lactobacilli leads to dysbacteriosis - an imbalance of microbiota, and its most common form is bacterial vaginosis - vaginal dysbiosis or vaginal dysbacteriosis.
Experts explain the difference between bacterial vaginosis and vaginitis. Bacterial vaginosis is not an inflammatory condition, but it creates favorable conditions for the development of opportunistic microorganisms that become active and show their pathogenic potential, which leads to inflammation - bacterial vaginitis.
Since the inflammation is caused by bacteria from the normal vaginal microflora, it is defined as non-specific bacterial vaginitis.
Symptoms bacterial vaginitis
When bacterial vaginitis develops, the first signs are changes in the color, odor, and volume of vaginal discharge.
Discharge from bacterial vaginitis often has an unpleasant odor and is accompanied by itching and burning in the genital area, for more details see - Itching and discharge in women
In addition, swelling, irritation and redness of the vulva are noted, burning and pain occur during urination, there may be pain in the lower abdomen, as well as painful sensations during sexual intercourse.
Depending on the stage, intensity and duration of the inflammatory process, the following types or forms are distinguished:
- acute bacterial vaginitis, see Acute vaginitis
- chronic bacterial vaginosis (in which symptoms may be less severe, sometimes decreasing to a minimum and periodically increasing).
When an opportunistic fungal infection is activated – the yeast-like fungus Candida albicans – bacterial vaginitis and thrush may be combined, that is, vaginal candidiasis with white, cheesy discharge that has a sour odor. First of all, candidal vaginitis differs from bacterial vaginosis in etiology; although, for simplicity, such a combination is sometimes defined as bacterial-candidal vaginitis.
During pregnancy, vaginal pH changes due to increased cervical mucus, and this changes the vaginal microbiota, resulting in bacterial vaginitis during pregnancy. Read more - Colpitis during pregnancy
Vulvovaginitis and bacterial vaginitis in girls usually develop due to infection with enterobacteria of the large intestine and rectum (Echeriсhia coli, Klebsiella aerogenes, Enterobacter cloacae) - due to poor hygiene of the perineum after defecation, and in prepubertal girls - due to low estrogen levels and age-related underdevelopment of the labia minora (and an unclosed genital slit).
Complications and consequences
Bacterial vaginitis can be complicated by inflammation of the mucous membrane of the cervical canal (endocervitis) and erosion of the cervix, as well as inflammation of the urethra - urethritis.
The consequences may include inflammation of the uterine appendages (adnexitis), uterine mucosa (endometritis) or bladder (cystitis).
Bacterial vaginitis in pregnant women can lead to miscarriage, infection of the amniotic fluid, and premature birth.
Diagnostics bacterial vaginitis
To diagnose bacterial vaginosis, a standard gynecological examination of the vagina is performed.
Instrumental diagnostics are limited to colposcopy and ultrasound examination (US) of the pelvic organs.
Laboratory tests include blood tests for antibodies, ESR, C-reactive protein, estrogen levels, as well as analysis of vaginal microflora - microscopy of a vaginal mucosa smear and determination of vaginal pH.
Differential diagnosis
Differential diagnostics are carried out with STDs, non-infectious desquamative vaginitis, inflammation of the cervix, inflammatory diseases of the pelvic organs, dermatological diseases (vulvar dermatoses, lichen planus, etc.).
Treatment bacterial vaginitis
In case of bacterial vaginitis, etiotropic treatment is carried out, and the drugs used should be aimed at combating the bacterial infection.
Therefore, antibiotics are prescribed first for bacterial vaginitis. These are Clindamycin (Dalacin), Metronidazole (Metrovit, Flagyl, Klion, Orvagil and other trade names) and similar Ornidazole and Tinidazole.
The macrolide antibiotic Azithromycin has a bacteriostatic or bactericidal effect on Streptococcus pneumoniae and Streptococcus pyogenes, Moraxella catarrhalis, Haemophilus influenzae, Echeriсhia coli and Chlamydia trachomatis. It is prescribed for bacterial pharyngitis, tonsillitis, sinusitis, otitis media, community-acquired pneumonia, and for the treatment of urogenital chlamydia.
Intravaginal suppositories are effective against bacterial vaginitis. More information:
- Vaginitis suppositories
- Treatment of colpitis with suppositories
- Vaginal suppositories for infections
Gynecologists recommend new generation suppositories for bacterial vaginitis, such as Polygynax and Vagitsin Neo, which contain the antibiotics neomycin, polymyxin B and nystatin (with antifungal action), Vagiclin (with clindamycin and clotrimazole).
Suppositories for bacterial vaginitis are inexpensive but effective: Metronidazole, Gravagin, Trichopolum and Mistol (with metronidazole); Hexitex, Klioron and Ledisept-Pharmex (with chlorhexidine); Vagiflorin (with extracts of medicinal plants and tea tree essential oil).
In the presence of candidiasis, use Pimafucin (with natamycin), Fucis (with fluconazole), Neo-penotran Forte (with metronidazole and miconazole) suppositories.
You can also use vaginal tablets for bacterial vaginitis, such as Femiclin and Flumibact IC (with the antiseptic dequalinium chloride).
Phytotherapy is used as an additional treatment – treatment with herbs: in the form of douching, vaginal irrigation and sitz baths with decoctions and infusions of chamomile flowers and calendula officinalis, sage and St. John's wort herbs, plantain leaves, lingonberries and walnuts.
For bacterial vaginitis, treatment of the partner is not required; the partner needs treatment for STIs and thrush.
Prevention
What can prevent the development of bacterial vaginitis (colpitis)? Maintaining intimate hygiene, a sufficient level of immunity, timely treatment of any infections with reasonable use of antibiotics (only as prescribed by a doctor), and it also does not hurt to periodically visit your gynecologist - to detect vaginal dysbiosis in time and improve the vaginal microflora.
Forecast
Inflammation of the vaginal mucosa caused by a bacterial infection is curable with a good prognosis for the female reproductive system.

