
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Torsion of the ovarian tumor pedicle
Medical expert of the article
Last reviewed: 04.07.2025
Tumours of various histological structures (epithelial, sex cord stroma, teratomas) that are not fused with adjacent organs and have a distinct pedicle may be subject to pedicle torsion. As a rule, these are benign and borderline neoplasms, but malignant ones may also occur.
Torsion of the anatomical and/or surgical pedicle of an ovarian tumor (when torsion occurs, the fallopian tube, less often the omentum, intestinal loops are included in these formations) is accompanied by the development of acute disruption of tumor nutrition and the rapid development of necrotic processes.
Epidemiology
"Acute" abdomen in gynecological practice may be a consequence of torsion of the mesentery of a pathologically altered or unchanged fallopian tube and ovary. But much more often, torsion of the tumor stalk (cystoma) or tumor-like, often retention, formation (cyst) of the ovary occurs. This complication is observed in 10-20% of patients with the specified pathology.
Causes ovarian tumor stem torsion
Torsion of the ovarian tumor or cyst stalk may be associated with a change in body position, physical stress, increased intestinal peristalsis, bladder overflow, cyst transition from the pelvis to the abdominal cavity, or a long, mobile cyst stalk. Increased blood pressure in the veins of the cyst stalk and cyst or in the tumor itself may play a certain role in this complication. It is known that, compared to healthy women diagnosed with ovarian cysts and cystomas, increased blood filling intensity, slower blood flow, and venous congestion are detected against the background of decreased vascular tone on the affected side.
These complications are more common in girls, young women and young women. The relative frequency of cyst pedicle torsion is characteristic in children and even in newborns.
Often, torsion of the ovarian tumor stalk occurs during pregnancy and in the postpartum period.
Pathogenesis
The anatomical pedicle of the tumor consists of a stretched ligament suspending the ovary, the proper ligament of the ovary, and the mesovary. The pedicle contains blood vessels that feed the tumor (the ovarian artery, its anastomosis with the uterine artery), as well as lymphatic vessels and nerves. The surgical pedicle is a formation that must be cut during surgery to remove the tumor. Most often, in addition to the anatomical pedicle, the surgical pedicle includes an overstretched fallopian tube.
A number of authors consider torsion to be a 90° rotation of the cyst around its stalk, while others consider it to be a 120°-180° rotation. However, it is difficult to agree with such a mechanical approach, since the degree of torsion does not yet determine the severity of the clinical manifestations of the disease. Sometimes, even with a relatively small torsion of the cyst stalk (by 90-120°), pronounced symptoms of the disease arise, while with a more significant degree of torsion (sometimes even up to 360°), signs of the disease may be absent or remain unexpressed.
Torsion of the ovarian tumor pedicle may occur suddenly (acutely) or gradually, and may be complete or partial. Pathological changes in the tumor during torsion of its pedicle depend on the speed with which the tumor rotates along the axis and on the degree of torsion. If torsion occurs slowly and is not complete, then changes are primarily observed in the thin-walled, unstable veins of the pedicle due to their compression and cessation of blood outflow, while elastic arteries continue to supply the tumor with arterial blood. As a result, pronounced venous congestion occurs: the tumor quickly increases in size, and hemorrhages into its parenchyma often occur. The tumor abruptly changes its color, its shiny, pearl-colored surface becomes yellowish-brown, copper-red, or blue-purple. Sometimes the tumor wall ruptures, resulting in bleeding into the abdominal cavity. Twisting of the tumor stalk, accompanied by compression of the arteries, leads to necrotic changes in the tumor tissues and even to peritonitis.
Symptoms ovarian tumor stem torsion
The symptoms of torsion of the cyst stalk or cystoma are practically independent of the nature of the ovarian neoplasm and are quite characteristic. The disease usually begins with severe pain in the lower abdomen, accompanied by nausea and vomiting. The onset of pain sometimes coincides with physical exertion, sudden movement. The body temperature in the first hours of the disease remains normal, the leukocyte reaction is not expressed.
In case of partial torsion of the pedicle, all symptoms are much less pronounced and may disappear even without treatment. Later, torsion of the pedicle of the cyst may be an unexpected finding during surgery for an ovarian cyst or some other abdominal disease.
In case of complete torsion of the cystoma stalk, the blood supply and nutrition of the tumor are severely disrupted. Clinically, this is manifested by the picture of an "acute" abdomen. The patient takes a forced position in bed due to the sharp pains that have arisen. Palpation reveals tension in the anterior abdominal wall, a positive Shchetkin-Blumberg symptom, intestinal paresis, stool retention, and, less often, diarrhea. The body temperature may increase, the pulse is rapid, the skin and mucous membranes become pale, and cold sweat occurs. Vaginal examination reveals a tumor in the area of the uterine appendages; attempts to displace it cause sharp pain. An important diagnostic sign of cystoma torsion is an increase in its size, which is of great importance. However, this can only be detected in cases where the patient is under the dynamic observation of a doctor. Such patients require urgent surgery - removal of the tumor.
Uncommon torsion of the uterine appendages also manifests itself as an "acute" abdomen. There is always pain in the abdomen and/or back, which increases gradually, but can also be sudden. In 50% of women, the pain is acute; sometimes it becomes dull and constant, often localized in the right or left lower quadrant of the abdomen. Nausea and vomiting are observed in 2/3 of patients, less common are urinary tract dysfunctions and a feeling of heaviness in the lower abdomen.
An objective examination reveals signs of moderate intoxication: body temperature does not exceed 38 °C; tachycardia within 100 beats/min.
Palpation of the abdomen reveals some tension in the muscles of the anterior abdominal wall and pain in the lower sections. Symptoms of peritoneal irritation are often observed. Peristaltic sounds of the intestines are heard well.
Enlarged appendages can be palpated in approximately 1/3 of patients, and 70% of patients experience pain in the area of the uterine appendages. Pain in the posterior vaginal fornix is not typical, unlike endometriosis or ectopic pregnancy. Bilateral pain in the area of the appendages may be observed with displacement of the cervix.
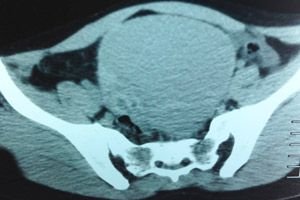
Diagnostics ovarian tumor stem torsion
The diagnosis of uterine appendage torsion is rarely established before surgery. A number of studies have shown that only in 18% of cases the diagnosis was made correctly and in a timely manner. Laboratory and instrumental studies do little to clarify the diagnosis. Leukocytosis often reaches 16 - 10 6 /l, and exceeds these values - in about 20% of patients. Ultrasound does not provide additional diagnostic information if the appendages are palpable, but helps to identify them in 80% of patients in whom they were not determined during vaginal examination. Excretory pyelography may indicate compression of the bladder or displacement of the ureter and is also used to exclude urolithiasis. Irrigoscopy may be used in tumor-like formations to exclude primary pathology of the colon. The presence of serous-bloody fluid during puncture of the posterior vaginal fornix usually does not provide additional information. Thus, we believe that when women are admitted to hospital with an acute abdomen and a tumor-like formation located in the pelvis, ultrasound, X-ray examinations and puncture of the posterior vaginal fornix, which delay the start of surgical treatment, are hardly advisable.
What do need to examine?
Differential diagnosis
Differential diagnosis of ovarian cyst pedicle torsion or ovarian cystoma is carried out with disrupted tubal pregnancy, inflammation of the appendages, ovarian apoplexy, renal colic, appendicitis and acute intestinal obstruction.
Ectopic pregnancy is characterized by delayed menstruation, dark bloody discharge from the genital tract; symptoms of internal bleeding and collapse predominate, rather than peritoneal irritation. The nature of the pain and its localization are of great value in differential diagnostics. In the case of a ruptured tube, the pain is usually sharp and strong, and in the case of a tubal abortion, it is cramping. The pain almost always radiates to the rectum and external genitalia, less often to the shoulder and collarbone (phrenicus symptom). A pregnancy test is often useful in this case.
Tuboovarian abscesses or salpingitis are usually characterized by more severe fever and leukocytosis, bilateral tenderness of the uterine appendages, and purulent discharge from the genital tract. Pus or serous fluid is found in the punctate from the abdominal cavity.
Ovarian apoplexy is most often observed in the middle of the menstrual cycle (at the time of ovulation) or in the second phase of the cycle. The clinical picture is not much different from the symptoms of an ectopic pregnancy.
In urolithiasis, tumor-like masses are not detected in the pelvic area, and erythrocytes can be found when examining urine. In renal colic, pain usually radiates downwards, dysuric disorders and pain when tapping the lumbar region are noted. Excretory pyelography in this case is an effective diagnostic procedure.
Differential diagnostics of torsion of the cyst stalk or cystoma of the right ovary and acute appendicitis may present certain difficulties. It should be taken into account that in acute appendicitis, pain usually begins in the epigastric region; appendicular symptoms (Rovsing, Sitkovsky, etc.) are positive, and vaginal examination reveals no pathological changes in the uterus or appendages.
Acute intestinal obstruction is characterized by cramping abdominal pain, stool and gas retention, flatulence, frequent pulse that precedes the temperature, and a dry tongue. The clinical diagnosis is confirmed by X-ray examination of the patient (horizontal fluid levels in the distended intestinal loops).
Errors in the diagnosis of torsion of the uterine appendages can be explained by the relative rarity of this pathology, as well as by the fact that many other diseases have a similar clinical picture. Ultrasound examination and puncture of the posterior vaginal fornix should be used to exclude other pathological conditions in patients with mild symptoms. However, in the presence of tumor-like formations in the area of the uterine appendages, accompanied by pain, symptoms of acute abdomen, or in the case of an unclear diagnosis, laparoscopy or laparotomy seems necessary to clarify the nature of the disease.
Who to contact?
Treatment ovarian tumor stem torsion
Patients diagnosed with ovarian cyst pedicle torsion or cystoma are subject to urgent surgery. A longitudinal incision is considered more preferable among other surgical approaches, as it allows for revision of the abdominal organs. After opening the abdominal cavity, before proceeding with further intervention, it is necessary to carefully examine the uterus, both ovaries, fallopian tubes, determine the condition of the peritoneum, the presence of adhesions, etc. It is necessary to obtain a clear idea of the formation originating from the ovary.
The main task of the doctor at the time of the operation is to determine the malignancy of the process, since the scope of the surgical intervention depends primarily on this. For this, along with a thorough examination of the pelvic organs and abdominal cavity, it is necessary to examine the outer and inner surfaces of the tumor capsule, as well as its contents. The outer surface of the capsule may be smooth and not raise doubts about the benign nature of the tumor, while the incision may reveal signs of malignancy (fragile, easily bleeding "papillae", "marbled" appearance of the tumor, etc.). When various complications occur, the ovarian tumor loses its characteristic appearance due to necrotic changes or the release of contents into the abdominal cavity. This significantly complicates the diagnosis and more often leads to the choice of an inadequate scope of surgical intervention than in planned operations for an ovarian tumor with an uncomplicated course.
When diagnosing a malignant ovarian neoplasm, the scope of surgical intervention, regardless of the patient's age, should be radical - panhysterectomy and resection of the greater omentum. Elderly patients with severe chronic somatic diseases may be an exception, for whom supravaginal amputation of the uterus with appendages and resection of the greater omentum or removal of the uterine appendages on both sides and resection of the greater omentum are performed. Young women with stage 1 malignant ovarian neoplasm may undergo conservative surgery in the scope of removal of the appendages from the affected ovary and resection of the second, visually unchanged, with subsequent careful observation of these patients for a number of years.
In case of a benign tumor, the surgeon's tactics depend on the tumor structure, the condition of the second ovary and the uterus, the patient's age, etc. If there is no certainty about the nature of the tumor during emergency intervention, the question of the scope of the operation is decided individually. In young women under 40 years of age, with unilateral ovarian damage and normal uterine size, unilateral removal of the uterine appendages and resection of the second ovary are performed to exclude its damage by the tumor process. In patients over 40 years of age, the scope of surgical intervention is expanded, since the risk of tumor occurrence in the remaining ovaries in women of older age groups is especially high.
If the tumor stalk is twisted, it should be cut off without untwisting, if possible above the site of the twist. This tactic is due to the fact that thrombi form in the tumor stalk, which, when it is untwisted, can separate and enter the general bloodstream.
An unfavorable course of the postoperative period after emergency intervention for ovarian tumor is somewhat more common than after planned surgical interventions. This can be explained by the presence of inflammatory and degenerative changes in complicated ovarian tumors, as well as the impossibility of good preparation of the patient for surgery in emergency conditions.


 [
[