
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Study identifies genetic switch that helps leukemia cells evade chemotherapy
Last reviewed: 18.08.2025
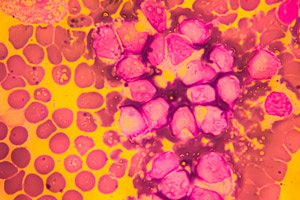 ">
">Scientists have described a molecular trick that allows acute myeloid leukemia (AML) to return so often after treatment. A new paper in Blood Cancer Discovery shows that during a relapse, an “alternative program” of the RUNX1 gene is activated in some patients: it is the RUNX1C isoform that sharply increases, triggering BTG2 and putting leukemia cells into quiescence, a state in which chemotherapy drugs have almost no effect. By blocking RUNX1C (with antisense oligonucleotides) and simultaneously giving standard chemotherapy, the researchers were able to “wake up” the cells and increase their sensitivity to treatment - in cultures and in mice.
Background of the study
Acute myeloid leukemia (AML) remains a disease of relapse: even after successful induction chemotherapy, a significant proportion of patients experience relapse. One leading explanation is the “hiding” of some cells in a state of rest (quiescence), characteristic of leukemia stem cells (LSCs). While dividing blasts die, slow and dormant clones survive the course and restart the tumor. Understanding the molecular switches of this dormancy is key to overcoming drug resistance.
RUNX1 plays a central role in the transcriptional regulation of hematopoiesis - but it is not a single protein, but a family of isoforms arising from alternative promoters and splicing. In humans, the RUNX1C isoform is encoded by the "distal" P1 promoter, while RUNX1A/1B are encoded by the "proximal" P2; the distribution of isoforms depends on the developmental stage and cell type. Isoform composition can radically alter cell behavior - from maintaining stemness to oncogenic properties - but the specific contribution of RUNX1C to AML relapse and chemoresistance has remained unclear.
In parallel, data were accumulating on the family of antiproliferative proteins BTG/Tob (in particular, BTG2), which bind to the CCR4-NOT complex and accelerate the "dehydration" of matrix RNAs (deadenylation), reducing their stability and globally suppressing protein synthesis. In the immune system, it is BTG1/BTG2 that help maintain cellular dormancy; it is logical to assume that similar mechanisms can "put to sleep" cancer cells, protecting them from cytostatics. However, a direct link between RUNX1 isoforms and BTG2 and the dormant phenotype in AML has remained a hypothesis until recently.
Another gap is methodological. Most expression studies in AML have taken into account total gene levels, without distinguishing between isoforms and rarely analyzing paired “pre-treatment → relapse” samples in the same patients. Such a design is critical if relapse is triggered not by “gene gain” but by promoter/isoform switching against the background of epigenetic shifts. Filling this gap means obtaining targets for isoform-specific therapy (e.g., RNA-targeted oligonucleotides) that can “wake up” dormant cells and make them vulnerable to chemotherapy.
Against this backdrop, a new paper in Blood Cancer Discovery is testing whether relapsed AML has an epigenetic “click” in RUNX1 with a shift toward RUNX1C, and whether RUNX1C and BTG2 form an axis that puts cells into dormancy and increases drug resistance. The authors use paired “pre-therapy/relapse” samples, RNA isoform analysis, functional assays, and isoform-specific antisense oligonucleotides - not just to describe the dormancy signature, but to test its reversibility and pharmacological vulnerability.
How did we come to this?
The authors took an unusual approach: they compared leukemia samples from the same patients before treatment and at relapse, analyzing RNA isoforms, and not just the "total" gene expression. This paired design allowed them to see that when the disease returns, it is not just the RUNX1 level that changes, but the ratio of its isoforms - it is RUNX1C that goes up. In parallel, the team checked what happens in the mechanics: they identified a "switch" on DNA (methylation of the RUNX1 regulatory region), the target of RUNX1C - the BTG2 gene, and the functional consequences - cell dormancy and drug resistance.
- Isoform matters. RUNX1 exists in several variants; their imbalance has long been suspected in hematological diseases, but the role of RUNX1C in AML relapse has been clearly demonstrated in clinical material.
- Epigenetic "click". During a relapse, a methyl mark appears in the RUNX1 regulatory zone, causing tumor cells to "switch" to producing RUNX1C.
- RUNX1C→BTG2 axis. RUNX1C activates BTG2, a known growth suppressor that inhibits transcriptional-translational processes and promotes a dormant phenotype. In this mode, cells almost do not divide - and "slip through" under chemotherapy.
What the experiments showed
- In patients (omics): in paired samples before therapy and at relapse, RUNX1C was consistently elevated; BTG2 and resting signatures rose along with it.
- In vitro: forced expression of RUNX1C made AML cells less sensitive to several chemotherapy drugs; knockout/knockdown of RUNX1C restored sensitivity.
- In mice, adding an anti-RUNX1C ASO to standard chemotherapy reduced tumor burden: cells “came out of hibernation,” began dividing—and became vulnerable to the drugs.
Why is this important?
The classic picture of AML relapse is of clonal source cells “surviving” treatment, often slow and dormant, for which cytostatics are a weak irritant. The new work identifies a specific molecular lever of this dormancy – the RUNX1C→BTG2 axis – and demonstrates that it can be pharmacologically tweaked at the level of RNA isoforms. This is a shift from a “kill the rapidly dividing cells” strategy to a “wake them up and kill them” strategy.
What can this change in practice?
- New target: RUNX1C as a therapeutic target in relapsed/chemoresistant AML. Antisense oligonucleotide (ASO) or other RNA-targeted technologies approach.
- Combinations of "ASO + chemo". The idea is to synchronize the cycle: bring the cells out of rest and treat them in the phase of maximum vulnerability.
- Selection biomarkers: RUNX1C/BTG2 elevation and RUNX1 regulator methylation at relapse are candidates for patient stratification and risk monitoring.
Context: What We Already Knew About RUNX1 and BTG2
- RUNX1 is a key transcription factor of hematopoiesis; in oncohematology it is paradoxical: it can behave as a suppressor or an oncogene - the context and isoform decide a lot.
- BTG2 is a growth/differentiation suppressor and stress signaling mediator; its activation often results in cell cycle slowing and “quiescence” – which is beneficial in normal conditions, and in tumors helps to survive the stress of therapy.
Limitations to keep in mind
- Path to the clinic. The ASO direction for oncohematology is only just forming; safety/delivery studies and precise combination regimens with chemotherapy are needed.
- Heterogeneity of AML. Not all patients relapse via the RUNX1C→BTG2 axis; validated panels will be needed to select those in whom the “switch” is truly turned on.
- Evidence of outcomes: So far shown in cells/mice and molecular profiling of patients; clinical trials are needed to talk about survival benefit.
What's next?
- Development of ASO for RUNX1C and wake-and-kill protocols with chemotherapy phasing.
- Clinical testing of biomarkers (RUNX1C, BTG2, RUNX1 methylation) for early detection of dormant resistance.
- Isoform oncology goes beyond AML: testing whether similar isoform 'switches' are hidden in other blood cancers and solid tumors.
Source: Han C. et al. An Isoform-Specific RUNX1C-BTG2 Axis Governs AML Quiescence and Chemoresistance. Blood Cancer Discovery, 2025. https://doi.org/10.1158/2643-3230.BCD-24-0327
