
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
New tool links types of Alzheimer's disease to rates of cognitive decline
Last reviewed: 02.07.2025
 ">
">Mayo Clinic researchers have discovered a series of changes in the brain characterized by unique clinical features and immune cell behavior using a new tool called the "corticolimbic index" to diagnose Alzheimer's disease, a leading cause of dementia.
Their findings are published in the journal JAMA Neurology. The tool classifies Alzheimer’s cases into three subtypes based on the location of changes in the brain and builds on the team’s previous work by showing how these changes affect people differently. Uncovering the microscopic pathology of the disease could help researchers identify biomarkers that could influence future treatments and patient care.
A new tool called the Corticolimbic Index assigns a score to the location of toxic tau proteins that damage cells in areas of the brain associated with Alzheimer's disease. The study found that differences in the accumulation of these proteins influence the progression of the disease.
"Our team found striking demographic and clinical differences in gender, age at symptomatic onset, and rate of cognitive decline," says Melissa E. Murray, Ph.D., a translational neuropathologist at the Mayo Clinic in Florida and senior author of the study.
The team analyzed brain tissue samples from a multi-ethnic group of nearly 1,400 Alzheimer's patients donated between 1991 and 2020. The samples are part of the Florida Alzheimer's Initiative Multi-Ethnic Cohort, housed at the Mayo Clinic Brain Bank. The cohort was created through a partnership with the Florida Alzheimer's Initiative.
The sample included Asians, blacks/African Americans, Hispanics/Latino Americans, Native Americans, and non-Hispanic whites who were treated at memory clinics in Florida and donated their brains for research.
To confirm the clinical utility of the tool, the researchers further studied Mayo Clinic study participants who had undergone neuroimaging during their lifetime. In collaboration with a Mayo Clinic team led by Prasanthi Vemuri, Ph.D., the researchers found that the corticolimbic index scores were consistent with changes in the hippocampus detected by MRI and with changes detected by tau protein positron emission tomography (tau-PET) in the cerebral cortex.
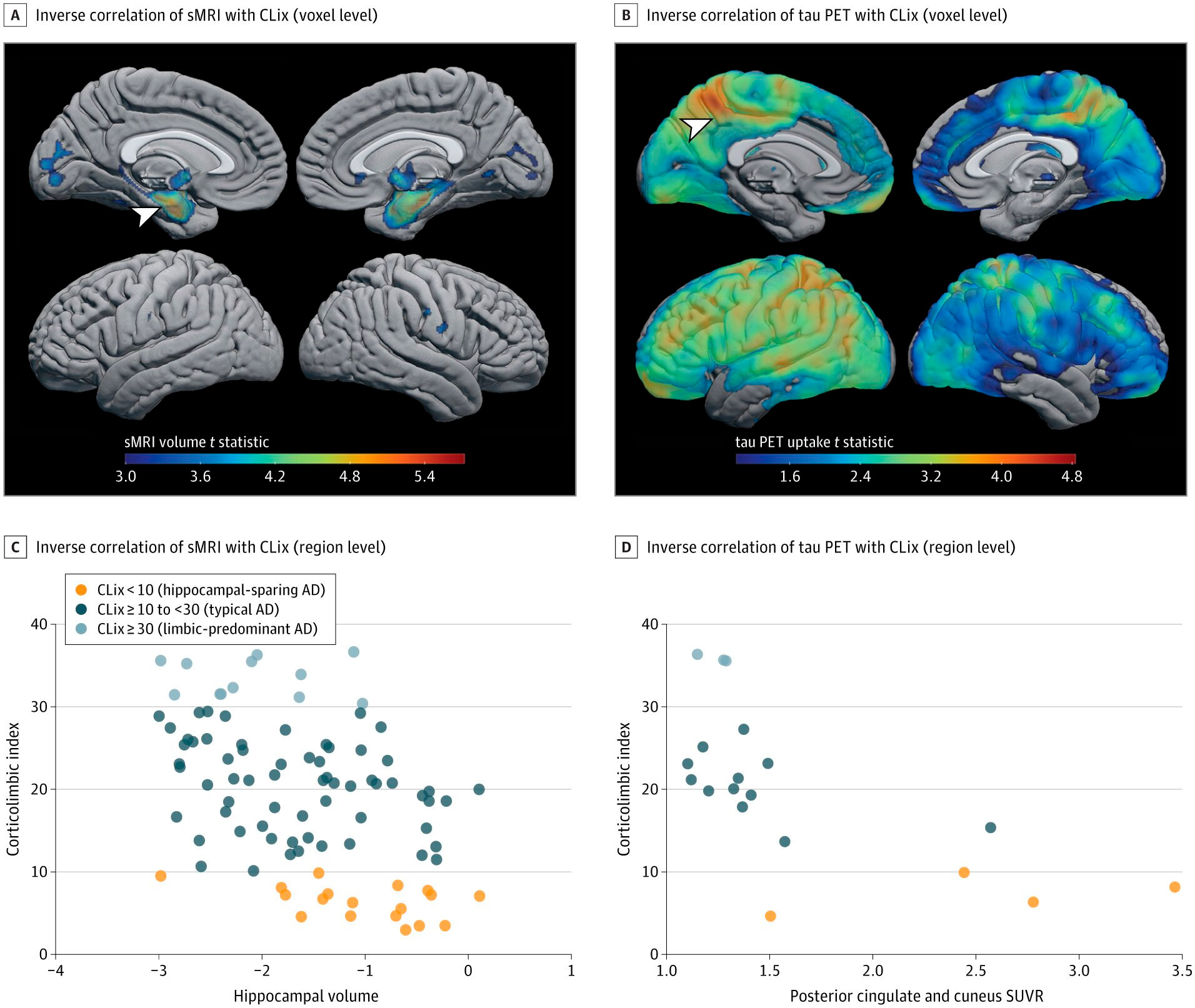
Association between structural magnetic resonance imaging (sMRI) and PET scans of tau proteins and tangle distribution in the corticolimbic region. Source: JAMA Neurology (2024). DOI: 10.1001/jamaneurol.2024.0784
"By combining our expertise in neuropathology, biostatistics, neuroscience, neuroimaging and neurology to study Alzheimer's disease from all angles, we have made significant advances in understanding how it affects the brain," says Dr. Murray.
"The Corticolimbic Index is an assessment that may contribute to a paradigm shift in understanding the individuality of this complex disease and broaden our understanding. This study represents a significant step toward personalized care, offering hope for more effective future therapies."
The next step for the research team is to translate the findings into clinical practice, making the Corticolimbic Index tool available to radiologists and other medical professionals.
Dr Murray says the tool could help doctors identify the progression of Alzheimer's disease in patients and improve clinical management. The team is also planning further studies using the tool to identify areas of the brain that are resistant to the toxic protein tau.
