
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
How the Brain “Suggests” Fatigue: fMRI Dynamics During Falling Asleep
Last reviewed: 09.08.2025
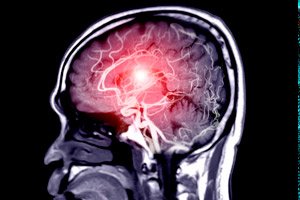 ">
">A study by Professor I. I. Gaez's team at the University of Southern California (USC), published in iScience, demonstrates new objective neuroimaging markers that can detect the onset of drowsiness at an early stage - before a person is fully asleep.
Task and relevance
Micro-sleep and momentary loss of attention lead to hundreds of traffic accidents and industrial injuries. Until now, it has been difficult to predict the exact time of “falling asleep” using subjective questionnaires or an electroencephalogram. In this study, the researchers looked at whether it is possible to detect the onset of the Sleep Onset Period (SOP) by changes in the BOLD signal in functional MRI.
Why is this important?
- Early diagnosis of fatigue. Identification of precise neuromaps helps develop methods for monitoring drivers and operators, preventing accidents due to micro-sleep.
- Sleep research. Dynamics of slow BOLD oscillations may become an objective biomarker of SOP onset, complementing psychological and electrophysiological tests.
- Neuromodulation: Targeting the thalamus or attention networks with neurostimulation could prolong wakefulness in critical situations without pharmacology.
“We have shown for the first time that the transition to drowsiness is accompanied by clear, reproducible shifts in slow fluctuations of the BOLD signal,” comments I. I. Gaez. “This opens the way to objective monitoring of fatigue based on neuroimaging.”
Experimental design
- Quorum of volunteers: 20 healthy participants (10 m/10 f, aged 22–35 years) without sleep disorders.
- Sleep in the MRI scanner: Subjects lay with their eyes closed and were allowed to fall asleep freely with the scanner playing background noise (80 dB).
- EEG (own electrodes in the scanner),
- EOM (eye movement amplitude),
- Eyelid surveillance camera.
- Definition of SOP: by the combination of half-closed eyelids, slowing of EEG rhythms and, for the first time, by changes in BOLD parameters.
Detailed analysis of the BOLD signal
- Low frequency fluctuations (0.03–0.07 Hz): in the early stages of SOP, the amplitude of these oscillations increased by 30–50% in
- thalamus (wakefulness coordination),
- occipital cortex (visual processing),
- nodes of the default mode network (DMN): medial prefrontal cortex and PCC.
- Functional connectivity:
- Thalamus ↔ prefrontal cortex: increased by 20%, indicating increased “translation” of sleep signals to the cortex.
- Attention network (DAN): Connections between the parietal and frontal lobes were reduced by 15%, reflecting a weakening of external orientation.
Correlation with fatigue
- Individual differences: Participants with less 24-hour sleep (<6 h) showed an earlier and more pronounced increase in low-frequency oscillations.
- Behavioural data: The first signs of micro-sleep (delayed response to a simple visual task in MRI) coincided with the peak amplitude of the thalamus–DMN BOLD axis.
Possible applications
- Driver and operator monitoring: transfer of fMRI findings to portable fMRI or EEG devices for early warning of fatigue.
- Personalized work schedules: taking into account the individual SOP “threshold” when planning shifts and rest, reducing accidents.
- Sleep therapy: testing the effects of caffeine, short naps, and neuromodulation (transcranial magnetic stimulation) on slowing BOLD shifts.
Authors' quotes
“We have shown for the first time how slow BOLD oscillations in the thalamus and cortex predict sleep onset,” comments Prof. Gaez. “This opens the way to developing objective ‘physiological eyes’ to monitor alertness.”
“Our findings allow us to rethink fatigue management: it is no longer enough to ask, ‘How did you sleep?’ – we need to be able to ‘see’ the brain,” adds co-author Dr. Li Jing.
The authors highlight the following key points:
Neurobiological reliability of markers
“The increase in low-frequency fluctuations of the BOLD signal in the thalamus and the passive mode network clearly correlates with objective signs of drowsiness (eyelid closure, EEG slowing), - notes I. I. Gaez. - This proves that SOP can be “seen” not only by behavior, but also directly by brain activity.”Individual differences
“We found that people with chronic sleep deprivation showed earlier and more pronounced BOLD shifts,” says Dr. Lee. “This opens up the possibility of personalizing fatigue-fighting strategies: some may need more frequent ‘microsleep’, while others may need light therapy or neurostimulation.”Translation into practice
“The next step is to adapt these markers to portable technologies (fNCD, dry EEG caps) to monitor vigilance in real time in drivers and operators,” adds Prof. Martinez.Clinical Perspectives
“The changes found may also help in diagnosing sleep disorders: insomnia, apnea and narcolepsy have different effects on the early phase of SOP, and the BOLD marker will help differentiate these conditions,” Dr. Singh concludes.
This research paves the way for accident and injury prevention neurotechnologies based on real-time and individual markers of drowsiness onset, and promises to make roads and industrial sites safer.
