
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Gliomas in the crosshairs of flavonoids: mechanisms of action and smart forms of delivery
Last reviewed: 18.08.2025
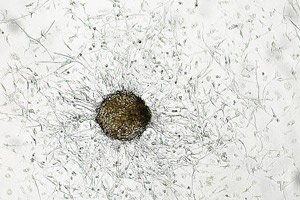 ">
">Gliomas are the most common tumors of the central nervous system, and glioblastoma remains their most aggressive face. Even with surgery, radiation therapy, and temozolomide, the prognosis for many patients is grim. Against this backdrop, unconventional ideas are being used - from viral vectors to... food polyphenols. A new review in Nutrients has collected data on three "stars" of plant flavonoids - luteolin, quercetin, and apigenin - and their antitumor effects in cell and animal models of gliomas, and at the same time has dismantled the main obstacle: how to deliver these molecules through the blood-brain barrier (BBB) and keep them in the blood long enough to be useful.
In short: all three compounds can stop glioma cell division, trigger apoptosis, interfere with vessel formation and tumor migration - but bioavailability is low, metabolism is fast, and they pass through the BBB poorly. Therefore, the main progress now is in smart delivery forms (nanoliposomes, mikeles, "bilosomes", PLGA nanoparticles and even intranasal gel systems).
Background
Gliomas are the most common primary CNS tumors, and glioblastoma remains their most aggressive variant: even with surgery, radiotherapy and temozolomide, the prognosis is often unfavorable. This prompts the search for adjuvant and combined approaches that can simultaneously attack tumor proliferation, invasion, angiogenesis and drug resistance. Against this background, there is growing interest in dietary polyphenols - molecules with multi-target action (regulation of PI3K/AKT/mTOR, NF-κB, glycolysis, EMT, angiogenesis), among which the flavonoids luteolin, quercetin and apigenin stand out. In preclinical models of gliomas, they inhibit cell growth and migration, trigger apoptosis and increase sensitivity to radiation/chemotherapy.
However, the main reason why “natural” candidates have not yet reached the clinic is pharmacokinetics and delivery barriers. Luteolin, quercetin, and apigenin are characterized by low solubility and rapid conjugation, and they pass poorly through the blood-brain barrier; “plate” concentrations are obviously insufficient for therapeutic effect. Therefore, the focus of research is on smart carriers (nanoliposomes, polymeric micelles, PLGA nanoparticles, “bilosomes”, intranasal gels) that increase bioavailability, prolong circulation and improve tumor penetration, as well as testing synergies with radiation therapy and temozolomide for dose-sparing regimens. It is this translational gap - between convincing biology and delivery to the target - that the modern literature is trying to close.
Ultimately, the scientific challenge is to confirm in standardized preclinical models that flavonoid nanoforms reach effective concentrations in tumor tissue and improve “hard” outcomes (volume, Ki-67, angiogenesis, survival), identify biomarkers of response (including microRNA signatures and metabolic effects), and then transfer the best candidates to early clinical trials as adjuvants to current standards.
Who is who and how it works
- Luteolin (parsley, celery, thyme, mint): in glioma models, it downregulates PI3K/AKT/mTOR pathways, increases ROS stress and mitochondrial permeability, activates caspases 3/8/12, shifts lipid mediator balance toward ceramides (anti-tumor signaling), and downregulates S1P. There is evidence of an effect on microRNAs (miR-124-3p, miR-17-3p) and the RNA-binding protein Musashi regulator, which indirectly reduces invasion and drug resistance. In mice, GBM xenografts shrink without weight loss or hepatotoxicity.
- Quercetin (onions, apples, berries, cabbage): in addition to the antiproliferative effect, synergizes with classical chemotherapy (in a number of models - with cisplatin; in glioma - with temozolomide, it reduced toxicity to body weight). In xenografts, it reduced tumor volume, Ki-67, inhibited EMT (N-cadherin, vimentin, β-catenin, ZEB1 fell; E-cadherin grew), and nanoforms with quercetin interrupted neoangiogenesis through VEGFR2.
- Apigenin (chamomile, parsley, celery, thyme): inhibits migration and triggers apoptosis in cells; in living models, the effect is less stable. In one study, only a moderate response was obtained against C6 glioma; in another, apigenin acted as a radiosensitizer - it suppressed glycolysis (HK, PFK, PK, LDH), reduced GLUT1/3 and PKM2, and thus made cells more sensitive to 8 Gy irradiation.
Almost all of these molecules suffer from the same problem: poor solubility, low oral bioavailability, rapid conjugation in the liver, and poor penetration of the blood-brain barrier. So researchers are turning to delivery technologies - and this seems to work.
How they are "delivered" to the target
- Nanoliposomes and polymeric micelles (including MPEG-PCL): stabilize the molecule, improve the distribution profile, increase absorption by glioma cells.
- Bilosomes and chitosan-coated systems for the intranasal route: increase membrane fluidity/retention time in the nasal cavity and improve access to the CNS, bypassing some barriers.
- PLGA nanoparticles, “magnetoliposomes”, albumin/lactoferrin conjugates, etc.: improve transport across the BBB and accumulation in the tumor; individual platforms specifically carry quercetin + metabolic inhibitor (3-BP), which reduced angiogenesis and tumor volume in mice.
To be fair, this is all still preclinical. None of the compounds have yet made it to randomized trials in patients with gliomas, and the comparability of animal studies is limited by different designs, doses, and durations. But there are some clues about what to combine them with.
What can enhance the effect in the future
- Combinations with radiotherapy (apigenin as a radiosensitizer) and with temozolomide/other cytostatics (quercetin/luteolin) are an idea for testing dose-sparing regimens.
- MicroRNA profiling: luteolin/apigenin likely alter tumor gene regulation 'network'; systematic omnics could suggest targets and response biomarkers.
- PK/PD modeling: will help to select dosing regimens and “windows” for maintaining therapeutic concentrations in tumor tissue with minimal risks.
- Standardization of models: today, the diversity of methods makes it difficult to compare effects between studies; protocols with uniform endpoints (volume, Ki-67, vascular density, survival) are needed.
Finally, an important "earthly" conclusion: drinking chamomile tea or eating more parsley is, of course, good, but not a glioma therapy. The concentrations effective in experiments are incomparable with those provided by a regular diet, and the dietary supplement approach has both risks and illusions. If these molecules have a clinical future, then in nanoforms and in combination regimens, and not as independent "natural drugs."
Summary
Luteolin, quercetin and apigenin show convincing anti-glioma activity in cell lines and animals, but their path to the clinic is limited by pharmacokinetics and the BBB. The arsenal already includes technological solutions for delivery and logical combinations with radiotherapy/chemotherapy; the next step is well-designed preclinical and clinical trials with response biomarkers.
Source: Justyńska W., Grabarczyk M., Smolińska E., et al. Dietary Polyphenols: Luteolin, Quercetin, and Apigenin as Potential Therapeutic Agents in the Treatment of Gliomas. Nutrients. 2025;17(13):2202. https://doi.org/10.3390/nu17132202
