
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Yersiniae
Medical expert of the article
Last reviewed: 08.07.2025
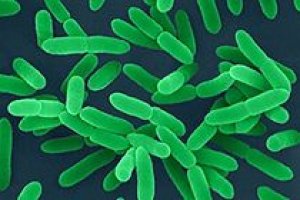 ">
">Y. pseudotuberculosis and Y. enterocolitica are not classified as particularly dangerous, but they also play a significant role in human pathology. Y. pseudotuberculosis and Y. enterocolitica are polymorphic, non-spore-forming gram-negative rods, often ovoid in shape, with unevenly stained cells in old cultures. Pseudotuberculosis bacteria taken from wet agar may have bipolar staining, form a capsule, but with varying degrees of severity. Both types of bacteria, unlike Y. pestis, have mobility due to the presence of peritrichous flagella. Mobility is detected by sowing in a column of semi-liquid agar by injection, but only at 18-20 °C, at 37 °C it is absent. Yersinia are undemanding to nutrient media, grow well on ordinary universal media, and are capable of actively multiplying in soil and water. The optimum temperature for growth is 30 °C, the upper and lower temperature limits of growth are 43 °C and 0-2 °C, respectively, the pH range is 6.6-7.8. On Endo medium, after 24 hours, the colonies have a diameter of 0.1-0.2 mm, are round, convex, shiny, with smooth edges, colorless (do not ferment lactose), after several days the colony size is 0.5-3 mm. Colonies of the pseudo-tuberculosis pathogen, which are in the R-form, are almost indistinguishable from colonies of Y. pestis (pigmented center and scalloped "lace" edge), but do not have the "broken glass" stage.
All three types of Yersinia also differ in their antigenic properties.
The pseudo-tuberculosis pathogen is divided into eight groups (I-VIII) with 20 O-factor antigens (1-20) according to O-antigens. According to O- and H-antigens (a-e), this species is divided into 13 serovars and subserovars (la, lb? IIa, IIb, IIc, III, IVa, IVb, Va, Vb, VI, VII, VIII).
Y. enterocolitica is characterized by heterogeneity in O-antigen. There are 34 serovars of this species. Most of them are adapted to certain animal species or are widespread in the environment. The vast majority of strains isolated from humans belong to serovars 03 and 09, less common are serovars 06, 08, 05, and very rare are serovars 01, 02, 010, 011, 013-017.
Strains of serotypes I (lb), III and IV are most often isolated from patients with pseudotuberculosis.
During the course of evolution, Yersinia acquired the need to exist in two environments - external (saprophytic phase) and in the body of warm-blooded animals and humans (parasitic phase). To implement the parasitic phase, Yersinia must penetrate the body of a warm-blooded animal. Infection with the pseudotuberculosis pathogen most often occurs when eating Yersinia-infected products stored at a low temperature (4-12 °C) in refrigerators and vegetable stores. Under these conditions, due to their psychrophilicity, the bacteria can multiply and accumulate in food substrates. An example of this method of infection is the disease of 106 people with pseudotuberculosis in the Krasnodar Territory in 1988, associated with the use of cabbage infected with Y. pseudotuberculosis. Its main reservoir is soil.
At low temperatures, Yersinia has a high potential for cellular and tissue invasiveness and is capable of maintaining a high level of virulence, but the pathogen can penetrate the human body through any mucous membranes, probably due to non-specific mechanisms. Wild and synanthropic rodents, domestic and farm animals are also the source of yersiniosis. Human-to-human infection is possible.
Strains of Y. pseudotuberculosis have been isolated from 175 species of mammals, 124 species of birds, and 7 species of fish. Infected rodents, animals, and humans excrete the pathogen with feces and urine, contaminating water, plants, and other environmental objects, and humans become infected through them. Thus, the food route is the leading one in the transmission of pseudotuberculosis and intestinal yersiniosis pathogens: infection occurs as a result of eating raw or insufficiently cooked foods (meat, meat products, milk, vegetables, fruits, greens). Both types of pathogens are capable of reproducing not only on plants, but also inside them (lettuce, peas, oats, etc.).
Diseases caused by Yersinia are characterized by polymorphic clinical manifestations, damage to the gastrointestinal tract, a tendency to generalization, septicopyemia and damage to various organs and systems.
Y. enterocolitica causes gastroenteritis in humans with damage to the walls of the small intestine. Autoimmune spondyloarthritis such as Reiter's syndrome and reactive arthritis are often observed after the disease. It is believed that these consequences are associated with the presence of superantigens in Y. enterocolitica. The membrane proteins of these bacteria have the properties of superantigens.
Pseudotuberculosis of people in the Far East is described as Far Eastern scarlet fever-like fever. It is more severe than pseudotuberculosis in the western regions and is characterized by stronger allergic and toxic manifestations, especially in the 2nd stage of the disease.
Pathogenic properties of both Yersinia species, as well as the plague pathogen, are determined not only by chromosomal but also by plasmid genes. They have plasmids very similar to those of Y. pestis, which code for the synthesis of VW antigens and external proteins (Yop), the same as in Y. pestis, and other virulence factors. They have a common gene cluster with Y. pestis associated with the iron transport system. It has been established that Y. pseudotuberculosis synthesizes a heat-stable toxin that causes death in guinea pigs with intraperitoneal infection. The ability of the pathogen to adhere to and colonize the intestinal mucosa plays an important role in the pathogenesis of pseudotuberculosis.
Microbiological diagnostics of yersiniosis includes the use of bacteriological methods and serological reactions. In the bacteriological method, the material to be examined from the patient (feces, blood, mucus from the pharynx), as well as suspicious products or water, are inoculated onto Endo, Ploskirev, Serov (indicator and differential) media and incubated at 37 °C for 48-72 hours. Suspicious colonies (small colorless on Endo and Ploskirev media and colored colonies of two different forms on Serov media) are reseeded to obtain pure cultures, which are identified by biochemical characteristics and finally typed using diagnostic agglutinating sera.
For serological diagnostics of pseudo-tuberculosis and intestinal yersiniosis, a detailed agglutination reaction (like the Widal reaction) with the corresponding diagnosticums or RPGA with an antigen erythrocyte diagnosticum is used. Reactions with an antibody titer of 1:400 and higher are considered positive. It is recommended to conduct reactions with paired sera at intervals of several days. An increase in the antibody titer indicates the specificity of the infectious process.

