
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
What triggers Icenko-Cushing's disease?
Medical expert of the article
Last reviewed: 04.07.2025
The causes of Itsenko-Cushing's disease have not been established. In women, Itsenko-Cushing's disease most often occurs after childbirth. In the anamnesis of patients of both sexes, there are head injuries, concussion, skull injuries, encephalitis, arachnoiditis and other CNS lesions.
The pathogenetic basis of Itsenko-Cushing's disease is a change in the mechanism of control of ACTH secretion. Due to a decrease in dopamine activity responsible for the inhibitory effect on the secretion of CRH and ACTH and an increase in the tone of the serotonergic system, the mechanism of regulation of the hypothalamic-pituitary-adrenal system and the daily rhythm of CRH-ACTH-cortisol secretion are disrupted; the principle of "feedback" with a simultaneous increase in the level of ACTH and cortisol ceases to operate; the reaction to stress disappears - an increase in cortisol under the influence of insulin hypoglycemia.
In most cases, pituitary adenomas are detected. Macroadenomas are found in 10% of patients, while the rest have microadenomas, which are not detected by conventional radiography of the sella turcica and can only be diagnosed by computed tomography during surgical diagnostic adenomectomy (in a small number of patients, tumors are not found, but hyperplasia of basophilic cells of the pituitary gland is detected during histological examination).
Tumor cells from removed pituitary adenomas in Itsenko-Cushing's disease give a positive immunocytochemical reaction to ACTH, beta-lipotropin, beta-endorphin, alpha-MSH and met-enkephalin.
At present, it has not been conclusively proven whether pituitary tumors in Itsenko-Cushing's disease are a primary pituitary lesion or their development is associated with a disorder in the overlying parts of the central nervous system. The probability of a central origin of adenomas is indicated by a disturbance in the secretion rhythm of not only ACTH and cortisol, but also somatotropic hormone and prolactin, resistance to exogenous corticosteroids, and the absence of stages III and IV in the slow sleep phase; against this - restoration of daily secretion of ACTH and cortisol after removal of a pituitary tumor in a significant number of patients. Most ACTH-secreting adenomas are localized in the anterior lobe of the pituitary gland (60%), the rest - in its posterior and middle parts.
The pathogenesis of Itsenko-Cushing's disease is based on both increased secretion of ACTH by the pituitary gland and the release of cortisol, corticosterone, aldosterone, androgens by the adrenal cortex. Chronic long-term cortisolemia leads to the development of a symptom complex of hypercorticism - Itsenko-Cushing's disease.
Disturbances in the hypothalamic-pituitary-adrenal relationship during the disease are combined with changes in the secretion of other pituitary tropic hormones. The secretion of somatotropic hormone is significantly reduced, the level of gonadotropins and TSH decreases, and prolactin increases.
Muscle tissue atrophy and the appearance of red stripes on the skin of the abdomen and thighs are associated with a violation of protein metabolism. Atrophic processes affect striated muscles and are especially noticeable in the muscles of the upper and lower extremities. When examining muscle tissue, severe damage to mitochondria is detected.
The redness, marbling, thinning and dryness of the skin characteristic of Cushing's disease are associated with both polycythemia and skin atrophy caused by increased catabolism and decreased collagen synthesis, which lead to capillary translucency. Thinning of the skin and rapid fat deposition lead to the appearance of stretch marks (striae). They are found in 77% of patients and usually occur earlier or simultaneously with other symptoms and are very characteristic of this disease. Their absence does not exclude Cushing's disease.
The effect of excess of the main corticosteroid, cortisol, in the body is that with the disruption of enzyme systems, the processes of dissimilation and deamination of amino acids are accelerated. The result of these processes is an increase in the rate of protein breakdown and a slowdown in their synthesis. The disruption of protein metabolism leads to an increase in the excretion of nitrogen in the urine and a decrease in the level of albumins.
A characteristic symptom of the disease is muscle weakness, which is explained by dystrophic changes in muscles and hypokalemia. Hypokalemic alkalosis is associated with the effect of glucocorticoids on electrolyte metabolism. Hormones promote sodium retention in the body, which leads to the excretion of potassium salts. Potassium content in plasma, erythrocytes, muscle tissue and heart muscle is significantly reduced.
The pathogenesis of arterial hypertension in Itsenko-Cushing's disease is complex and poorly understood. An undoubted role is played by disturbances in the central mechanisms of vascular tone regulation. Hypersecretion of glucocorticoids with pronounced mineralocorticoid activity, in particular corticosterone and aldosterone, is also important. Dysfunction of the renin-angiotensin system leads to the development of persistent hypertension. Long-term hyperproduction of cortisol leads to an increase in the content of renin, which participates in the formation of angiotensin I and causes an increase in arterial pressure. The loss of potassium by muscle cells causes changes in vascular reactivity and an increase in vascular tone. Potentiation of the effect of catecholamines and biogenic amines, in particular serotonin, by glucocorticoids also plays a certain role in the pathogenesis of hypertension.
In the pathogenesis of osteoporosis in Itsenko-Cushing's disease, the catabolic effect of glucocorticoids on bone tissue is of great importance. The mass of bone tissue itself, as well as the content of organic matter and its components (collagen and mucopolysaccharides) in it, decreases, the activity of alkaline phosphatase falls. Due to the preservation of mass and disruption of the structure of the protein matrix, the ability of bone tissue to fix calcium decreases. A significant role in the development of osteoporosis belongs to a decrease in calcium absorption in the gastrointestinal tract, which is associated with the inhibition of calciferol hydroxylation processes. The destruction of protein components of bone and secondary demineralization lead to osteoporosis. The excretion of large amounts of calcium by the kidneys causes nephrocalcinosis, the formation of kidney stones, secondary pyelonephritis and renal failure. Disturbances of carbohydrate metabolism in Itsenko-Cushing's disease are accompanied by an increase in the functions of alpha-, beta- and 6-cells of the pancreas. In the pathogenesis of steroid diabetes, relative insulin deficiency, insulin resistance and an increase in the level of counter-insular hormones are of great importance.
Pathological anatomy of Itsenko-Cushing's disease
In Itsenko-Cushing's disease, damage is often localized in the paraventricular and supraoptic nuclei of the hypothalamus and leads to diffuse or focal hyperplasia of corticotrophs and/or their hyperfunction, as evidenced by hypertrophy of cells and their organelles. In more than 50% of cases, this leads to the formation of microadenomas from ACTH-producing cells with a semi-autonomous nature of functioning. Some of them are primary pituitary adenomas. In 5-15% of patients, adenomas are basophilic-cellular and represent small solitary tumors of the anterior lobe with specific neurosecretory granules 250-700 nm in diameter, located along the cell membrane, and bundles of microfilaments around the nucleus. The majority of adenomas are mixed-cellular (from basophils and chromophobes), less often - chromophobic-cellular. Tumor chromophobes are obviously a variant of basophils of the intermediate lobe of the pituitary gland, specializing in the formation of ACTH. Some corticotropinomas are tumors of the intermediate lobe. They are often multiple and contain nervous tissue. In the tissue of the anterior lobe surrounding the tumor, hyalinization of basophils is observed, characteristic of excess corticosteroids of any origin. Some cells of the paraadenomatous tissue have degenerative changes, and the stroma is often fibrotic. Malignant variants of corticotropinomas with aggressive growth are possible.
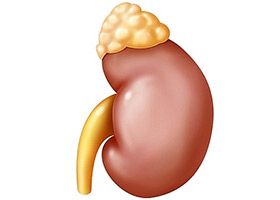 Hyperproduction of ACTH causes an increase in the mass of adrenal tissue and an increase in the functional activity of cells due to an increase in their number (hyperplasia) and hypertrophy. These phenomena are most pronounced in ectopic ACTH syndrome. In children, signs of increased functional activity of adrenal cells predominate, in people over 30 years of age - hyperplasia and hypertrophy of the organ. The adrenal glands removed at stage II of surgical treatment are always larger than those removed at stage I. The mass of the adrenal gland does not depend on the age of the patients or on the mass of the previously removed one. Microscopically, they are characterized by thickening of the fascicular zone and, to a lesser extent, the reticular zone. Changes in the glomerular zone are varied: from atrophic to focal hyperplastic. In 30% of patients, hyperplasia is diffuse-nodular. Nodules are formed mainly in the fascicular zone, often growing through the capsule of the adrenal gland and forming mushroom-shaped outgrowths on the surface. Their functional activity is comparable to the activity of the entire cortex. In people over 40 years of age, nodules of pseudotubular structures with low functional activity are formed, the cells of which are overfilled with lipids. Diffuse-nodular hyperplasia in 1/3 of patients also develops in the accessory adrenal tissue.
Hyperproduction of ACTH causes an increase in the mass of adrenal tissue and an increase in the functional activity of cells due to an increase in their number (hyperplasia) and hypertrophy. These phenomena are most pronounced in ectopic ACTH syndrome. In children, signs of increased functional activity of adrenal cells predominate, in people over 30 years of age - hyperplasia and hypertrophy of the organ. The adrenal glands removed at stage II of surgical treatment are always larger than those removed at stage I. The mass of the adrenal gland does not depend on the age of the patients or on the mass of the previously removed one. Microscopically, they are characterized by thickening of the fascicular zone and, to a lesser extent, the reticular zone. Changes in the glomerular zone are varied: from atrophic to focal hyperplastic. In 30% of patients, hyperplasia is diffuse-nodular. Nodules are formed mainly in the fascicular zone, often growing through the capsule of the adrenal gland and forming mushroom-shaped outgrowths on the surface. Their functional activity is comparable to the activity of the entire cortex. In people over 40 years of age, nodules of pseudotubular structures with low functional activity are formed, the cells of which are overfilled with lipids. Diffuse-nodular hyperplasia in 1/3 of patients also develops in the accessory adrenal tissue.
In the pubertal-juvenile, often familial form of Itsenko-Cushing's disease with pigmented multinodular dysplasia of the adrenal cortex, the latter are of normal size and mass. They are easily verified by the presence of numerous nodular inclusions of dark brown color on the cut surface; microscopically, they are characterized by the presence of numerous nodular formations surrounded by an atrophied cortex and formed by large cells with hypertrophied, often polymorphic nuclei, the cytoplasm is oxyphilic, contains brown pigment. The latter have an unusually high functional activity. The stroma of the nodules is infiltrated by lymphoid elements and fat cells.
Menstrual and reproductive dysfunctions in Itsenko-Cushing's disease are caused by early-onset but reversible atrophic changes in the endometrium with thinning of the functional layer, a decrease in the number of glands, and cystic degeneration of those that remain. Changes in the ovaries occur later. They are reduced to atrophic changes due to the death of the follicular apparatus, disturbances in the maturation of the remaining follicles, atrophy of the interstitial tissue, disappearance of hilus cells, and reduction of the elements of the ovarian network.
Atrophic changes with a decrease in functional activity also develop in other endocrine glands: testicles, parathyroid glands, etc.

