
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Ventriculitis
Medical expert of the article
Last reviewed: 04.07.2025
If a doctor diagnoses ventriculitis, it means that a complication has developed that threatens not only the health but also the life of the patient. The pathology is an inflammatory reaction that affects the walls of the cerebral ventricles: it is a serious intracranial infectious disease that develops in patients suffering from various disorders of the central nervous system - in particular, the primary problem may be traumatic brain injury, intracranial surgery, infectious and inflammatory diseases. The mortality rate from complications is very high. [ 1 ]
Epidemiology
If we consider statistical information on ventriculitis, we can see that most authors mention the frequency of cases of the disease, either depending on their cause or as complications of other pathologies of the nervous system. Separate statistics on ventriculitis are not kept.
According to the American Center for Disease Control and Prevention, in general, infectious lesions of the central nervous system are in eleventh place among all hospital infections, with an incidence rate of 0.8% (more than 5.5 thousand patients annually).
To date, the most studied pathogenetic type of the disease is ventriculitis, which developed as a result of the ventricular drainage procedure. In such cases, ventriculitis developed in 0-45% of patients. If we consider the frequency of complication development by the duration of drainage, the figure is 11-12 patients per thousand drainage days. At the same time, over the years, the number of cases gradually decreases, which may be due to the improvement of medical manipulation and diagnostic techniques, as well as the optimization of the quality of processing surgical instruments.
Some experts have drawn a parallel in the occurrence of ventriculitis and meningoencephalitis following neurosurgical operations. The prevalence of such pathologies, according to various sources, is 1-23%: such a wide percentage range is associated with the different diagnostic criteria used in research. Many studies took into account only those cases in which cerebrospinal fluid cultures revealed the growth of certain pathogenic microorganisms. [ 2 ]
The incidence of ventricular catheter-associated ventriculitis (or healthcare-associated ventriculitis) ranges from 0 to 45% depending on insertion technique and treatment (usually less than 10%).[ 3 ],[ 4 ]
Causes ventriculitis
Ventriculitis is an infectious disease. In newborns, infection occurs in utero. In older patients, the causes are most often the following:
- Open craniocerebral traumatic injuries, fractures of the base or cranial vault, other injuries that cause damage to the brain tissues located in the periventricular zone, as well as the formation of cerebrospinal fistulas through which the infection penetrates. An inflammatory reaction develops when pathogenic flora enters the ventricular space.
- Penetrating cranial injuries – in particular, gunshot wounds, penetration of various foreign objects, which entails the penetration of infection into brain tissue.
- A brain abscess localized near the ventricular system. When the lesion spontaneously opens, its internal purulent contents leak into the ventricle or into the periventricular space. As a result, ventriculitis develops.
- Inflammation of the brain, encephalitis, can spread to the ventricles - in particular, infectious agents enter the ventricular cavity.
- Purulent inflammation of the meninges. The spinal meninges are closely adjacent to the subarachnoid space, which is filled with cerebrospinal fluid and is part of the general cerebrospinal fluid system. Pathogenic flora enters the spinal tracts, spreads through the ventricles, causing an inflammatory process such as ventriculomeningitis.
- Neurosurgical operations. In case of aseptic violations during the operation in the area of the brain ventricles, penetration of an infectious agent into the ventricular space is possible. This is possible with insufficient sterilization of surgical instruments, such as a puncture needle, drains, etc.
Increased risk factors for developing ventriculitis include cases of trauma and other cranial injuries, surgical manipulations on the brain, and intrauterine infection of the fetus (septic processes). [ 5 ]
Risk factors
The risk group for developing ventriculitis includes patients with the following characteristics:
- oncological pathologies, chronic hematological disorders;
- drug addiction, chronic alcohol dependence;
- frequent traumatic brain injuries;
- endocrine disorders;
- immunodeficiency states of various origins (genetic diseases, HIV infection, asplenia, etc.);
- old age (over 70 years). [ 6 ]
Additional risk factors for the development of ventriculitis include:
- late visit to the doctor (later than the third day from the moment the pathological process developed);
- incorrectly provided first aid at the pre-hospital stage, or lack of necessary assistance;
- cerebral arterial atherosclerosis with signs of cerebrovascular insufficiency against the background of hypertension.
If the patient belongs to one of the risk groups or has any of the risk factors, then this clearly indicates a high probability of a severe or complicated course of the pathology, which may require emergency and competent use of therapeutic and rehabilitation measures. [ 7 ]
Significant factors in the development of ventriculitis are:
- presence of blood in the ventricles or subarachnoid space;
- presence of other systemic infections;
- cerebrospinal fluid leakage, particularly in patients with penetrating head injuries;
- prolonged drainage of the cerebral ventricles and the introduction of washing fluids into them.
Many experts point to the involvement of frequent CSF collection by catheterization for examination in the development of ventriculitis. According to some information, if catheterization continues for more than one week, this significantly increases the likelihood of developing an infectious process. However, the question of the duration of drainage and the need for prophylactic replacement of the catheter is still controversial. Some authors suggest tunneling the catheter to reduce the risk of ventriculitis from the burr hole to the area of exit from the skin. It is recommended to make an indentation of less than 50 mm from the burr hole, or to bring the catheter out in the chest area or the upper segment of the anterior abdominal wall. [ 8 ]
Pathogenesis
There are different ways for an infectious agent to enter the cerebral ventricles. Thus, the development of ventriculitis can start as a result of direct delivery of pathogenic microorganisms from the external environment. This happens with open craniocerebral injuries, during neurosurgical operations - for example, the risk zone includes such interventions as the installation of ventricular drainage in patients with hemorrhages in the cranium, acute hydrocephalus, valve spinal shunting, and other operations with open access. Contact spread of infection during the opening of a brain abscess into the ventricular system, hematogenous spread during the circulation of bacteria in the bloodstream, cerebrospinal penetration during the reverse flow of cerebrospinal fluid in patients with primary and secondary meningitis or meningoencephalitis are also possible.
Presumably, the reverse flow of cerebrospinal fluid occurs during the transformation of the pulsatile movement of cerebrospinal fluid through a deterioration in the elasticity of the intracranial subarachnoid spaces, which is caused by inflammatory changes or hemorrhage. [ 9 ]
The indicated mechanism of ventriculitis development determines the frequent association of the disease with an inflammatory process in the meninges. [ 10 ]
As a result of the opening of a brain abscess into the ventricular system, ventriculitis also occurs. But another, "mirror" variant is also often encountered: with a complicated course of ventriculitis, an encephalitis focus develops in the adjacent tissues with the formation of a brain abscess.
Symptoms ventriculitis
If ventriculitis develops against the background of penetrating traumatic or wound injuries, the patient experiences a strong and sudden general deterioration in health. The body temperature rises, and the indicators exceed 38 ° C. A similar picture is observed with spontaneous opening of a brain abscess. If patients are conscious, then most often they voice complaints of severe headaches and increasing agitation. There is a significant increase in heart rate (more than 120-130 beats per minute), paleness or redness of the skin (which is especially noticeable on the face), shortness of breath, vomiting, after which it does not become easier. Meningeal syndrome is clearly defined.
Increased motor activity (psychomotor agitation) is replaced by tonic-clonic or clonic seizures. During the attacks, progressive impairment of consciousness is observed. The patient becomes lethargic, inhibited, sleepy: the stage of stupor begins with a gradual lapse into a comatose state. The patient's body is exhausted, which may be accompanied by a slight decrease in temperature to the level of subfibrillation, as well as a decrease in the intensity of meningeal manifestations.
If ventriculitis develops in a newborn baby as a result of intrauterine infection, then there is a serous inflammatory process that is not accompanied by any clinical signs. The pathology is determined during ultrasound diagnostics. When the pathology develops as a septic complication, pathognomonic symptoms are absent, but the baby's condition worsens significantly. [ 11 ]
The initial clinical picture of ventriculitis development quickly makes itself known, as it develops literally "before our eyes". Characteristic are severe diffuse headache, vomiting attacks against the background of the absence of nausea and relief. General health quickly deteriorates. Severe conditions are accompanied by frequent changes in periods of excitement and apathy, convulsive attacks, the appearance of hallucinations and impaired consciousness, the development of stupor and comatose state.
The following are considered pathognomonic signs of ventriculitis:
- hyperesthesia (increased sensitivity);
- muscular-tonic symptoms;
- pain syndrome.
Increased sensitivity during the development of ventriculitis is an increase in sound, light, and tactile sensitivity. A pronounced muscular-tonic sign is rigidity of the occipital muscles (increased tone), which can be determined by passively tilting the head with an attempt to bring the patient's chin to the chest. The state of muscular hypertonicity can also be determined by the peculiar pose of the patient, who lies on his side, arching his back and throwing his head back, bending and tucking his legs to his stomach.
The pain syndrome affects the head, eyes, and is noted at the exit points of the trigeminal nerve, in the occipital region and cheekbones. [ 12 ]
Ventriculitis in newborns
Diagnosis and treatment of congenital anomalies of the central nervous system with the development of ventriculitis is a very important issue in medicine, since in recent years this pathology has become increasingly common. Purulent ventriculitis is a particularly severe intracranial complication caused by the entry of microflora into the cerebral ventricles. There is no characteristic CT picture for this pathology. It can be detected when an abscess breaks through into the ventricles, when a cerebrospinal fistula forms that communicates with the ventricles, or based on clinical and cerebrospinal fluid manifestations. [ 13 ]
The development of purulent meningoencephalitis and ventriculitis is possible with progressive internal occlusive hydrocephalus. The complication may manifest as a result of the ascending infection in the combination of a congenital defect of the central nervous system with an infected spinal hernia, or in isolated hydrocephalus with generalization of meningoencephalitis.
Characteristic clinical signs of hydrocephalus and ventriculitis are rapid growth of head circumference, spastic tetraparesis, vivid meningeal manifestations, prolonged stable hyperthermia. When coexisting with cerebrospinal hernias, the symptoms are supplemented by lower paraparesis, dysfunction of the pelvic organs with the presence of a tense hernial sac.
The course of the inflammatory process is usually severe, against the background of gross neurological insufficiency. Given the complexity of treatment, the degree of mortality, the severity of disability, an important point should be the improvement of preventive measures during pregnancy planning. It is important to perform qualified prenatal diagnostics and, if necessary, step-by-step treatment during the first months of the baby's life before complications and decompensated conditions appear. This is recommended to be done only in a specialized neurosurgical clinic or department.
Neurosonography is considered the most informative screening method for the morphological determination of brain lesions in children in the neonatal period. Neurosonography has the greatest diagnostic value in terms of identifying congenital anomalies of the central nervous system, internal hydrocephalus, periventricular hemorrhages and leukomalacia at the stage of cyst formation. [ 14 ]
Forms
The first information about the existence of ventriculitis was obtained almost a hundred years ago. It was published by an American, a specialist in pathohistology S. Nelson. A little earlier, assumptions were made about the belonging of granular ependymatitis to chronic lesions of the cerebral ependyma: the pathology, according to doctors, could develop as a complication of tuberculosis, syphilis, chronic alcohol intoxication, echinococcosis, senile dementia and other chronic pathologies of the central nervous system. The works of Dr. Kaufman, who believed that the primary factors in the development of the disease were traumatic and alcoholic lesions, acute infectious processes, were important.
Nelson's descriptions of the disease include an analysis of the chronic form of hydrocephalus. In particular, the doctor pointed out the difficulties in determining the etiology of granular ependymatitis, since the pathology can have both an inflammatory and non-inflammatory nature. [ 15 ]
Subsequently, other terms were used in medicine to characterize the disease - in particular, ependymatitis, ependymitis, intraventricular abscess, ventricular empyema and even the so-called "pyocephalus" are mentioned. After the assumption of the development of an inflammatory process inside the vessels, the term chorioependymatitis was introduced into medical use by Dr. A. Zinchenko (about fifty years ago). In addition, the following types of the disease were defined:
- nonspecific ventriculitis (allergic, infectious, viral, sinusogenic, tonsillogenic, rheumatic, otogenic, post-traumatic and intoxication pathology);
- specific ventriculitis (tuberculous, syphilitic, parasitic pathology).
The course of the disease was divided into acute, subacute and chronic stages.
According to the quality of cerebrospinal dynamics, the following types of pathology began to be distinguished:
- occlusive ventriculitis against the background of obliteration of the cerebrospinal fluid passages;
- non-occlusive ventriculitis in the phase of hypersecretion or hyposecretion (fibrosclerotic variant with hypotension).
Later, the name ependymatitis was hardly mentioned in medical circles. The term "ventriculitis" became much more widespread, and can develop in the following forms:
- primary form, caused by direct penetration of infection into the ventricular structures - for example, during penetrating injuries and wounds, surgical operations;
- secondary form, which occurs when pathogenic microorganisms enter from an existing focus in the body - for example, with meningoencephalitis, brain abscess.
Complications and consequences
As the inflammatory process in the ventricular system – ventriculitis – develops, pus enters the cerebrospinal fluid. As a result, the cerebrospinal fluid becomes more viscous, and its circulation is disrupted. The condition worsens if the cerebrospinal fluid ducts are clogged with accumulations of purulent masses. Intracranial pressure increases, brain structures are compressed, and cerebral edema develops.
When the inflammatory process spreads to the fourth ventricle, the cavity of the latter expands, and the developing hydrocephalus leads to compression of the adjacent brainstem. Vital centers localized in the medulla oblongata and the pons are affected. Increased pressure leads to respiratory and cardiovascular dysfunction, which significantly increases the risk of patient death. [ 16 ]
The most severe consequence of ventriculitis is death. In other cases, disability and dementia are possible.
Recovered patients may experience residual effects in the form of asthenia, emotional instability, chronic headaches, and intracranial hypertension.
Necessary conditions for successful treatment of patients with ventriculitis:
- timely and comprehensive diagnostic measures with adequate and competent therapy;
- individual and comprehensive approach;
- complete sanitation of the primary infectious focus. [ 17 ]
Diagnostics ventriculitis
The main diagnostic criterion for ventriculitis is a positive indicator of infection in the cerebrospinal fluid, or the presence of at least two characteristic symptoms of the disease:
- a febrile condition with a temperature exceeding 38°C, headaches, meningeal signs, or symptoms of affected cranial nerves;
- changes in the composition of cerebrospinal fluid (pleocytosis, increased protein content or decreased glucose content);
- the presence of microorganisms during microscopic examination of cerebrospinal fluid stained by Gram;
- isolation of microorganisms from blood;
- a positive diagnostic laboratory test of cerebrospinal fluid, blood, or urine without detection of culture (latex agglutination);
- diagnostic antibody titer (IgM or a fourfold increase in IgG titer in paired sera).
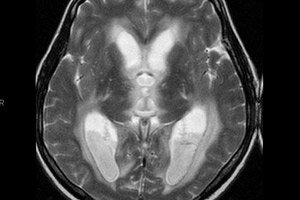
Of decisive diagnostic importance are the clinical and neurological characteristics of ventriculitis, as well as the results of laboratory tests. During computed tomography, a slight increase in the density of the cerebrospinal fluid can be determined, which is due to the presence of pus and detritus, as well as a periventricular decrease in density as a result of edema of the inflammatoryly altered ependyma from the subependymal layer. [ 18 ]
In many cases, the diagnosis of ventriculitis is confirmed by the detection of paraventricular localization of areas of brain destruction that communicate with the ventricular cavity, in combination with other symptoms. [ 19 ]
The optimal method for neurovisualization of ventriculitis is magnetic resonance imaging of the brain using DWI, FLAIR and T1-WI with contrast. Most often, it is possible to detect intraventricular detritus and pus, with predominant localization in the area of the occipital horns or triangles of the lateral ventricles, sometimes in the fourth ventricle during MRI diagnostics of a patient in a horizontal position. An additional MRI sign of ventriculitis is the presence of an enhanced contour of the ventricular lining (characteristic of 60% of cases). There are also signs of choroidal plexitis, including an unclear signal of blurring from the boundaries of the enlarged choroid plexus.
In early childhood, neurosonography is used as the main diagnostic method: the picture of ventriculitis is similar in signs to that seen in computed tomography or magnetic resonance imaging:
- increased echogenicity of the cerebrospinal fluid and detection of other echogenic inclusions due to the presence of pus and detritus;
- increased echogenicity and thickening of the ventricular walls (in particular, due to fibrin deposits);
- increased echogenicity of the choroid plexus, with blurring and deformation of the outlines. [ 20 ]
Tests include blood and cerebrospinal fluid tests:
- the glucose content in the cerebrospinal fluid is less than 40% of the glucose content in plasma (less than 2.2 mmol per liter);
- the protein content in the cerebrospinal fluid increases;
- microbiological cerebrospinal fluid culture is positive, or the pathogen is detected in a smear of cerebrospinal fluid (with Gram staining);
- cerebrospinal fluid cytosis is observed with a neutrophil level of 50% or higher of the total content;
- leukocytosis with a band shift is observed in the blood;
- plasma levels of C-reactive protein increase. [ 21 ]
The etiology of the disease is established by the cultural isolation of the pathogen during bacteriological seeding of cerebrospinal fluid and blood. It is imperative to take into account the duration and atypicality of the culture growth. Serological tests (RSK, RNGA, RA) involve the study of paired sera at two-week intervals. [ 22 ]
Instrumental diagnostics include computer or magnetic resonance imaging, neurosonography, and lumbar puncture. Encephalography is used to assess the functional state of the brain and the extent of damage to the nervous tissue. Electroneuromyography demonstrates the severity of damage to the conductive nerve pathways if the patient has paresis or paralysis.
Differential diagnosis
When an intraventricular hyperintensive signal is detected on MRI, differential diagnostics of ventriculitis with intraventricular hemorrhage is performed. Clinical practice shows that in relatively rare cases, a pathological hyperintensive signal is detected:
- in 85% of cases with FLAIR mode;
- in 60% in T1-VI mode with contrast;
- in 55% of cases – in DVI mode. [ 23 ]
It is important to take into account that areas of periventricular hyperintensity of a bordering type are also observed in patients with hydrocephalus, without infectious complications, which is associated with transependymal migration of cerebrospinal fluid and the formation of periventricular edema. [ 24 ]
Who to contact?
Treatment ventriculitis
The most important measure in the treatment of ventriculitis is antibiotic therapy. In order for such treatment to be as effective as possible, a set of medications is selected for the initial therapeutic stage, taking into account the presumed cause of the disease and microbiological indicators. The doctor determines the most appropriate dosage and frequency of antibiotic administration. [ 25 ]
Rational prescription of drugs involves determining the etiological factor of the disease and determining the sensitivity of the isolated culture of the microorganism to antibiotics. Bacteriological methods help to determine the pathogen after 2-3 days from the moment of collection of the material. The result of the sensitivity of microorganisms to antibacterial drugs can be assessed after another 24-36 hours. [ 26 ]
Antibacterial treatment of patients with ventriculitis should be started as early as possible, without wasting time waiting for the results of instrumental diagnostics and examination of cerebrospinal fluid, immediately after taking blood for sterility. Doses of antibiotics are established as the maximum permissible. [ 27 ]
Empirical treatment of ventriculitis necessarily involves the use of Vancomycin in combination with Cefepime or Ceftriaxone. If the patient is over 50 years old, or if the disease was preceded by an immunodeficiency state, Amikacin is prescribed as an adjuvant drug. [ 28 ]
An alternative regimen suitable for patients with severe allergic reactions to β-lactam antibiotics involves the use of Moxifloxacin or Ciprofloxacin in combination with Vancomycin. Patients over 50 years of age or suffering from immunodeficiency conditions additionally receive Trimethoprim/Sulfomethoxazole. [ 29 ]
Approximately 15 minutes before the first administration of the antibacterial drug, an injection of Dexamethasone should be given at a dosage of 0.15 mg per kilogram of body weight. If gram-positive diplococci are detected during microscopy of the cerebrospinal fluid sediment, or a positive latex agglutination reaction to pneumococci is detected in the blood or cerebrospinal fluid, then the administration of Dexamethasone is continued every 6 hours for 2-4 days, at the same dosage. In other situations, Dexamethasone should not be used. [ 30 ]
Ventriculitis may require additional intraventricular administration of antibacterial agents. Thus, Vancomycin, Colistin and aminoglycosides are considered safe and effective drugs for this purpose. Polymyxin B is considered the optimal option. The dosage is established empirically, taking into account the achievement of the required therapeutic content of the drug in the cerebrospinal fluid. [ 31 ]
Epidural administration of the following drugs is possible:
- Vancomycin 5-20 mg per day;
- Gentamicin 1-8 mg per day;
- Tobramycin 5-20 mg per day;
- Amikacin 5-50 mg per day;
- Polymyxin B 5 mg per day;
- Colistin 10 mg per day;
- Quinupristin or Dalfopristin 2-5 mg per day;
- Teicoplanin 5-40 mg per day.
Any β-lactam antibiotics, particularly penicillins, cephalosporins and carbapenems, are not suitable for subarachnoid administration because they increase seizure activity.
The combination of intravenous and intraventricular administration of antibiotics is always more preferable and effective. [ 32 ]
As the results of the study of cerebrospinal fluid and the resistance of microbial flora to antibiotic therapy are ready, the doctor corrects the antibacterial treatment, selecting a drug to which the microorganisms are particularly sensitive. [ 33 ]
The effect of antibiotic therapy is assessed according to clinical and laboratory indicators:
- weakening and disappearance of clinical symptoms;
- elimination of intoxication;
- stabilization of laboratory diagnostic indicators;
- "purity" of repeated cerebrospinal fluid cultures.
In addition to antibiotic therapy, patients with ventriculitis often undergo drainage of the cerebral ventricles to eliminate acute hydrocephalus, which occurs as a result of occlusion of the spinal canal by pus and detritus. It is important to carefully follow the rules of asepsis and antisepsis during the procedure, regularly change dressings, treat drainage areas, and ensure the cleanliness of connectors and containers for cerebrospinal fluid. [ 34 ]
The duration of treatment for patients is determined depending on the type of pathogen:
- at least two weeks for pneumococci;
- one week for group B streptococci;
- three weeks for enterobacteria.
During the treatment process, an assessment of clinical and laboratory effectiveness is performed.
If antibiotic therapy is ineffective, endoscopic surgery is recommended two weeks after the start of treatment to revise the ventricles, using an elastic endoscope and flushing the system with Ringer's solution or other similar drugs. Endoscopy can be repeated: the procedure is repeated if there is no positive dynamics within three weeks after the previous intervention. [ 35 ]
Throughout the entire period of a person's stay in the hospital, doctors monitor vital signs, maintain them at an optimal level with the help of constant and careful infusion of saline solutions. They also monitor the quality of diuresis. To prevent exhaustion, they provide parenteral nutrition and carry out hygienic care.
Additional symptomatic therapy for ventriculitis includes:
- correction of hypoxic conditions (artificial ventilation);
- anti-shock measures (corticosteroids, Heparin, Fraxeparin, Gordox, Contrycal);
- careful detoxification treatment (Infucol, Heisteril, fresh frozen plasma, albumin);
- dehydration and anti-edema treatment (Mannitol, 40% Sorbitol solution, Lasix);
- improving metabolic and neurovegetative protection of brain structures (Nootropil, Cavinton, Trental, Actovegin);
- compensation of energy costs (Moriamine, Polyamine, Lipofundin, etc.).
For pain relief, analgesics (including narcotic ones) and non-steroidal anti-inflammatory drugs are used.
Prevention
Modern neurosurgery involves the use of ventricular catheters, saturated with antibacterial agents (impregnation method), which helps to reduce the risk of infection during drainage. As practice shows, the use of such catheters simultaneously with careful adherence to other preventive measures helps to reduce the risk of infection to almost 0%. [ 36 ], [ 37 ], [ 38 ]
It is possible to prevent the development of ventriculitis. To do this, it is necessary to promptly treat otolaryngological and dental pathologies, avoid injuries and contact with infected people, strengthen the immune system, and avoid intoxication and stress. [ 39 ], [ 40 ]
Forecast
According to information published by specialists, the mortality rate in patients with post-drainage ventriculitis ranges from 30 to 40%. In patients of different ages who underwent neurosurgical operations with complications in the form of meningitis or ventriculitis, an unfavorable clinical prognosis was observed in almost 80% of cases, including:
- in more than 9% of cases, patient death was observed;
- in more than 14% of cases, persistent vegetative state developed;
- Almost 36% of patients developed severe pathological changes;
- In almost 20% of cases, moderate pathological changes were observed.
More than 20% of patients recovered well, 60% of children showed positive dynamics. The most unfavorable prognosis mostly related to people over 46 years old, showing a focal neurological picture, or demonstrating a level of consciousness less than 14 points according to the Glasgow Coma Scale. A poor prognosis was associated with cases in which there was a need for the procedure of artificial ventilation of the lungs.
In general, in patients with ventriculitis of various origins (including post-drainage and other development options), the mortality rate is about 5%. An extremely unfavorable prognosis is noted if ventriculitis occurs as a result of penetration of multiresistant microflora. For example, when affected by Acinetobacter baumannii, the mortality rate, even with systemic administration of Colistin, is more than 70%. The number of fatal cases in such a situation can be significantly reduced by supplementing systemic treatment with intraventricular use of Colistin.
The above indicators reflect prognostic data voiced by foreign authors. In the post-Soviet countries, such information is insufficient due to the lack of serious research on this issue. There is only a general statistical indicator of fatal outcomes in patients with ventriculitis, which is from 35 to 50% and higher.
It can be concluded that ventriculitis is a problem that requires comprehensive study. This is necessary both to prevent the development of pathology and for its successful treatment.

