
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Varicocele - Information Overview
Medical expert of the article
Last reviewed: 04.07.2025
Varicocele was first described by Celsius in the 1st century AD as "swollen and tortuous veins above the testicle, which becomes smaller than the opposite one." In 1889, WH Bennet established the relationship between changes in the scrotum and functional insufficiency of the testicle. He defined varicocele as "a pathological condition of the vein of the spermatic cord, arising, in most cases, as a result of or in combination with functional insufficiency of the testicle." It is the criterion of functional competence of the testicles that determines the interest of clinicians in this urological disease. This is due to the demographic situation observed in most developed countries. At least 40% of infertile marriages are due to male infertility. In this regard, the problem of varicocele, which affects up to 30% of men, is considered to be the cause of decreased fertility in 40-80% of cases, is becoming increasingly relevant.
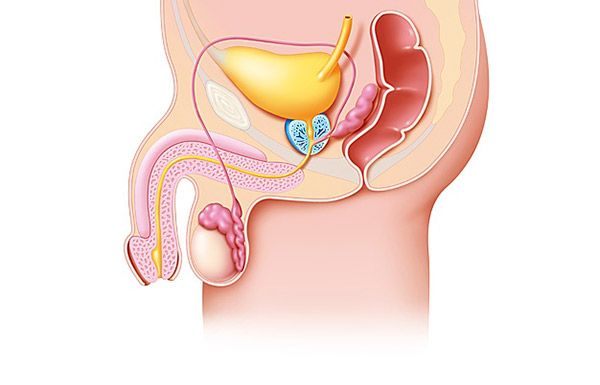
The ambiguity and contradictory nature of existing approaches and interpretations are noted already at the stage of terminological definition of the disease. Varicocele is a varicose (grape-shaped) expansion of the veins of the pampiniform (plexus pampiniformis) plexus of the spermatic cord, accompanied by intermittent or permanent venous reflux.
Epidemiology
Varicocele is one of the most common diseases among men, the frequency of which varies, according to different authors, from 2.3 to 30%. Having congenital predispositions to development, the incidence in different age groups is heterogeneous.
In preschool age, it does not exceed 0.12% and increases with growth and maturation. Varicocele is most often observed at the age of 15-30 years, as well as among athletes and physical workers.
Causes varicoceles
In 1918, O. Ivanissevich defined varicocele as "an anatomical and clinical syndrome, anatomically manifested by varicose veins inside the scrotum, and clinically - by venous reflux, for example, caused by valvular insufficiency." He saw the relationship between varicocele and insufficiency of the valves of the testicular vein, leading to retrograde blood flow through it. This was subsequently confirmed in connection with the introduction of vascular studies into clinical practice, allowing a visual assessment of the condition of the internal spermatic vein along its entire length. The defining concept today is that varicocele is considered not as an independent disease, but as a symptom of a developmental anomaly or disease of the inferior vena cava or renal veins.
Extreme variability of the structure of the venous system in general, as well as the left and right renal veins, is a consequence of impaired reduction of the cardinal and subcardinal veins. Retrograde blood flow is observed in congenital (primary) absence of valves in the testicular vein, as well as genetically determined weakness of the venous wall due to underdevelopment of the muscular layer, dysplasia of the connective tissue, leading to primary valvular insufficiency. Secondary valvular insufficiency develops as a result of venous hypertension in the system of the inferior vena cava and renal veins. In such cases, varicocele is considered as a bypass reno-caval anastomosis (through the internal and external spermatic veins into the common iliac), compensating for renal venous hypertension. Taking into account the anatomical features, which consist in the fact that the left testicular vein flows into the renal vein, and the right one in most cases directly into the inferior vena cava and only in 10% into the right renal vein, the structure of morbidity is dominated by left-sided varicocele - 80-86%, right-sided - 7-15%, bilateral - 1-6% of cases.
Any pathological conditions at the level of the scrotum, inguinal canal, abdominal cavity (hernia), renal and inferior vena cava, leading to compression of the spermatic cords, increased intra-abdominal pressure, pressure in the inferior vena cava and renal veins, which impedes the outflow of spermatic cord veins, are considered the cause of reflux blood flow and the development of varicocele.
The main causes of permanent increase of hydrodynamic pressure in the renal vein system and reno-testicular reflux are: renal vein stenosis, retroaortic location of the left renal vein, annular renal vein, arteriovenous fistula. Varicocele in such cases is determined both in ortho- and clinostasis, it exists since childhood and progresses. Particular attention is paid to the intermittent nature of reflux, often observed with aorto-mesenteric forceps, which is considered one of the causes of orthostatic varicocele. Sometimes this urological disease develops with tumors of the left kidney, abdominal cavity, compressing the main venous collectors, with a tendency to rapid progression as the tumor grows.
Pathogenesis
The role of pathogenetic factors leading to spermatogenesis disorders in varicocele has not been definitively established. These include:
- local hyperthermia;
- hypoxia;
- disruption of the hematotesticular barrier, including from the contralateral side due to collateral blood flow, leading to the production of antisperm antibodies;
- excess production of hydrocortisone in adrenal venous hypertension;
- disorders of the receptor apparatus and steroidogenesis;
- disturbances of the testicle-pituitary-hypothalamus feedback.
The role of local and general, relative and absolute androgen deficiency and other hormonal disorders is currently being studied. Recently, the influence of genetic factors leading to spermatogenesis disorders in varicocele has been studied. There is no direct correlation between the severity of varicocele and the degree of spermatogenesis disorders; the question of the influence of extrafunicular varicocele on spermatogenesis is being studied. Taking into account the anatomical and physiological features of the structure of the cremasteric vein and the superficial venous system of the testicle, there is no consensus on the pathogenetic significance for gametogenesis of the refluxing type of blood flow, sometimes observed normally in this vascular system.
Symptoms varicoceles
Symptoms of varicocele are unnoticeable. Sometimes patients note heaviness and pain in the left half of the scrotum, which must be differentiated from inflammatory diseases of the scrotum organs.
Forms
Depending on the nature of the phlebo-testicular relationship, Coolsaet distinguishes three hemodynamic types of reflux:
- reno-testicular:
- ileo-testicular;
- mixed.
There are a large number of classifications of varicocele based on the degree of severity.
Varicocele grades according to WHO (1997)
- Stage I varicocele - dilated veins protrude through the skin of the scrotum, are clearly visible. The testicle is reduced in size, has a doughy consistency.
- Stage II varicocele - dilated veins are not visible, but are easily palpated.
- Stage III varicocele - dilated veins are determined only by the Valsalva maneuver.
Asymptomatic varicocele is determined using a cough test or Doppler ultrasound of the scrotum using the Valsalva maneuver.
In domestic practice, the classification of Yu.F. Isakov (1977) is used, based on the reverse gradation of disease manifestations, in contrast to the WHO classification.
- Grade I varicocele is determined by palpation only with the Valsalva test (straining) in orthostasis.
- II degree - varicocele is clearly defined by palpation and visually. The testicle is unchanged.
- III degree pronounced dilatation of the veins of the pampiniform plexus. The testicle is reduced in size, has a doughy consistency.
Diagnostics varicoceles
Varicocele diagnostics is based on palpation, ultrasound and Doppler studies. Of the non-invasive methods, ultrasound combined with Doppler mapping of the renal vessels and testicular vein has the highest sensitivity. The study is performed in ortho- and clinostasis with mandatory assessment of the nature of changes (gradient) in blood flow (renal venous blood flow velocity, testicular reflux velocity and duration) during the Valsalva maneuver and transfer of the patient to the orthostatic position. Normally, the diameter of the testicular vein at the level of the scrotum is no more than 2 mm, the blood flow velocity does not exceed 10 cm/s, reflux is not detected. With subclinical varicocele, the diameter of the testicular vein increases to 3-4 mm, short-term (up to 3 s) reflux is detected during the Valsalva maneuver.
A further increase in reflux parameters corresponds to more pronounced stages of the pathological process. Performing a study using this technique allows in most cases to assume the hemodynamic type of varicocele, identify signs of renal venous hypertension and determine subclinical forms of the disease that are difficult to diagnose by palpation, which is considered a subjective method for assessing the condition of the spermatic cord and its elements. Urine is tested before and after physical activity. A positive march test (the appearance of microhematuria, proteinuria) indicates renal venous hypertension, a negative one does not exclude the presence of the latter, since the reno-caval shunt blood flow through the testicular vein system is sufficient to compensate for it. In such cases, the march test may become positive after ligation, clipping or embolization of the testicular vein due to worsening renal venous hypertension.
The ultrasound method has high sensitivity and is considered the main method in varicocele diagnostics, invasive radiological methods are also relevant and have the greatest clarity and information content. Antegrade phlebotesticulography and retrograde renal phlebography with retrograde phlebotesticulography and multiposition phlebotonometry are used in unclear cases and in diagnostics of recurrent forms of the disease. Sometimes dynamic nephroscintigraphy is performed to determine the functional state of the kidneys. Depending on the results of the examination, the type of surgical intervention is selected.
The diagnostics of varicocele has the following objectives:
- determination of the hemodynamic type of varicocele;
- assessment of the severity of renal venous hypertension, the nature and severity of venous reflux;
- study of the initial hormonal status and spermatogenesis.
A semiological study, MAR test, hormonal profile study (concentration of testosterone, estradiol, prolactin, follicle-stimulating hormone (FSH), luteinizing hormone (LH) are mandatory. Most patients are diagnosed with pathospermia of varying severity during a semiological study, consisting of a decrease in the concentration of actively motile forms of spermatozoa and an increase in the number of pathological forms. Oligospermia is noted in 60% of patients.
Formulations of the diagnosis of varicocele
Orthostatic left-sided varicocele, stage II, hemodynamic type I, oligoasthenozoospermia, infertile marriage.
Aortomesenteric forceps, intermittent renal venous hypertension, orthostatic left-sided varicocele, stage III, hemodynamic type I, asthenoteratozoospermia, infertile marriage.
What do need to examine?
Who to contact?
Treatment varicoceles
Non-drug treatment of varicocele
There is no conservative treatment for varicocele.
Drug treatment of varicocele
Drug treatment of varicocele is used in the postoperative period to stimulate spermatogenesis. It includes vitamins, biologically active food supplements (containing selenium and zinc) and hormonal drugs (androgens, human chorionic gonadotropin), prescribed according to strict indications in courses under strict laboratory control.
Varicocele surgery
Today, approximately 120 types of operations are used for varicocele. Some of them are of historical significance only. The currently used procedures are divided into two groups.
Group I - preserving renocaval shunt. These include shunting operations: proximal testicular-iliac and proximal testicular-saphenous vascular anastomoses. Performing bidirectional anastomoses is considered inappropriate.
Group II - not preserving the renocaval shunt.
- Suprainguinal non-selective.
- Operation A. Palomo (1949) - the internal spermatic vein is ligated together with all accompanying vascular structures.
- Operation by A.P. Erokhin (1979) ligation of the internal spermatic vein and artery with preservation of the lymphatic vessels, for better visualization of which a solution of indigo carmine is introduced under the protein coat of the testicle.
- Operation Bernardi, Kondakov and other manuals.
- Suprainguinal selective.
- Operation O. Ivanissevich (1918).
- High ligation of the testicular vein.
- Operation Speriongano (1999) - ligation of veins at the internal ring of the inguinal canal under the control of intraoperative color Doppler sonography.
- Subinguinal selective.
- Subinguinal ligation of the testicular vein (microsurgical method).
Giving preference to reconstructive vascular and selective supra- and subinguinal interventions, it is advisable to use optical magnification and precision technology. Performing surgical intervention using microsurgical technology allows, on the one hand, to reduce the number of relapses due to increased effectiveness of the intervention, and on the other hand, to reduce the number of complications associated with difficult differentiation of elements of the spermatic cord and vascular structures accompanying the internal spermatic vein.
The most common operation is the Ivanissevich operation. Ligation and transection of the left testicular vein interrupts the reverse blood flow from the renal vein to the pampiniform plexus, thereby eliminating varicose veins.
However, during this operation, which eliminates varicocele, the bypass venous renocaval anastomosis undergoes changes, which developed compensatorily due to the difficulty of venous outflow from the kidney. Considering that the cause of varicocele is not only reflux along the testicular vein, but also increased arterial blood flow to the testicle through the testicular artery. A. Palomo (1949) proposed to ligate the artery along with the vein. During this operation, the testicular vein is ligated together with the testicular artery accompanying it in the form of a thin tortuous trunk. It has been proven that ligation of the testicular artery does not cause a disruption in the blood supply to the testicle and its atrophy, provided that the arterial flow to it through the external spermatic artery and the artery of the vas deferens is preserved. It has been established that with ligation of the testicular artery, spermatogenesis is restored more slowly.
The introduction of 0.5 ml of a 0.4% indigo carmine solution under the protein coat of the testicle before surgery allows for a good view of the proximal lymphatic pathways of the vascular bundle of the left testicle during surgery in children and avoids their accidental ligation along with the artery and vein.
Varicocele recurrence occurs when a thin venous trunk, accompanying the main one, remains untied during surgery. The persistent reverse blood flow through this vein quickly transforms it into a wide trunk. Hydrocele of the testicular membranes that appears after surgery (in 7% of cases) develops as a result of blockage of lymphatic outflow from the testicle.
Laparoscopic testicular vein clipping
Laparoscopic varicoectomy is considered a minimally invasive endoscopic analogue of open suprainguinal interventions. Contraindications include several previous surgeries on abdominal organs. One of the important advantages is the possibility of performing laparoscopic clipping of veins in case of bilateral lesions. The length of hospital stay is from 1 to 3 days.
To identify the lymphatic vessels, methylthioninium chloride must be injected under the tunica albuginea of the testicle and the artery and lymphatic vessels must be carefully separated, which is considered a preventative measure for relapse.
According to I.V. Podtsubny et al., the advantage of laparoscopic occlusion of testicular veins compared to angioembolization is more promising and economically beneficial.
Technique of laparoscopic occlusion of the testicular vein. The operation is performed under endotracheal anesthesia. After applying carboxyperitoneum at point #1 near the navel, a 5-mm trocar is inserted and the abdominal cavity is inspected using a 5-mm laparoscope. Adhesions with the sigmoid colon are often detected during the operation and are separated. The testicular vessels are detected. In case of adhesions, the testicular vessels are visualized on the left less clearly than on the right. A Valsalva maneuver is performed (compression of the testicle by hand - the testicle is pulled down by a doctor not participating in the operation), after which the vessels are detected more clearly. 5-8 ml of a 0.5% procaine solution is injected into the retroperitoneal space. A transverse incision is made over the vessels, 1.5-3.0 cm long. The artery is separated from the veins, after which they are clipped and transected. The magnification of the laparoscope allows the lymphatic vessels to be seen and left intact. Carefully check whether all the veins have been transected, as sometimes a vein is found that is very close to the artery and difficult to distinguish.
This is why the artery at the level of the intersected veins is carefully and cautiously examined. The Valsalva maneuver is repeated to confirm the absence of bleeding. After revision of the abdominal cavity, desufflation is performed and 5-mm trocars are removed. Only the skin is sutured. Performing a laparoscopic operation with clipping of the testicular veins has advantages over open surgery.
Taking into account the above, it should be concluded that, along with a wide range of surgical interventions proposed for the treatment of varicocele, laparoscopic surgery performed according to strict indications is considered a worthy alternative.
Eudovascular phlebosclerosis
Performed simultaneously with phlebography and phlebotonometry, indicated when type 1 hemodynamic varicocele is detected, in the absence of organic disease (stenosis, retroaortic location of the renal vein) and renal venous hypertension.
Endovascular obliteration of the testicular vein is an alternative to surgery in children and adults. Various materials are used for endovascular occlusion: spiral emboli, tissue glue, wire umbrella devices, detachable balloons, sclerotherapy preparations, etc. Catheterization of the femoral vein is performed according to Seldinger. After superselective probing of the testicular vein, one of the thrombosing agents (8-15 ml) is injected into it, 5-8 cm from the mouth of the testicular vein. The absence of contrast in the testicular vein at the level of the iliac crest 30 minutes after the introduction of the sclerosing agent indicates thrombosis of the vessel.
The primary importance is the direct contact of the thrombosing agent with the patient's blood. Thrombosis occurs at the thrombosing agent-blood interface. Some authors recommend providing a relatively motionless interface between the thrombosing agent and blood for 2-3 minutes and not filling the entire testicular vein with the thrombosing agent solution. Thrombosis ends on average in 20-25 minutes.
This method is contraindicated in case of loose veins. Disadvantages of the method: possibility of recanalization and penetration of sclerosing substances into the general bloodstream, phlebitis of the pampiniform plexus. To exclude the latter complication, it is recommended to carefully squeeze the spermatic cord at the entrance to the scrotum with your hand during the introduction of the thrombosing agent.
Absolute contraindications to endovascular occlusion in children:
- diagnosis of large diameter testicular and testicular renal collaterals, through which the sclerosing agent may be dislocated into the central veins, which leads to its entry into the systemic bloodstream;
- absence of occlusion of the trunk of the testicular vein distal to these collaterals;
- absence of phlebographic signs of renal-testicular reflux, which may be due to either the absence of varicocele or abnormal entry of the left testicular vein into the inferior vena cava, lumbar veins, etc.;
- diagnosis of a single trunk of the testicular vein, accompanied by pronounced signs of renal venous hypertension, hematuria and proteinuria in combination with a single trunk and agenesis of the right kidney.
Advantages of the method of endovascular percutaneous transfemoral sclerotherapy of the left testicular vein:
- the manipulation is performed under local anesthesia;
- the hospital stay is reduced to 2-3 days;
- the method allows to avoid surgical intervention;
- the sclerosing drug causes thrombosis of not only the 1st trunk of the testicular vein, but also small anastomoses;
- embolization allows to avoid lymphostasis and hydrocele;
- Repeated embolization is possible if the disease recurs.
Each of the listed methods of the second group has its advantages and disadvantages, and their use is largely motivated by the individual preferences of the urologist. The choice between the interventions of the first and second groups is considered fundamental.
Varicocele of the 1st hemodynamic type with organic narrowing of the renal vein, permanent or intermittent renal venous hypertension with a high orthostatic or functional (Valsalva test) pressure gradient and other parameters of renotesticular reflux is an indication for performing group 1 shunt operations.
Thus, the predominant hemodynamic type of varicocele is considered to be renotesticular reflux, surgical treatment is the only method of treating this disease. The type of surgical intervention is determined by the hemodynamic type of varicocele, the presence of renal venous hypertension and the nature of phlebotesticular reflux. Surgery must be undertaken when the disease has been identified.
Forecast
According to various authors, relapse of the disease is observed in 2-30% of cases. On average, relapses occur in 10% of operated patients and are associated not only with defects in surgical technique, but also with an erroneous determination of the hemodynamic type of varicocele. In 90% of patients, improvement in spermatogenesis indicators is observed, but only in 45% of cases the indicators approached the norm. The longer the disease and the older the age group of operated patients, the lower this indicator and the longer the recovery period (up to 5-10 cycles).


 [
[