
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
trigeminal neuritis
Medical expert of the article
Last reviewed: 04.07.2025
True neuritis, according to research, is actually a rare phenomenon, even post-infectious lesions are more related to neuroallergic ones. A more correct and modern name for the pathology is the term "neuropathy", which is increasingly used at present, since the mechanism of the disease development and the presence of an inflammatory process are usually not precisely established. However, the final verdict on the terms "neuritis - neuropathy" has not been made, so the name "neuritis of the trigeminal nerve" is still quite common as a diagnosis of its damage.
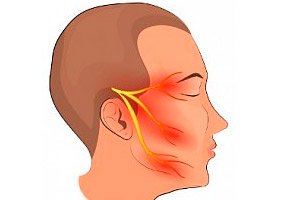
A little anatomy: the trigeminal nerve is also called mixed, since it has sensory and motor nerve fibers. Its three main branches (ophthalmic, maxillary and mandibular) emerge from the trigeminal ganglion, located in the temporal region, and are directed, dividing into increasingly smaller branches, to the sensory receptors of the skin, mucous membranes, muscles and other anatomical structures of the anterior upper third of the head and face. The ophthalmic and maxillary nerves contain only sensory fibers, the mandibular nerve also contains motor fibers, ensuring the movement of the chewing muscles of the same name. Trigeminal neuritis is an inflammation of one or more peripheral processes of its branches, that is, external ones, located outside the brain, manifested by excruciating pain that disrupts the rhythm of life, and sometimes is disabling, a violation of autonomic innervation with loss of sensitivity of the affected area, paresis, structural changes in nerve fibers.
Epidemiology
Morbidity statistics classify trigeminal nerve damage as a fairly common pathology - from 40 to 50 people out of 100 thousand people suffer from trigeminal neuralgia, among them there are two women for every man. Among neuralgias, it dominates. Every year, from two to five people out of every ten thousand inhabitants of the planet seek medical help for the first time with complaints of pain along the trigeminal nerve.
Secondary pathology accounts for about 4/5 of all cases, the main contingent of patients are over 50 years of age. [ 1 ]
Causes trigeminal neuritis
The term "neuritis" indicates that there is inflammation of the nerve fibers, they already have anatomical changes in the myelin layer, connective tissue (interstitium), axial cylinders (nerve cell processes). Infectious agents - viruses, bacteria, fungi - usually play the main role in the development of the inflammatory process. Each of us has acute infectious diseases, and almost everyone has latent chronic infections (caries, tonsillitis, sinusitis, herpes, etc.). Inflammation of the trigeminal nerve can occur as a secondary process after an acute disease or exacerbation of a chronic infection. But most often there is herpetic ganglioneuritis, the cause of which is (presumably) irritation of the neurons of the Gasserian ganglion affected by the herpes virus.
However, much more often, pain along the nerve is caused by inflammatory and destructive processes not so much in the tissues of the nerve fibers, but in the anatomical structures located next to it. The cause of pain is then the compression and irritation of the nerve fibers by nearby altered vessels and tumors, injuries and congenital pathologies of the cranial structures, which over time lead to the appearance of degenerative-dystrophic changes in the nerve (neuropathy). [ 2 ]
Traumatic neuritis of the peripheral parts of the trigeminal nerve is quite common. The risk factors for its occurrence are quite banal. Direct trauma to the nerve and surrounding tissues can occur not only with accidental fractures of the facial bones of the skull, but also in the dentist's office. Violation of the integrity of nerve fibers can be a consequence of complex tooth extractions, the penetration of filling material beyond the root of the tooth during canal filling, surgical manipulations, anesthesia, prosthetics.
Risk factors
Risk factors for compression of the trigeminal nerve are anatomical anomalies related to the canals, openings, and vessels along its branches; cysts, benign and malignant neoplasms; injuries; metabolic disorders caused by digestive disorders, endocrine and cardiovascular pathologies; multiple sclerosis or atherosclerosis of the cerebral arteries with plaque formation localized at the entrance of the trigeminal nerve root, hemorrhage in the brainstem basin.
Sometimes attacks of specific pain, the so-called pain tic, are preceded by severe hypothermia and a common cold.
Long-term neuralgia may be a symptom of nerve inflammation. In advanced cases, with structural disorders and loss of sensitivity, we speak of the neuritic stage of neuralgia.
If the diagnostic examination does not reveal any diseases, trigeminal neuralgia is considered an essential or primary, independent disease. If vascular pathology, tumor, metabolic disorders, inflammatory process or trauma are detected, then the nerve damage is interpreted as secondary (symptomatic).
Neuritis of smaller peripheral branches of the trigeminal - alveolar nerves are more common than inflammatory lesions of the main branches. They can be provoked by infectious diseases, such as osteomyelitis, and colds, accidental injuries to the jaw bones, and are also often a consequence of dental interventions.
The inferior alveolar nerve can be damaged during the extraction of the third lower molars, during the treatment of pulpitis of the premolars and molars of the lower jaw (during the canal filling, an excessive amount of filling material can get behind the apex of the tooth), sometimes the nerve is damaged during conduction anesthesia. The superior one is damaged as a result of chronic sinusitis and surgical interventions for them, periodontal inflammation, pulpitis, prosthetics, anesthesia, blockades, tooth extraction (the alveolar branches that innervate the canines and second premolars are most often damaged), etc. Impaired sensitivity of the superior alveolar nerves is difficult to treat, which takes several months, and sometimes it cannot be restored at all.
Complex extractions of teeth in the upper jaw can lead to neuritis of the anterior palatine process of the nerve, and in the lower jaw – to neuropathy of the lingual or buccal nerve.
Pathogenesis
The pathogenesis of neuritis is multifactorial. The integrity of nerve structures is affected not only by the direct mechanical damaging factor, but also by intoxication, metabolic disorders, and vascular transformations. And if everything is clear with traumatic lesions of the branches of the trigeminal nerve, then other theories are still hypothetical. There are several assumptions about its nature, based on clinical data, but not reliably confirmed. One of the most common versions is the hypothesis that damage to one of the branches of the nerve in a certain area leads to local damage to the myelin sheaths. Nerve fibers are "exposed", generating ectopic excitation waves (impulses) in this place, provoking attacks of pain (peripheral theory). A long-term situation leads to deeper damage, the formation of a pain focus and sensitivity disorders.
Another hypothesis, based on the fact that the drug of choice for the treatment of neuralgia is the anticonvulsant carbamazepine, considers the central origin of pain and neuralgia itself as a disease similar to partial epilepsy.
Symptoms trigeminal neuritis
Symptoms of trigeminal neuritis include pain of varying intensity, often not as acute as with pure neuralgia, but aching. They can be paroxysmal and constant. There is always a weakening or loss of sensitivity in the affected areas, and if the motor fibers of the third branch are affected, there are also motor disorders.
Pain in trigeminal neuritis is felt in the vast majority of cases on one side, right-sided damage is 2.5 times more common, although the nerve is paired, located symmetrically on the left and right. Bilateral pain is not typical, but such a case cannot be ruled out. Sometimes patients complain that the pain impulse is given to the index finger of the left hand. Basically, one branch of the trigeminal nerve is affected - pain is felt in the area of its autonomic innervation, both deep and superficial sensitivity can be impaired.
At the peak of an attack of pain, some patients notice contractions of the facial muscles (tic) or chewing muscles (trismus).
Neuritis of the first branch of the trigeminal nerve, the ophthalmic one, is much less common than that of the other two branches. It emerges from the temporal ganglion upwards, is located in the thickness of the lateral wall of the cavernous sinus (above the eyebrows) and enters the orbit, having previously bifurcated into the ophthalmic branch itself and the tentorial branch, which goes back to the tentorium cerebelli. In the orbit, part of the nerve divides into three more branches: the frontal, lacrimal and nasociliary, which branch further. The first branch of the trigeminal nerve innervates the skin of the forehead and approximately 1/3 of the frontal surface of the head under the hairline, the corresponding meninges, the skin and mucous membrane of the upper eyelid, the eyeball, lacrimal glands, the top of the bridge of the nose and the mucous membrane of the "ceiling" of the nasal passage, the frontal and ethmoid sinuses. Pain syndrome occurs along the branch at any point of innervation where the nerve is affected. Depending on the location of the lesion, the upper part of the head to the crown and face, the area of the eyes, the back and nasal cavity may hurt. Additionally, there may be lacrimation, mucus discharge from the nose, loss of smell and a feeling of numbness. The patient may have impaired reflexive closure of the eyelids: when hitting the inner edge of the superciliary arch with a hammer (orbicular reflex) and/or when touching the surface of the cornea (corneal reflex). [ 3 ]
Neuritis of the second branch of the trigeminal nerve, the maxillary, is felt as pain in the triangular part of the cheek located under the eye. The apices of the conditional triangle of pain localization are located in the temple area, the upper part of the wing of the nose, under the middle of the upper lip. The branches of this nerve are numerous, the largest are meningeal, infraorbital and zygomatic, which in turn are divided into smaller branches that provide innervation of the dura mater in the area of the middle cranial fossa, the outer corner of the eye, the skin and mucous membranes of the lower eyelid, nose, maxillary sinus, the upper part of the cheek in the above area, the upper lip, jaw and teeth. The external exit of the second branch of the trigeminal nerve is the infraorbital canal. The maxillary branch is affected most often. Pain and hypoesthesia (paresthesia) may be accompanied by lacrimation, nasal discharge, salivation.
Neuritis of the lower branch of the trigeminal nerve manifests itself as pain localized from the temples along the back of the face, the lower part of the cheek and the frontal part - the chin. Pain can be felt in the ear, tongue and lower jaw. This branch exits the cranium through the mental opening of the lower jaw, exits under the fourth and fifth lower teeth from the center. The lower (third) branch contains both sensory nerve fibers that innervate the surface of the skin of the back side of the face, the bottom of the cheek and the front part of the chin, the corresponding mucous membranes, structures of the lower jaw (gums, teeth), two-thirds of the tongue from its tip, and motor fibers that innervate the masticatory muscles, the defeat of which causes its partial paralysis. It manifests itself in weakened muscle tension when performing chewing movements, asymmetry of the facial oval, drooping of the lower jaw on one side, and a violation of the chin reflex - the reflex closure of the lips when hitting the chin with a hammer. With paresis (paralysis) of the temporal muscle, a visually noticeable depression of the temporal fossa. [ 4 ]
In addition to neuropathies of the three main branches of the trigeminal nerve, lesions of its smaller branches innervating the teeth, and inflammation of the alveolar nerves, both lower and upper, are of clinical significance. The main clinical manifestations of their lesions are pain and a decrease (complete absence) of all types of sensitivity in the corresponding gum, adjacent mucous membrane of the cheek, and lip. Electrical excitability of the dental pulp in the affected area is noticeably reduced or completely absent. In the acute stage, paresis and trismus of the masticatory muscles on the affected side may be observed.
Neuritis of the mental nerve, the terminal branch of the inferior alveolar nerve, is observed quite rarely. The area of localization of sensitivity disorder covers the lower lip and chin.
Neuritis of the lingual nerve has practical significance. Impaired sensations (reduced tactile and absence of pain sensitivity, burning, tingling, pain) are localized in the area of the anterior two-thirds of the corresponding half of the tongue. It can be either isolated or combined with neuropathy of the inferior alveolar process of the nerve.
Neuritis of the buccal nerve occurs without pain, only hypo- or anesthesia is observed in the area of the inner side of the cheek and the corresponding corner of the mouth. Isolated lesions are almost never encountered, as a rule, the lower alveolar process of the nerve is also affected.
Herpetic neuritis of the trigeminal nerve develops with lesions of the trigeminal (Gasserov, trigeminal) ganglion by the herpes simplex virus type 1, as well as Varicella zoster. Ganglioneuritis - a lesion of the nerve cells of the trigeminal ganglion (node) manifests itself with acute pain and a characteristic herpetic rash in the innervation zone, more often of one branch of the trigeminal nerve, much less often - all at once. This is accompanied by swelling of the affected side of the face and pain localized at three points of exit of the trigeminal nerve.
If the herpes virus has spread to the maxillary or mandibular branch, then during the period of exacerbation the herpetic rash appears not only on the surface of the skin of the face, but also inside, on the mucous membranes of the corresponding half of the hard and soft palate, the soft palate, gums and cheeks. The mucous membrane of the nasal passage can often be free of rashes, but this is not necessary. The branches that provide innervation of the mucous membranes can be affected to a greater extent than the skin. Then the rash is more abundant on the internal surfaces. It can also be the other way around.
The ocular form of trigeminal ganglioneuritis is distinguished (4% of all cases) - the infection spreads to the first branch of the trigeminal nerve. The manifestation of this direction is herpetic conjunctivitis and keratitis, usually with ulceration. Hutchinson's symptom, when herpetic vesicles are observed on the wings or tip of the nose, indicates the development of complications - inflammation of the cornea of the eye, its iris, episclera or optic nerve with its subsequent atrophy.
Pain in the area of innervation of all branches at once can also indicate damage to the sensory roots of the trigeminal nerve at the entrance to the brain stem.
Forms
There is no specific classification of trigeminal neuritis. Peripheral lesions are distinguished when sensitivity, deep or superficial, is impaired along one branch or smaller branches (neuritis of the alveolar nerves). It is also called typical.
And total (atypical), when the whole half of the head and neck hurt. Bilateral pathology is diagnosed extremely rarely.
The localization and nature of pain in each patient has individual characteristics, since the location of the branches may differ in different people. In addition, the innervation zones of the branches of the trigeminal nerve overlap one another.
According to the origin of the pathology, an independent disease is distinguished - essential neuralgia (primary, idiopathic), when the cause of the pain cannot be determined, and symptomatic (secondary).
Complications and consequences
The neuritic stage of neuralgia is already a complication in itself, since pain attacks are accompanied by loss of sensitivity and paresis, indicating damage to the nerve fibers.
In addition, a patient who has been experiencing pain for a long time, trying to avoid an attack, develops the so-called protective type of behavior. For example, he chews food mainly with the healthy part of the mouth, avoids making certain movements, taking poses, because of this the muscles on the sore side suffer, and degenerative changes occur in it over time.
Against the background of such behavior, not only physical changes appear, but also mental pathologies - a phobia often develops. The patient, constantly expecting an attack, becomes anxious and irritable, often prefers voluntary isolation, which leads to the progression of a mental disorder.
Complications are possible from nearby vessels (trophic disorders), facial, optic and auditory nerves. The disease becomes chronic, and it is already problematic to cure it completely. The consequence of late seeking help may be partial paralysis of the facial muscles, for example, drooping of the corner of the mouth or eyelid on the affected side (ptosis), impoverishment of facial expressions, incoordination of the movements of various groups of facial muscles (ataxia); decreased vision and/or hearing.
With prolonged course of trigeminal neuritis, it can be complicated by cerebellar hematoma.
Although the disease does not pose an immediate threat to life, its quality suffers greatly.
Diagnostics trigeminal neuritis
Complaints of intense facial pain, loss of sensitivity and jaw muscle dysfunction require a comprehensive examination of the patient. In addition to a physical examination and interview, the doctor prescribes a clinical and biochemical blood test, tests for the detection of the herpes virus. Typically, this is a polymerase chain reaction, enzyme immunoassay or immunofluorescence reaction. Depending on the suspected underlying disease, tests for blood glucose levels, autoantibody levels, etc. may be prescribed.
The patient is necessarily examined for the presence of odontogenic diseases, pathologies of the visual and ENT organs, and a consultation with a neurosurgeon, maxillofacial surgeon and other specialists is prescribed as necessary.
Classical instrumental diagnostics – radiography and magnetic resonance imaging as the most informative methods for visualizing bone structures and soft tissues. Additional studies may include electroencephalography, electroneuromyography, computed tomography, ultrasound, spinal puncture, and other studies depending on the suspected etiological factor of neuritis. [ 5 ]
Differential diagnosis
Differential diagnostics are carried out with glaucoma (with this disease, acute pain is felt in the innervation zone of the ophthalmic branch of the trigeminal nerve); sinusitis; maxillary sinusitis; calculous formations in the salivary glands; subluxation of the temporomandibular joint; neoplasms in the trigeminal ganglion zone and along the nerve branches; temporal tendinitis; trigeminisms - reflected pain in diseases of internal organs; pathological processes affecting the teeth and jaw.
Neuritis and trigeminal neuralgia are components of the same process. When they talk about "pure" neuralgia, they mean acute paroxysmal pain of neurogenic origin, not relieved by available painkillers. Pain paroxysms are usually short, from a few seconds to two minutes, with a clear beginning and end. In the period between them, called refractory, the patient feels as usual, there are no neurological symptoms. Typical attacks of pain occur suddenly and are repeated frequently (30-40 times a day), sometimes not allowing the patient to come to his senses. An attack of pain is often provoked by irritation of the affected area (trigger factor) - chewing, coughing, palpation, change in ambient temperature, for example, the patient comes from the winter street into a warm room. Such pains are called "trigger pains". In addition, an attack of trigeminal neuralgia in some people occurs as a result of strong anxiety, stress, consumption of stimulating foods and drinks: spicy foods, alcohol, coffee, and other stimulants of the nervous system.
The most typical trigger (algogenic) zones are the area above the eyebrow, at the inner corner of the eye, on the bridge and under the nose, the outer point of the wing of the nose, the corner of the mouth, the inner surface of the cheek, and the gums. A slight touch on one of these areas can cause an attack of pain. Typically, a sharp and strong irritation of the trigger zone can lead to the cessation of the pain attack. The acute period can be accompanied by hypersalivation, increased sweating, nasal discharge, and lacrimation. It is comforting that at night during sleep, trigeminal neuralgia usually does not bother, but many cannot sleep on the sore side.
Specific behavioral features are observed in people with trigeminal neuralgia - during an attack, the patient freezes silently, often putting his hand to and rubbing the sore area of the face. At the same time, he does not scream, does not complain, does not cry, although the pain is very sharp and excruciating. He is approachable. He answers questions in monosyllables.
Neuralgia - pain along the nerve can be a manifestation of an inflammatory process in the nervous tissue, the presence of changes in the structure of the nerve trunk. Then they talk about neuritis. Inflammation of the nerve is clinically manifested not only by pain, but also by symptoms of dysfunction - a decrease in muscle volume, decreased muscle strength, hypoesthesia or anesthesia, decreased or lost reflexes. The nature of pain in the neuritic stage also changes, it becomes aching and often constant. This indicates the neglect of the process and the upcoming difficulties of treatment.
Who to contact?
Treatment trigeminal neuritis
Treatment of trigeminal neuritis is complex. Sanitation of the oral cavity and elimination of inflammation in the nasal cavities, if detected, are mandatory, and any somatic pathologies are corrected if present. Direct treatment is reduced to eliminating attacks of pain and preventing their relapses, and, if possible, restoring sensitivity and the structure of nerve fibers. [ 6 ]
In case of damage to the trigeminal ganglion and the main branches of the trigeminal nerve, the analgesic effect is provided by anticonvulsants. The drug of choice is carbamazepine. The effect of its use occurs in 70% of patients suffering from trigeminal neuralgia. The pain usually disappears on the second or third day from the start of taking the drug. Carbamazepine is started with low doses. On the first day, a double dose of 100 to 200 mg is prescribed. Every day, the patient takes 100 mg more of the drug. The daily dose is increased until the pain disappears due to more frequent administration of the drug. The maximum the patient takes per day is three or four times 200 mg. After achieving pain relief, the dose of the drug is gradually reduced by 100 mg per day, stopping at the minimum effective. The course of treatment is on average three to four weeks.
Some patients are helped by valproic acid. Treatment begins with a daily dose of 3 to 15 mg, divided into two doses. It is assumed that the dose can be increased by 5-10 mg per kilogram of the patient's weight per week, but not more than 3 g per day.
Second-line drugs include centrally acting muscle relaxants baclofen and tizanidine, and antidepressants such as amitriptyline.
Doses of muscle relaxants are selected empirically so that muscle tone does not decrease to the point of motor disorders. Baclofen is started at 2-5 mg three times a day, gradually increasing the dose every three days to the minimum effective dose. The daily dose should not exceed 60-75 mg. Baclofen is discontinued, also gradually reducing the dose.
Tizanidine is started with one capsule per day, as a rule, two capsules are enough to relieve pain. The dose is increased every three to seven days. In some cases, four capsules are required.
Amitriptyline is initially taken at 25-50 mg before bedtime, with a subsequent increase in the frequency of administration to three and the dose of the drug itself over five to six days up to 150 mg, and if the therapeutic effect does not occur within two weeks, then the dose is increased to 300 mg / day, with most of it taken before bedtime. After the pain stops, gradually return to the original maintenance dosage. Treatment can be long-term, but not more than eight months.
In severe cases, during hospital treatment, anticonvulsants, muscle relaxants, and antidepressants may be prescribed intravenously or by drip.
In case of bacterial infections (sinusitis, maxillary sinusitis, osteomyelitis, dental infections), intravenous infusions of hecamethylenetetramine, which has the necessary spectrum of antibacterial activity, are recommended.
Antihistamines are also prescribed, preferably also providing sedation (diphenhydramine, suprastin). They enhance the effect of painkillers and antidepressants. Biotonic agents are prescribed - aloe extract, in case of severe muscle atrophy - adenosine triphosphoric acid, alcohol-novocaine blockades, other drugs according to the symptoms.
In case of relapses of trigeminal neuralgia, single drip injections of phenytoin give a good effect. The dose of the drug is calculated in proportion of 15 mg per kilogram of the patient's weight. The procedure takes two hours.
Non-narcotic analgesics do not have the expected effect, except in cases of neurostomatological neuritis (damage to the alveolar nerves). Moreover, the desire to quickly relieve a pain attack with a large dose of the drug can lead to the development of such a side effect as drug abuse syndrome. This applies to taking pills. And local use of a drug of the same group, dimethyl sulfoxide, better known as dimexide, for trigeminal neuritis has proven effective. The treatment method is very simple and can be done at home. And in comparison with the above-mentioned drugs, it is also absolutely safe, since the side effects with local use are minimal.
Compresses with dimexide for trigeminal nerve neuritis are made on the skin of the face at the points where the affected branches exit - simply apply a napkin soaked in a solution prepared from a mixture of dimexide with lidocaine or novocaine to this area for 20-30 minutes.
So, to make a solution for a compress, you need to buy a bottle of a standard 98% solution of dimethyl sulfoxide and a 2% solution of any anesthetic - lidocaine or novocaine - from a pharmacy. Before starting treatment, you need to test for sensitivity to each of the ingredients: moisten a tampon with the solution and apply it to the skin. The appearance of a rash, redness and itching at the site of application will indicate the impossibility of using this method. In addition, dimexide is a pronounced conductor. Already five minutes after the start of the application, it is detected in the blood serum. Therefore, pregnant women, people with glaucoma and cataracts, severe liver, kidney, heart dysfunction, vascular pathologies should refrain from treatment with compresses with dimexide. In general, it is better to consult with your doctor before treatment. [ 7 ]
If there are no contraindications, prepare a solution, that is, mix dimexide with any of the anesthetics in the following ratios: 1:9 (one part dimexide to nine parts anesthetic) or 1:5 or 3:10. Choose the ratio of ingredients depending on the severity of the pain syndrome - the stronger the pain, the more concentrated the solution. Take a gauze napkin, dip it in the prepared solution and squeeze it out, not dry, but so that it does not flow. Apply to the point of exit of the affected branch to the surface of the face: the first is the supraorbital notch, located directly above the eyebrow about a centimeter from its beginning; the second is the infraorbital canal; the third is the mental opening of the lower jaw, located under the fourth and fifth lower teeth from the center. Cover with a piece of cling film and a small terry towel on top. Lie with a compress for about half an hour. The procedure should be done two to three times a day (depending on the intensity of pain). The course of treatment is from 10 to 15 days.
Vitamin therapy is indicated as part of complex treatment for both essential and symptomatic neuralgia. Prescribed from the first days of treatment are mainly B vitamins, known for their neuroprotective effect, as well as ascorbic acid and vitamin D.
Vitamins of group B (B1, B2, B3, B6, B12) are catalysts of reactions of intermediate metabolism in nerve fibers, have analgesic activity, especially vitamin B12 (cyanocobalamin), its deficiency leads to demyelination of nerve fibers. A course of intramuscular injections of this vitamin significantly, according to observations of clinicians, eliminates pain syndrome and improves the general condition of the patient.
Clinical studies have proven the role of B vitamins in normalizing the nervous system at all levels, reducing inflammation and reducing pain. They participate in metabolic processes, help strengthen the myelin sheaths of nerve fibers, axial cylinders, connective tissues, maintain their integrity and, accordingly, can help restore impaired innervation and normalize the transmission of nerve impulses. Preference is given to complex drugs in tablets, however, injection forms can be prescribed, and electrophoresis with vitamins can also be prescribed.
Physiotherapy is indicated both in the acute period of neuritis and for the prevention of relapses of the disease. During attacks, thermal procedures are prescribed. The use of ultraviolet irradiation of the affected half of the face, light therapy with infrared rays (Sollux lamp) is indicated. Moderate thermal exposure with an electric heating pad may be useful. [ 8 ]
Diadynamic therapy is widely used. Treatment with direct current impulses has a pronounced analgesic and anti-inflammatory effect. In the acute period, daily procedures are prescribed; two or three ten-day courses with a week interval are recommended. With the help of diadynamic currents, drugs are delivered - local anesthetic procaine or tetracaine, adrenomimetic epinephrine, which contributes to rapid pain relief.
Ultrasound and laser beam effects on the exit points of the trigeminal nerve branches, sinusoidal modulated currents, medicinal electrophoresis (for trigger pain - using the endonasal method with procaine and vitamin B1) are also used. D'arsonval for trigeminal nerve neuritis is performed by point effects on the affected half of the face in the areas where its branches exit onto the surface, the area under the earlobe, the cervical-collar area, and also the palmar surface of the phalanx of the thumb of the corresponding hand.
Exercise therapy for trigeminal neuritis is performed in the form of facial exercises and helps restore mobility to the affected part of the jaw, improve trophism and normalize reflexes. Massage for trigeminal neuritis is prescribed for the same purpose.
In complex treatment, a special place is given to reflexology. For some patients, acupuncture helps to fully recover without medication.
Also, as additional treatment methods and for the purpose of preventing relapses, mud therapy, ozokerite and paraffin applications, radon, sea, and sulphide baths are prescribed.
Folk remedies
Official medicine denies the possibility of curing inflammation of the trigeminal nerve using folk medicine methods. Of course, if it is necessary to reseal a tooth canal, then such treatment is unlikely to be successful. And in other cases, when radical interventions are not required, according to the patients themselves, folk remedies help faster and better. In addition, they do not have serious side effects. The disease does not belong to those where delay is like death, so you can almost immediately begin to help yourself with the help of folk remedies, which does not exclude a visit to the doctor and examination. After all, facial pain can be caused by various reasons.
Let's start with the simplest recipes for eliminating pain syndrome. According to those who have tried them, they help relieve pain immediately, and not on the second or third day like carbamazepine.
- Take an old teapot, put five cloves of garlic in it, cut into large (2-3) pieces. Pour boiling water and breathe through the spout of the nostrils on the affected side until the pain subsides. At the initial stage, literally several such procedures help. The pain goes away and does not return. The procedures are carried out when necessary to eliminate the pain syndrome.
- Take a freshly boiled hard-boiled chicken egg, peel it, cut it in half, and apply it to the points of most intense pain. When the halves of the egg on your face cool down, the pain syndrome will go away for a long time.
- Apply a freshly picked leaf of domestic geranium to the area where the pain occurs (it has an anti-inflammatory effect). [ 9 ]
- You can smear the areas of your face along the pain with black radish juice or apply grated horseradish wrapped in a piece of gauze. These substances have a local irritating effect, that is, they stimulate blood flow to the surface of the skin, and activating blood flow in the right direction, as practice shows, leads to normalization of the condition.
- It is also good to lubricate the skin of the face in the areas of pain with fir oil as needed. Three days of such treatment will relieve pain for a long time.
- Contrast procedure: rub the painful areas with a piece of ice, then massage them until they warm up. During one procedure, you need to do rubbing → massage three times.
Herbal treatment plays a big role in folk medicine. A mint decoction will help to cope with pain: pour a tablespoon of mint with a glass of boiling water and simmer in a water bath for 10 minutes. Infuse until it cools to about 40℃, filter, divide in half and drink in the morning and evening. The second portion needs to be slightly warmed up.
An infusion of yarrow is prepared in the same proportion and drunk throughout the day in three to five doses.
It is recommended to rinse your mouth with chamomile infusion (a teaspoon of dry crushed herb per glass of water) for neurodental problems.
Homeopathy
Homeopathic treatment is often effective in cases where official medicine fails. It must be carried out by a professional homeopathic doctor, then its success is guaranteed. The homeopathic medicine chest has an extensive arsenal for treating neuritis.
In case of damage to the second and third branches of the trigeminal nerve, alveolar mandibular processes, buccal nerve, the use of Aconite can be effective. Characterized by severe pain, causing anxiety and fear in the patient, paresis, convulsive twitching of the muscles of the affected area, loss of sensitivity. Aconite copes well with pain of inflammatory origin. In cases of hyperemia of the affected part of the face, it is taken alternately with Belladonna, in case of traumatic genesis - with Arnica, and neurostomatological problems are well relieved by a combination with Bryonia. These same drugs are suitable in some cases for monotherapy of trigeminal neuritis.
In case of right-sided lesion of the first branch, Chelidonium is used. In case of complications on the organs of vision, and on any side, Quininum sulphuricum can be effective.
Also used are Coffea, Hypericum, Ignatia and other drugs. Only a doctor can accurately prescribe treatment after studying the patient's medical history and inclinations. In this case, you can count on success, and quite quickly.
Surgical treatment
If conservative therapy is ineffective, there is intolerance to medications or their severe side effects, the question of surgical intervention is raised.
Modern neurosurgery has many methods of gentle surgical treatment. Currently, the following are used:
- to microsurgical release of the nerve section exiting the brainstem;
- puncture destructive operations;
- partial sensory nerve transection or its peripheral block by excising part of it and replacing it with muscle or fascial tissue.
Neuroectomy is performed using gentle methods with the use of ultra-low temperatures (cryodestruction), ultra-high temperatures (diathermocoagulation), and high-frequency radiation.
A promising direction is laser treatment of trigeminal neuritis. Dissection or removal of part of the nerve root with a laser beam ensures the absence of direct contact and blood, rapid healing and recovery.
Prevention
The main preventive measure is timely sanitation of the oral cavity, for which it is necessary to regularly (once every six months) visit the dentist in order to prevent the development of pulpitis and nerve removal.
It is also recommended not to neglect other chronic diseases, eat well, try to avoid accidental facial injuries and hypothermia, lead a healthy lifestyle and strengthen the immune system.
If you experience pain in the facial area, you need to get examined and find out the cause, rather than take painkillers and hope that it will go away on its own.
Forecast
With timely diagnosis and treatment, the prognosis is favorable. Usually, it is possible to cure neuritis with conservative methods. However, each case is individual.

