
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Ruptured thoracic and abdominal aortic aneurysm: chances of survival, treatment
Medical expert of the article
Last reviewed: 04.07.2025
The cardiovascular system, in which the scarlet liquid (blood) circulates, supporting the viability of the entire human body, consists of the heart and many vessels of various sizes. The largest of them is the aorta. It is in the aorta that the maximum blood pressure is noted, and if the walls of the blood vessel weaken, become less elastic, this causes their irreversible overstretching with the formation of an aneurysm. The aneurysm itself may not make itself known for a long time, and not interfere with a person's normal life, but you need to know that in some cases, aortic aneurysm dissection or rupture may occur, and this is an extremely life-threatening condition that requires immediate professional help from a vascular surgeon.
Useful information from anatomy
In connection with the above, the expression "rupture of the aorta or an aneurysm formed on it" sounds frightening. Therefore, it is not surprising if the reader is interested in the question of where the aorta is located, what it is, as well as what an aneurysm is and what factors can provoke its rupture.
The human circulatory system begins with a rhythmically contracting hollow muscular organ that functions like a pump. This organ was named the heart and its purpose is to ensure continuous circulation of blood that delivers oxygen and nutrients to all human organs.
Large blood vessels that communicate with the heart are divided into arteries and veins. The former drain blood from the heart, the latter are responsible for supplying blood to the central organ of the circulatory system. The largest human artery is the aorta, which is part of the systemic circulation, which supplies blood to the entire body, while the small one is responsible only for the blood supply to the pulmonary system.
The aorta, which comes out of the left ventricle of the heart and is a kind of continuation of it, can be compared to a pump hose. This large artery is very long and extends along the entire human body.
It is customary to distinguish 3 main sections of the aorta:
- ascending (originates in the left ventricle of the heart and debuts from the expanded part called the bulb),
- aortic arch (starts somewhere at the seventh centimeter of the vessel, has a curved shape),
- descending (in the region of the 4th thoracic vertebra the arch becomes a straight line).
The ascending aorta is hidden behind the pulmonary trunk, the artery that begins the lesser (pulmonary) circulation, and is covered by the pericardium. The diameter of the artery in this part is about 2.5-3 cm.
In the area of the junction of the second costal cartilage and the sternum (the main bone of the chest), the aorta narrows to 2 cm and takes the form of an arch, turning slightly to the left and back. Reaching the fourth thoracic vertebra, it forms a small isthmus, after which its position becomes almost vertical.
The descending aorta is in turn divided into 2 sections:
- the thoracic region, which is located in the chest cavity in the posterior mediastinum,
- the abdominal region, which is considered a continuation of the thoracic region and begins at the level of the 12th thoracic vertebra.
The initial section of the thoracic aorta is located in the anterior-left position from the esophagus. Then, in the region of the 8th vertebra, it bends around the esophagus on the left side and rushes down along the back wall of the esophagus.
The beginning of the abdominal section is considered to be the aortic opening of the diaphragm. Diving into this opening, the aorta extends to the 4th lumbar vertebra.
Along the aorta, branches of various sizes – arteries – branch off from it. In the ascending section, these are the right and left coronary arteries. In the area of the aortic arch, they originate:
- the brachiocephalic trunk, which in turn divides into the right carotid and subclavian arteries,
- left common carotid and subclavian arteries.
The descending part is divided into the thoracic section, where the intercostal, tracheal and many other types of arteries begin, and the abdominal section. The following emerge from the abdominal section:
- the celiac trunk, which after a couple of centimeters divides into the left gastric, common hepatic and splenic arteries,
- mesenteric blood vessels responsible for the blood supply to the intestines and pancreas,
- low diaphragmatic artery, which supplies the diaphragm and adrenal glands,
- adrenal artery,
- lumbar arteries,
- renal artery.
In the region of the 4-5 lumbar vertebrae, the abdominal part of the aorta is divided into 2 parts (its bifurcation occurs): the right and left common iliac arteries, the continuation of which are the femoral arteries.
Weakening of the walls of large blood vessels that experience maximum blood pressure can occur in any part of the aorta or arteries branching off from it. Overstretching of the aortic walls leads to them becoming weaker and prone to rupture in this area. Rupture of an aneurysm of the aorta or arteries branching off from it is dangerous in any case. But the prognosis in this case depends on many factors: the location of the aneurysm, its shape and size, the degree of damage to the arterial walls.
Aneurysm and its consequences
An aneurysm of the aorta and other large arteries is usually called a section where the vessel undergoes a pathological change in shape and size. In this section, an unusual expansion with an increase in the lumen of the arterial vessel is formed. A diagnosis of an aneurysm is made in the case of an increase in the lumen of the vessel by 2 or more times.
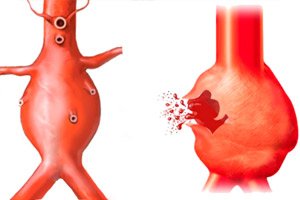
A distinction is made between spindle-shaped and saccular aneurysms. The spindle-shaped form is said to be observed when there is a diffuse protrusion of the artery walls along its entire diameter. The saccular form of aneurysm is characterized by the appearance of such a protrusion in a limited area of the vessel and its shape resembles a sac protruding from the side of the artery.
The aorta, like all blood vessels, has a three-layer wall. Under blood pressure, in the presence of risk factors for aortic damage, both individual layers of the vessel and all 3 layers can rupture. In the first case, they talk about aortic dissection. Usually, such a situation is observed at the site of an aneurysm and the aneurysm is called dissecting.
An aneurysm is a pathological protrusion of the aortic walls, which can be either acquired or congenital. The causes of acquired aneurysms are:
- inflammatory pathologies of the vascular wall caused by an infectious factor (aortitis, which develops against the background of syphilis, tuberculosis, postoperative infections),
- degenerative changes in the tissues of the aorta (atherosclerosis of blood vessels, defects in the structure of the aortic wall that arise after vascular surgery),
- medial aortic necrosis (a pathology whose causes are unknown, manifested in the formation of cystic cavities (necrotic foci) in the inner layer of the aortic wall),
- mechanical damage and injury to the largest blood vessel
Congenital aneurysms can occur in such hereditary pathologies as Marfan syndrome, Ehlers-Danlos syndrome, congenital elastin deficiency and other pathologies of the connective tissue of which blood vessels are composed.
It should be said that the risk of aneurysm is higher in people with high blood pressure (arterial hypertension) and hereditary predisposition. Smokers and fans of alcoholic beverages are at risk. As for sexual preferences, this pathology is more common in men. And it is most often found in older people (60 years and older).
A small aneurysm itself may not cause any symptoms until it grows and begins to compress nearby organs. Then a person begins to experience pain of varying intensity, plus symptoms appear that indicate problems with the compressed organs. If the aneurysm is located in the chest area, a cough and difficulty breathing appear, the voice becomes hoarse, and the pain is localized in the sternum, back, and neck. If the aneurysm is located in the abdomen, a person feels pain in the epigastric region, as well as a feeling of severe bloating and nausea. He may be tormented by belching, urination problems, and constipation.
This is an unpleasant, but not the most dangerous condition. The greatest danger is a ruptured aortic aneurysm. But in this place the vessel walls are the least durable, so the integrity of the aorta usually breaks down in such areas. This complication of an aneurysm is considered life-threatening and is treated strictly surgically.
It is believed that aortic rupture in the chest area is preceded by stratification of the vessel walls, when only the inner layers are subject to rupture. But in the abdominal part of the aorta, ruptures in most cases occur unexpectedly, and all 3 layers of the aortic wall are damaged. In this case, severe bleeding occurs, and patients in the vast majority of cases die. It can be said that an abdominal aortic aneurysm is a potentially very dangerous condition that requires treatment even in the early stages of development.
Epidemiology
According to statistics, spindle-shaped aneurysms are formed most often. Moreover, in 37 percent of cases, such protrusions occur in the abdominal part of the blood vessel. A little less often, aneurysms are diagnosed on the ascending part of the aorta (about 23 percent). Pathological areas on the arch and descending branch of the largest artery are detected in less than 20% of cases. Much less often, aneurysms are diagnosed in the area of the inguinal and femoral arteries.
Rupture of a dissecting aortic aneurysm is diagnosed much more often than damage to an aneurysm whose walls are intact. It is clear that a three-layer wall can withstand higher loads than one in which the inner or both the inner and middle layers are damaged. A dissecting aneurysm, which is an incomplete rupture of the aortic wall, has the highest risk of rupture and the worst prognosis.
The most dangerous is considered to be a rupture of the aorta in the abdominal region, which has a more severe course and certain difficulties in diagnosis.
Risk factors
Risk factors for rupture of an aneurysm of any large vessel include:
- atherosclerosis of blood vessels, because the formation of cholesterol plaques on the walls of arteries makes them less elastic,
- high blood pressure, which causes an aneurysm to form and subsequently increases the tension in that area even more,
- physiological age-related changes, i.e. wear and tear of various tissues of the body,
- congenital diseases of connective tissue, as a result of which its underdevelopment is observed, which means that it cannot efficiently perform the functions assigned to it,
- inflammatory vascular pathologies, which additionally weaken the internal tissues of the vascular wall (progressive syphilis, for example, can provoke the development of a chronic inflammatory process in the arteries, and this increases the risk of damage to the walls with the slightest stress),
- increased thrombus formation, since a harder thrombus will exert higher pressure on the aneurysm wall than liquid blood (and thrombi are literally drawn into the aneurysm cavity, where they subsequently accumulate, reducing the lumen and increasing the pressure on the weak walls)
- alcoholism and smoking (these bad habits create a high load on the heart, increase blood pressure and, accordingly, can become a risk factor for rupture of the walls of the heart and blood vessels)
- autoimmune and endocrine diseases that lead to rapid destruction of blood vessels (most often, aortic ruptures occur in patients with diabetes, especially if the pathology is combined with vascular atherosclerosis, which is typical of diabetes).
It should be said that any increased load on the heart can provoke a rupture of the aortic walls. Such a negative impact on the heart can be caused by:
- strong emotions and stress,
- excessive physical activity (in the case of an aneurysm, even moderate, slightly increased tension on the vessels is often enough to cause them to rupture at the weak point),
- pregnancy and childbirth (in this case, not only the heart, but also other organs of the woman experience increased stress, therefore, expectant mothers with cardiovascular pathologies are registered separately, while an aneurysm can form both before conception and in the last months and days of pregnancy, and rupture at the time of childbirth),
- excess weight, obesity, physical inactivity, which negatively affect the heart and blood vessels, gradually weakening them.
- chest and peritoneum injuries (for example, aortic aneurysm ruptures quite often in road accidents as a result of a sharp blow to the steering column or during a fight, when the blow falls in the area where various sections of the aorta pass). If the blow is strong, even an undamaged section of the vessel can rupture. In this case, all 3 layers of the aorta are usually damaged, which leads to the death of the victim.
Why do pathological foci form, which subsequently become a risk factor for aortic wall rupture? The pathogenesis of this process is based on multifactoriality. Inflammatory and degenerative processes in tissues, the formation of cholesterol plaques on the walls, and traumatic injuries cause pathological changes in the structure of the vascular wall.
Structural and geometric changes in the collagen and elastin fibers that make up the vascular membrane lead to an unnoticeable destruction of the arterial walls, so it is not surprising that when stretched, they cannot return to their normal position. At the same time, the once damaged shape of the wall cannot be naturally corrected, but may well progress, i.e. the size of the aneurysm may gradually increase, and the larger the area of damage to the vessel, the higher the risk of its rupture, and the more difficult it is to save the patient's life.
The diameter of the aneurysm is directly proportional to the pressure on the vessel walls and the rupture force. With an aneurysm diameter of less than 5 cm, the risk of wall rupture approaches 1%, while a seven-centimeter aneurysm increases the risk of tissue rupture to 30 percent or more.
Pathogenesis
It is believed that the appearance of a focus of pathological stretching of the blood vessel wall is itself one of the main risk factors for aortic rupture, because in this place the tissue becomes thinner and less elastic, so it can rupture with any increase in pressure on it. It is clear that the causes of aortic rupture will be closely related to the factors causing the appearance of the aneurysm itself, most often occurring in the area of increased tension of the vessel walls.
Symptoms of a ruptured aortic aneurysm.
It should be said that a person may not even suspect such a pathology as an aortic aneurysm for a long time, because pronounced symptoms of the disease usually appear when the pathological area reaches large sizes and begins to have a negative impact on the work of other organs. But an aneurysm rupture cannot proceed asymptomatically.
The first signs of an aneurysm rupture are considered to be high-intensity pain. However, the localization of pain may differ depending on the location of the aneurysm. A ruptured thoracic aortic aneurysm will debut with attacks of pain in the sternum area, while the symptom may radiate to the back, shoulders or neck, much less often to the abdomen, upper and lower extremities.
A similar situation is observed with a rupture of an aneurysm of the ascending aorta, its arch or descending section.
Most often, in this case, we are not talking about a complete rupture, but about a dissecting aneurysm, the symptoms of which are considered to be:
- migrating pain (pain syndrome with difficult to determine localization, caused by hemorrhage into the lumen between the aortic membranes), they are observed along the course of hematoma formation),
- tachycardia (rapid pulse, which is different in the upper and lower extremities),
- fluctuations in blood pressure, first increasing and then decreasing,
- neurological symptoms caused by ischemia of the brain and spinal cord (weakening of the muscles of half the body, decreased sensitivity or paralysis of the limbs), impaired consciousness, dizziness, damage to peripheral nerves,
- the appearance of shortness of breath,
- hoarse voice,
- severe weakness and sweating,
- pale or bluish skin color,
- formation of edema, etc.
In severe cases of blood leakage outside the aorta, hemopericardium, myocardial ischemia, heart failure, and cardiac tamponade may develop.
If the aneurysm dissection occurs in the descending thoracic or abdominal aorta, symptoms of acute renal failure, ischemia of the digestive organs or lower extremities may occur.
Rupture of an abdominal aneurysm is characterized by abdominal pain. The clinical picture of this pathology is characterized by symptoms of acute abdomen: severe pain in this area and tension of the abdominal wall. Most often, we are talking about a complete rupture of the aortic membranes with its characteristic symptoms:
- the appearance of acute, unbearable pain in the epigastrium (if the rupture occurred in the thoracic part of the aorta, the localization of pain will be different),
- severe dizziness up to loss of consciousness and coma,
- nausea with bouts of vomiting,
- dryness of the oral mucosa,
- bluish skin color,
- pulse is weak, threadlike,
- cold sweat,
- heavy, intermittent breathing,
- heart rate increased,
- a sharp decrease in blood pressure is observed, and collapse may occur.
The intensity and localization of symptoms of aortic aneurysm rupture are affected by the location of the tissue integrity violation and the size of the resulting hematoma. Retroperitoneal aortic rupture is characterized by severe, persistent pain in the abdomen and lower back. The larger the hematoma, the more it presses on the nerve trunks. This causes excruciating pain syndrome that cannot be relieved with analgesics.
If the rupture of the vessel tissue occurred in the upper part of the abdominal region or the descending part of the thoracic aorta, the pain may radiate to the heart, resembling the clinical picture of a ruptured cardiac aneurysm. The spread of the hematoma to the pelvic area will cause pain not only in the lumbar region, but also in the groin area, perineum. Irradiation to the thigh is possible.
For example, a rupture of an aneurysm of the splenic artery coming out of the abdominal aorta, with a retroperitoneal rupture, manifests itself as pain in the left half of the abdomen and lower back. The formation of a hematoma somewhat stops the bleeding, but is accompanied by the appearance of bruises on the side, abdomen, thighs and groin area (depending on the size and extent of the hematoma). Patients experience a decrease in blood pressure and signs of anemia. Symptoms from the abdomen in this case are not so intense, which is associated with a small amount of blood flowing from the aorta (no more than 1 glass).
Blood leakage into the abdominal cavity is accompanied by the development of collapse, loss of consciousness, cold sweat, pale skin, weak pulse and other dangerous symptoms, while pain is felt throughout the abdomen. Penetration of blood from the artery into the gastrointestinal tract is accompanied by pain in the stomach, intestines or pancreas. In the latter case, the pain will be of a girdle nature.
Symptoms of intraperitoneal aneurysm rupture are more pronounced, they are accompanied by the development of hemorrhagic shock and manifestations of internal bleeding. There is severe bloating and abdominal pain, the pulse becomes frequent but very weak, the skin is pale, covered with cold sweat. The clinical picture may resemble acute appendicitis or peritonitis. In addition, the pathology is characterized by the Shchetkin-Blumberg symptom, when the pain intensifies when pressing and removing the hand from the abdomen.
The symptoms of an intraperitoneal rupture develop rapidly, so there is usually no time left for diagnostic measures.
If an aortic aneurysm ruptures into the vena cava, a gradual progression of symptoms is noted: weakness, shortness of breath, rapid heartbeat, pain in the abdomen and lumbar region, swelling that spreads to the lower part of the body and legs. In the peritoneum, a pulsating area can be easily felt; listening will show the appearance of a systolic-diastolic murmur above it.
A rupture of an aortic aneurysm or large arteries branching off from it can also occur in the duodenum or other organs of the gastrointestinal tract. In this case, symptoms of gastrointestinal bleeding are evident: black stool formed by a mixture of blood and gastrointestinal contents, vomiting blood, rapidly occurring collapse (a sharp drop in blood pressure). Pain syndrome localized in the epigastric region is not decisive here, although these pains cannot be called weak.
It is important to understand that an aneurysm, which is most often localized in the area of large vessels with high blood pressure, can also form in smaller arteries that branch off from the aorta. So, the iliac arteries branch off from the abdominal part of the aorta, which smoothly pass into the femoral area. In this area, an aneurysm does not occur so often, and a rupture of an aneurysm of the femoral artery can be considered a rare pathology. But this is possible, as indicated by the following symptoms: pain in the legs, numbness of the lower limbs, cramps, a feeling of cold in the feet and white skin on the feet, the appearance of bleeding ulcers and bruises in the area of the anterior abdominal wall, groin, weakness, decreased pressure, tachycardia.
Despite the fact that the femoral artery is not as large a blood vessel as the aorta, bleeding in the event of its rupture can be quite severe, and foci of necrosis and gangrene may appear at the site of the hematoma.
Forms
We have already noted that an aortic aneurysm rupture can occur anywhere in this large blood vessel, and the location of the rupture determines the prognosis of not only health, but also life. Quite often, doctors use a simplified classification, dividing the aorta into 2 large sections:
- rupture/dissection of the upper (proximal) or thoracic aorta,
- rupture/dissection of the lower (distal) or abdominal aorta.
As we can see, doctors consider 2 types of damage to the aortic wall that are considered life-threatening:
- complete rupture, when the integrity of all layers of the vessel wall is broken and blood flows outside the artery,
- incomplete rupture or delamination with damage to 1-2 internal layers and penetration of blood into the space between the layers of the blood vessel.
According to the classification of American cardiac surgeon Michael DeBakey, incomplete damage to the aortic walls can be viewed from this perspective:
- dissection of the aortic walls simultaneously in the ascending and descending sections (generalized form or type 1)
- rupture of the internal membranes of the vessel, localized mainly in the ascending part and arch of the aorta (type 2),
- dissection localized in the descending aorta (type 3).
The Stanford classification considers only 2 types of bundles:
- ascending aortic dissection (type A),
- rupture of the internal membranes of the vessel in the area of the arch and descending section (type B).
Since the aortic wall consists of three-layer connective tissue, its rupture is considered as a sequential violation of the integrity of the layers, starting from the inner and ending with the outer, which is the last to rupture. The violation of the inner layer leads to the fact that the blood begins to leak into the space between it and the middle layer. Individual components of the blood and increased pressure begin to destroy the middle layer, which can also be damaged, releasing blood further into the space between the subendothelium and the outer shell. The stratification intensifies and eventually the outer layer cannot withstand it, which, like the others, ruptures, and the blood goes beyond the aorta.
All these stages follow one after another, but the interval between them may vary. A person with a dissecting aorta may die in the first minutes after the rupture or live with this pathology for several years.
There is a classification of stages, or more precisely forms of aortic rupture:
- Acute form, when a successive change of rupture stages occurs during the first 2 days. There is practically no hope that a person will survive with this form of rupture, since 9 out of 10 patients do not even have time to be taken to the hospital (death occurs at home or on the way to a medical facility).
- Subacute form. The duration of the change of stages of aortic dissection in this case can reach 2-4 weeks, which gives a person some time to recognize the disease and seek help.
- Chronic form. In this case, the ruptures are small and there is a large gap between the stages of delamination. The process can last from several months to several years, which allows saving a person's life with the help of an operation, which is necessary regardless of the form of the disease.
It can be said that the faster the stages change, the less chance a person has to survive. With a strong blow to the heart or abdomen, for example, during a car accident or fight, the aorta ruptures so quickly that the victim can die within a few minutes due to severe bleeding.
Complications and consequences
If you hit your leg or arm hard, a large hematoma will form on them, which hurts a lot when pressed and swells due to bleeding in this area. If the bruise is small, it does not pose a particular danger, but a large, gradually increasing hematoma can pose a serious problem, which is fraught with tissue necrosis, the development of purulent processes under the skin, and limitation of limb mobility.
When tissue integrity is compromised, blood begins to ooze out, and the longer this happens, the worse the patient will feel. Even with minor bleeding, we first try to stop the bleeding.
An identical situation is observed with a ruptured aortic aneurysm, but it is important to understand that the aorta is not a peripheral vessel, the diameter of which is insignificant, and the blood pressure in it is much higher. That is, we are not talking about a small hemorrhage, but about serious bleeding, when about 200 ml or more of blood accumulates in the internal cavities.
Aortic dissection itself does not always lead to severe bleeding, but there are circulatory disorders that can eventually lead to ischemic myocardial infarction or stroke. The fact is that an aneurysm creates conditions for the formation of blood clots, which in turn can clog blood vessels, preventing the flow of blood carrying oxygen to the body's tissues. And the brain and heart are the first to suffer from hypoxia. Ischemic disorders make organ tissues weak and unable to perform their functions.
Often, smaller vessels, usually responsible for the nutrition and respiration of the tissues of the lower extremities, become blocked. The legs begin to freeze more often, the risk of frostbite and the development of ulcerative processes increases.
The penetration of blood between the layers of the aortic wall also causes necrotic processes in the tissues, which weaken them and lead to rupture, which is considered a fairly common and most dangerous complication.
Penetration of blood into the chest or abdominal cavity has its unpleasant consequences. In the first case, compression of lung tissue and displacement of mediastinal organs occurs, respiratory failure increases, and the risk of hemorrhagic shock caused by internal bleeding increases. Coagulated blood causes the development of purulent processes in the pleura. Hemothorax is considered an emergency condition that can lead to the death of the patient.
Penetration of various substances and liquids, including blood, into the abdominal cavity becomes a risk factor for the development of purulent-inflammatory processes there. Peritonitis is one of the most life-threatening conditions for a person, which can quickly end in death. Especially if there is severe blood loss with a drop in pressure and acute signs of anemia. That is why an intra-abdominal aneurysm rupture is considered the most dangerous condition, which in the vast majority of cases ends in the death of the patient.
It turns out that, no matter how you look at it, a ruptured aortic aneurysm does not pass without a trace, and a person's death is a matter of time if he is not given timely assistance. And it is better if this assistance is given at the stage of aneurysm formation, and not when a rupture of its membranes is diagnosed.
Diagnostics of a ruptured aortic aneurysm.
An aneurysm itself is a potentially dangerous condition, which increases the risk of rupture of the tissues of the largest blood vessel many times over. Therefore, the sooner such a pathologically stretched section of the vessel wall is detected, the greater the chances of preventing its rupture.
Aortic aneurysm is a condition that can be detected both during a routine examination (for example, in an asymptomatic course) and when a patient seeks medical attention due to pain in the heart or epigastrium during chest and abdominal X-ray. An aneurysm in the ascending aorta can be detected during transthoracic or transesophageal echocardiography, and in the descending aorta – by means of Doppler ultrasonography of the vessels of the chest or abdominal cavity.
Magnetic resonance computed tomography and aortography help to clarify various parameters of the aneurysm. The latter, although considered an invasive method, allows you to detect the localization of the initial section of the rupture, assess the length of the dissected section, various disturbances in the structure of the vessel leading to dissection of the tissues of the aortic wall, the size of the lumen and other diagnostically important parameters. While a tomogram allows you to determine the direction of dissection, the involvement of aortic branches in the process, the state of the aortic valve.
But if, in most cases, patients come on foot to diagnose a normal and dissecting aortic aneurysm, then when it ruptures, the person is usually brought in by ambulance, and diagnostic procedures are carried out directly on the operating table.
The doctor's task in this case is to assess the location of the rupture and the size of the hematoma as soon as possible in order to decide on the further treatment plan. In this case, computer and magnetic resonance imaging, ultrasound examination, laparoscopy, aortography and other available methods come to the rescue. The fact is that when the aorta ruptures, every minute counts, so there is often no time left to transport patients to centers equipped with MRI and CT equipment.
It is clear that the patient's complaints and pale skin will not be enough to make a tentative diagnosis. During palpation, the doctor may detect a pulsating compaction in the peritoneum, which indicates the presence of an aneurysm in the abdominal aorta (although pulsation is not always felt). Listening to the sounds of the heart will show the presence of systolic murmurs in the projection of the dilated section of the aorta. Blood tests will indicate signs of anemia.
Instrumental diagnostics allows the doctor to visualize his suspicions and assess the degree of their danger. Thus, ultrasound angiography allows visually assessing the size of the aneurysm, the location of the rupture and the size of the hematoma near the aorta. With the help of spiral computed tomography, it is possible to assess not only the location and size of the rupture, but also its relation to various arteries that branch off from the largest blood vessel, which is the aorta, and differentiate an old hematoma from a new one. The presence of a rupture will also be indicated by the displacement of nearby organs relative to the aorta.
A computer or magnetic resonance imaging scan not only helps to determine the method of treating the rupture, but also, if aortic stenting is necessary, allows one to determine the size of the stent.
It is important to understand that not all clinics are equipped to perform CT or MRI, so it usually comes down to X-rays and ultrasound. If these studies are not possible, and the upper pressure indicator (systolic blood pressure) is not less than 90 mm Hg, endoscopic techniques (laparoscopy) come to the rescue, which is effective in the case of a rupture of the abdominal aorta. In this case, a rupture of the vessel will be indicated by the detection of a hematoma in the area of the aorta near the small intestine, as well as the presence of blood that colors the serous fluid scarlet.
Laparoscopy can also be useful in the postoperative period to assess the quality of the operation and recovery processes.
Aortography (contrast radiography) is a diagnostic method used in situations where diagnosis is difficult or the doctor requires more information about:
- the relationship between the aneurysm and the branches of the aorta,
- the spread of the pathological focus to the site of bifurcation of the distal part of the vessel and its transition into the iliac arteries,
- to clarify the nature of damage to the branches extending from the aorta,
- to detect such a rare pathology as aortocaval fistulas.
It should be said that aortic aneurysm rupture is a diagnostically rather complicated situation. On the one hand, you need to act quickly, because time spent on diagnostics can cost a person their life, but on the other hand, the symptoms of the pathology can resemble many other diseases, and the clinical picture can change significantly depending on the location of the rupture, its size and nature.
 [ 35 ]
[ 35 ]
Differential diagnosis
The greatest difficulty is differential diagnostics of abdominal aortic aneurysm rupture. The symptoms of acute abdomen characteristic of it can be observed in pancreatic necrosis, acute cholecystitis, appendicitis, peritonitis caused by perforation of gastric ulcer or rupture of the cecum, etc. Pain in the lower back, characteristic of aortic rupture in its abdominal section, are also signs of acute kidney diseases and urogenital tract, radiculitis, girdle pains are characteristic of exacerbations of pancreatitis. Symptoms of internal bleeding require differentiation of aortic bleeding from gastrointestinal.
A presumptive diagnosis in this case may be "acute obstruction of the bifucation of the aorta and its branches feeding the lower limbs." In principle, thrombosis of the vessels causing obstruction is quite possible, but if you pay attention only to this point, causing ischemia of the lower limbs, you may not notice in time a much greater danger, which is a rupture of the aorta.
If we are talking about aortic dissection or rupture in the thoracic region, then its symptoms, such as cough and difficulty breathing, can mislead the doctor, resembling the symptoms of inflammatory diseases of the respiratory tract. Thus, the patient may be examined by a therapist or pulmonologist, while he clearly has a cardiological problem.
Such mistakes and delays in making a final diagnosis often result in tragic consequences. However, the doctors' fault is not as great as it seems. A dangerous pathology with such controversial manifestations sometimes causes difficulties in diagnosis even for experienced clinicians with many years of experience, not to mention paramedics and therapists who do not have such knowledge.
Who to contact?
Treatment of a ruptured aortic aneurysm.
If even an experienced doctor cannot always accurately diagnose and assess the degree of danger of a given pathology by eye, then what can we say about people who are not initiated into medical issues. Nevertheless, patients with aortic ruptures, near which such an uninitiated person may be, can only count on him and the patient's life will depend on the correctness of the actions to provide first aid to the victim.
First aid for aortic rupture
The same should be done if symptoms appear that are part of the clinical picture of a ruptured aortic aneurysm and pose a danger to life? First of all, there is no need to panic or try to compare these symptoms with manifestations of other diseases in the hope of the best, assuming that this is an exacerbation of diseases of the gastrointestinal tract or respiratory system. Pale skin, a sharp drop in blood pressure, thready pulse, breathing problems and sudden severe pain of various localizations are not at all safe symptoms, the interpretation of which is the job of a specialist. Therefore, in any case, when they appear, you need to:
- Call an ambulance immediately, remembering to mention the extremely serious condition of the patient and the suspicion of acute cardiovascular pathology (in this case, resuscitation should arrive, and in a short time).
- If a person has previously been diagnosed with an aneurysm, it is imperative to tell the ambulance operator and then the paramedic about this diagnosis.
- It is also necessary to ensure free access for the doctor to the entrance and apartment (house) so that help can arrive as soon as possible.
- The patient must be immediately laid on a flat horizontal surface, with the head slightly raised in relation to the feet.
- The victim's clothing should not constrict the chest and abdominal cavity: unbutton the collar and top buttons of the shirt (if necessary, unbutton the clothing completely or take it off), loosen the corset or belt.
- The patient may experience mental and motor agitation, so you need to try to keep him from unnecessary movements and ensure a motionless position, which will affect the intensity of bleeding, because it is severe bleeding that often causes the death of the patient.
- Circulatory problems caused by a ruptured aorta result in tissues not receiving enough oxygen, so to reduce the symptoms of oxygen starvation, it is necessary to increase the oxygen content in the blood by allowing fresh air into the room where the patient is located (this will also make it easier for the victim to breathe).
- The first thought of many when health problems occur is the desire to alleviate the patient's condition with pills, but since the diagnosis of the disease is unknown, it is difficult to navigate with medications for first aid. Giving blood pressure medications, analgesics, laxatives and other drugs is not recommended. The best option to help reduce pain in acute cardiovascular pathologies is a nitroglycerin tablet under the tongue.
- Before the ambulance arrives, the patient should not be given any food or drink.
- The occurrence of severe pain, especially in the heart and lower abdomen, is often a reason for panic in the patient himself. In this case, you need to try to calm the person down, because worries can only increase the pressure in the heart and blood vessels, which will increase the force of bleeding.
Since we do not know exactly what we are dealing with, it is better not to make any other attempts to help the patient. The only thing we can do is to provide him with bed rest and peace, and the treatment of the victim and the maintenance of his vital functions should be handled by specialists, especially since the treatment of an aneurysm rupture is surgical, because from such a large vessel coming directly from the heart, a large amount of blood can flow out under pressure and it is impossible to stop this process with medication.
Aortic aneurysm rupture is a condition that requires emergency care, and it will be a great success if the person is delivered to the hospital alive. However, doctors always hope for the best. The fight for the patient's life begins in the ambulance and in the emergency room, where the Rh factor and blood group, hemostasis indicators are determined, catheters are inserted into the central vein and bladder.
Upon arrival at a medical facility, the patient is often almost immediately sent to the intensive care unit, where diagnostic measures are carried out in a short time, allowing for the development of an effective treatment plan for the victim, the functions of vital organs are assessed: heart, kidneys, lungs. Along with diagnostics, various parameters are measured: blood pressure, heart rate, body temperature, respiratory rate and frequency, etc. If necessary, life support devices are immediately connected.
Doctors have a limited choice of methods for treating aortic aneurysm rupture. This is either an intracavitary operation or endoprosthetics (stenting) of the aorta, which is an operation in any case. Unfortunately, traditional drug and physiotherapy treatments remain powerless in this case.
Intracavitary surgery involves opening the sternum or abdominal cavity (depending on the location of the rupture), removing the part of the aorta where the integrity of the vessel wall has been violated (aneurysm resection), and installing a synthetic prosthesis in this area. This is a fairly common operation, the features of which are well known to cardiac surgeons (it is important to understand that surgery on large vessels can only be performed by a specialist, i.e. a vascular or cardiac surgeon).
But such operations have many disadvantages: low survival rate due to the high trauma of the intervention and high risk of developing all sorts of complications. The fact is that most patients with aortic rupture have other problems with the cardiovascular system. These are myocardial ischemia, cerebrovascular accidents, arrhythmia, arterial hypertension, carotid artery atherosclerosis, etc., which can become a risk factor for developing all sorts of complications and even be a contraindication to surgery. The doctor has to assess the risk of performing such an operation, and it is often extremely high, leading to a fatal outcome.
Unlike abdominal surgery, endoprosthetics is considered a low-traumatic method of performing surgical actions, which makes it possible to perform it on patients with heart and vascular diseases. In this case, transvascular introduction of prostheses (stents) is used, strengthening the vascular walls and replacing the tissues of the damaged area. Usually, the stent is inserted in the femoral artery under local anesthesia, which is tolerated much better than general anesthesia required for intracavitary surgery. The stent-graph is inserted in a folded state using a conductive system, which is removed after the stent is opened at the site of the rupture. Endoprosthetics is performed under X-ray control.
The first and main goal of aortic surgery is to stop internal bleeding, which can be done in various ways:
- by applying special clamps to the arteries,
- by introducing a special balloon catheter into the arterial bed,
- compression of the aorta, etc.
If there is no possibility of performing an urgent operation, and delay is tantamount to death, pneumatic compression of the body is performed, which allows one to gain from 2 to 5 hours of time.
But it is not enough to stop the bleeding surgically. It is also necessary to restore the integrity of the aorta and normal blood flow in it, which is what synthetic prostheses help to do. In addition, it is necessary to remove the symptoms of the disease: relieve pain, normalize blood pressure, carry out preventive measures to prevent renal failure and some other measures that improve the patient's condition and speed up recovery after surgery.
Consequences after surgery
Despite the vast experience of vascular surgeons and the widely used low-trauma methods of treating aortic aneurysm rupture, such operations are far from always successful. It happens that the patient dies simply on the operating table or after the operation. Statistics are especially unfavorable for older people and those with cardiovascular diseases.
Recovery and rehabilitation after aortic aneurysm rupture can proceed in different ways. Depending on the type of surgery, the patient must stay in the hospital for a certain period of time. After intracavitary intervention, a hospital stay of 2 weeks is mandatory, and after vascular stenting, the patient can return home after 2-3 days. After traditional intervention, the postoperative period is extended for up to 14 days, after which the patient can be discharged home, but only if the prosthesis is in a satisfactory condition after the stitches are removed. But endoprosthetics provides for a reduction in the entire rehabilitation period to 14 days.
Unpleasant consequences after surgery that force the patient to remain in hospital under the supervision of a doctor are considered to be:
- bleeding in the area where the stitches were placed,
- blockage of blood vessels by blood clots,
- inflammation of tissues in the area of surgical sutures,
- pulmonary edema,
- distal migration (displacement) of the stent,
- obstruction of the prosthesis,
- occlusion of the renal arteries with a tent,
- urinary dysfunction (a poor prognostic sign indicating progressive renal failure, which again can cause the patient's death).
Complications during endoprosthetics occur much less frequently than during abdominal surgery (no more than 20% of cases). In order for the patient to be discharged home from the hospital, the X-ray and laboratory data must be normal.
After discharge from the hospital, the patient is required to undergo monthly examinations by a cardiologist and, if necessary, visit a doctor for any unusual symptoms. This is a necessary condition that must be observed during the first year.
To avoid possible complications, a person will have to constantly monitor the level of blood pressure and, if it increases, take antihypertensive drugs, avoid heavy physical exertion and stressful situations, and eat right. Doctors do not restrict patients in movement, but overwork in this case is unacceptable, and patients get tired very quickly even from ordinary simple housework.
If a patient who has suffered an aortic aneurysm rupture is subsequently referred for surgery on any other organs, including dental surgery, a course of antibiotic therapy is required to prevent various complications, as well as antihypertensive drugs and anticoagulants, which will prevent the formation of blood clots.
Prevention
Prevention of aortic aneurysm rupture before surgery can include timely treatment of emerging cardiovascular diseases, giving up bad habits, and preventive medical examinations.
Since 90% of cases of aortic aneurysm formation are caused by atherosclerosis of the vessels, such a dangerous pathology can be avoided by carrying out atherosclerosis prevention: following a diet that includes a minimum amount of fats and harmful cholesterol, moderate but regular physical activity, quitting smoking and drinking alcohol, using folk recipes to cleanse the vessels of cholesterol plaques.
If an aneurysm has been detected, a person should regularly visit a cardiologist who will monitor the patient's condition, prescribing the necessary tests (for example, Dopplerography or duplex scanning of blood vessels). Now it will be necessary to constantly monitor the level of blood pressure and cholesterol in the blood.
If a person learns about an aneurysm only when it ruptures or simply ignores the requirements for preventing aortic aneurysm rupture, it will no longer be possible to avoid surgery. But even after surgery, the patient will have to follow certain requirements that will prevent relapse of the disease, because the cause of the aneurysm is not removed surgically:
- complete rejection of bad habits (smoking, drinking alcohol),
- gentle regimen for at least 1 month after surgery (limitation of physical activity, avoidance of emotional experiences and nervous tension),
- maintaining weight within the age norm,
- regular measurement of blood pressure (2 or more times a day) and its reduction if the readings exceed 130/85 mm Hg,
- proper nutrition (fractional meals, food should be sufficiently chopped, strict selection of products and dishes).
As for the diet of patients after aortic surgery. They are prohibited from eating spicy, fried foods, products containing animal fats, fatty meats and fish, rich broths, offal, strong tea and coffee, cocoa and chocolate in large quantities. Products that cause increased gas formation (beans and legumes, fresh and sauerkraut, white bread, etc.), as well as carbonated drinks, are also prohibited.
The amount of salt in dishes should be limited to 4-5 g per day, the amount of water drunk - up to 1 liter per day. But products that have a laxative effect will benefit such people. Dried apricots and prunes are considered especially useful, which go well with flax seeds.
For six months after the operation, physical activity should be low, but hypodynamia should also be avoided. If the doctor allows, 4-5 months after treatment, you can practice health walking, swimming, and slow running. It is better to start exercising under the supervision of specialists as part of rehabilitation programs.
It is also worth limiting the lifting of heavy objects. The maximum weight of objects lifted is 5 kg, otherwise you cannot avoid increased pressure or damage to the seams.
Now the person will have to be especially careful, because he may simply not survive the repeated formation and rupture of the aortic aneurysm. The mortality rate of even the first operations is very high, and what can we say about similar interventions in the work of the body weakened by the disease and its treatment.
Forecast
Aortic aneurysm rupture is a pathology that leaves patients with no chance of survival without professional treatment. No pills, folk remedies, or physiotherapy can help in such a situation. Only timely stopping of bleeding and vessel prosthetic surgery give a person hope, although it is very weak. About 90 percent of patients who have undergone abdominal surgery die in the near future. The prognosis after vascular stenting is more favorable, although additional surgeries may be required later (the stent has a limited period during which it can perform its functions well).
It should be said that aortic surgery allows 50% of patients to live for another 5 years or more, which is also important. But even in the absence of complications immediately after surgery, long-term consequences may occur, such as:
- thrombus formation and blockage of blood vessels by thrombi,
- formation of fistulas in the intestine (this is possible after surgery on the abdominal aorta),
- suppuration of tissues in the area of the prosthesis,
- deterioration of sexual function and urinary system.

