
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Symptoms of appendicitis: what to pay attention to?
Medical expert of the article
Last reviewed: 07.07.2025
The first signs of appendicitis include periumbilical colic. Localized pain coincides with irritation of the parietal peritoneum. The pain increases over 24 hours, accompanied by nausea, vomiting, and loss of appetite. [ 1 ] In 3.5% of cases of appendicitis, deep palpation of the left iliac fossa causes pain in the right iliac fossa, which is called Rovsing's sign. [ 2 ] If the patient has a positive Rovsing's sign, a barium swallow is used to confirm the diagnosis. Initially, the barium swallow method was found to be 95% accurate. [ 3 ]
Symptoms that allow diagnosis
Abdominal pain is the main complaint of patients with acute appendicitis. The diagnostic sequence of colicky central abdominal pain followed by vomiting and migration of pain to the right iliac fossa was first described by Murphy but may be present in only 50% of patients. Typically, the patient describes periumbilical colic that increases in intensity over the first 24 hours, becomes constant and sharp, and migrates to the right iliac fossa. The initial pain is referred pain resulting from visceral innervation of the midgut, and localized pain is due to involvement of the parietal peritoneum after progression of the inflammatory process. Loss of appetite is often the predominant feature, and constipation and nausea are common. Profuse vomiting may indicate the development of generalized peritonitis after perforation but is rarely the main feature of simple appendicitis. A meta-analysis of symptoms and signs associated with the presentation of acute appendicitis failed to identify any diagnostic feature, but showed that pain migration was associated with the diagnosis of acute appendicitis.[ 4 ]
This classic presentation may be influenced by the patient's age and the anatomical position of the appendix. Patients at the extremes of age may present diagnostic challenges due to a nonspecific presentation, often with subtle clinical features. Infants and young children often appear withdrawn, and older adults may appear confused. A high index of suspicion for acute appendicitis is necessary in these patients.
Anatomical aspects of acute appendicitis manifestation
The appendix is a tubular structure that attaches to the base of the cecum at the point where the taeniae coli enter. In adults, it is approximately 8–10 cm long and represents the underdeveloped distal end of the large cecum seen in other animals. In humans, it is considered a vestigial organ, and acute inflammation of this structure is called acute appendicitis.
- Retrocecal/retrocolic (75%) - often presents with right lumbar pain, tenderness on examination. Muscle rigidity and tenderness on deep palpation are often absent due to protection from the overlying cecum. In this position, the psoas muscle may be irritated, causing hip flexion and increased pain on hip extension (sign of a psoas strain).
- Subcecum and pelvic region (20%) - suprapubic pain and urinary frequency may predominate. Diarrhea may result from rectal irritation. Abdominal tenderness may be absent, but rectal or vaginal tenderness may be present on the right side. Microscopic hematuria and leukocytes may be present on urinalysis.
- Pre- and post-ileal (5%) - signs and symptoms may be absent. Vomiting may be more severe and diarrhea may result from irritation of the distal ileum.
The study gives a fairly clear picture in the form of specific symptoms. More than two hundred of them are described, but not all of them have absolute diagnostic reliability, but the simultaneous combination of three or four of them already clearly indicates the development of appendicitis.
Survey
The patient often presents with redness, dryness of the tongue, and associated foul odor from the mouth. Fever (up to 38°C) with tachycardia is not uncommon. Abdominal examination reveals localized tenderness and muscle rigidity following localization of pain in the right iliac fossa. Rebound tenderness is present but should not be induced to avoid disturbing the patient. Patients often find that movement increases the pain, and if asked to cough, the pain is often localized to the right iliac fossa. The site of maximal tenderness is often said to be over McBurney's point, which is two-thirds of the way along a line drawn from the umbilicus to the anterior superior iliac spine. Rectal and vaginal examinations may be normal, although there may be tenderness on the right side, particularly in the pelvic process. Tenderness on rectal examination may be suggestive of, but is not diagnostic of, appendicitis. Percussion tenderness, guarding and rebound tenderness are the most reliable clinical findings indicating the diagnosis of acute appendicitis.
The leading and absolutely pathognomonic of these are tension of the anterior abdominal wall (defence symptom) and a positive Shchetkin-Blumberg symptom in the right iliac region. Of the other symptoms of appendicitis, the following have received the greatest recognition:
- Bartomier-Michelson symptom. The patient is placed on the left side. When palpating the right iliac region, pain appears, and compared to the initial localization, it shifts more medially.
- Voskresensky's symptom. The patient is lying on his back. The shirt is pulled up with the left hand, and with the right hand it is moved from the epigastrium to the right side, pain appears in the area of the appendix.
- Karavanova's symptom. Press the right lower side with the palm, hold until the pain subsides, then ask the patient to cough. With appendicitis, pain appears again. Kushnirenko describes the same technique without pressing.
- Lennander's symptom. The difference in temperature in the armpit and rectum is more than 1°.
- Obraztsova symptom. Increased pain on the right when raising the right lower limb. Noted with a retrocecally located appendix.
- Razdolsky's symptom. Careful tapping with a hammer or a bent finger on the right causes pain. This is the earliest symptom.
- Rovsing's symptom. A push in the left iliac region causes increased pain in the right region due to the displacement of gas and stretching of the cecum.
- Sitkovsky's symptom. If a patient lying on his back or right side is turned to the left, he will either develop or intensify pain on the right side below.
- Yaure-Rozanova symptom. Pain appears when pressing with a finger in Petit's triangle.
Gabai proposed to define the Shchetkin-Blumberg symptom in the Petit triangle.
In all doubtful cases, it is better to go for a diagnostic laparotomy than to miss appendicitis, the symptoms of which can often be atypical and allow the development of peritonitis. A clinical picture similar to acute appendicitis is given by typhlitis, terminal ileitis (Crohn's disease), Meckel's diverticulitis, but differentiation in most cases is achieved only during surgery. Differential diagnostics in most cases has to be carried out precisely with pathology of the female genital tract, and gynecologists, even after consulting the patient, again return her to the surgeon with the requirement to exclude appendicitis. In this case, several fairly informative symptoms are used.
- Zelheim's symptom. On digital rectal examination, thickening, tension and tenderness in the right uterosacral ligament indicate salpingitis.
- Karla symptom. The patient is asked to lie on the left side, and pressure is applied to the McBurney point (in the middle of the spinous-umbilical line). In acute appendicitis, the patient experiences pain, but there will be no pain in salpingo-oophoritis.
- Kruglova symptom. With appendicitis, the ESR growth is slow, with inflammation of the appendages it is very fast.
- Posner's symptom. During a vaginal examination, the cervix is grasped with two fingers and pendulum-like movements are made. In diseases of the female genital area, quite sharp pain appears.
- Promtova symptom. When examining through the rectum, press on the bottom of the Douglas space. With acute appendicitis, pain appears, and with inflammation of the appendages there will be no pain, but it will appear when the uterus is lifted.
What research can help?
Specialized investigations to confirm the diagnosis of acute appendicitis are rarely required, and the diagnosis is primarily clinical. There is no specific diagnostic test for appendicitis, but judicious use of simple urine and blood tests, especially of inflammatory response, should allow other pathologies to be excluded and provide additional evidence to support the clinical diagnosis of appendicitis.
Investigation of acute appendicitis:
- Urine analysis - up to 40% may have deviations.
- Pregnancy test – to rule out pregnancy.
- General blood analysis: neutrophilic (>75%), leukocytosis predominates in 80-90%.
- C-reactive protein - may be elevated, but its absence should not exclude the diagnosis of appendicitis.
The mandatory examination complex includes blood tests with calculation of LII, urine, blood biochemistry. Moreover, in doubtful cases, dynamic observation and repeated studies are mandatory. In very doubtful cases and for differential diagnostics with pathology of the female genital area, a puncture of the posterior vaginal fornix or laparoscopy can be performed; ultrasound and radiological methods, including laterography, are uninformative.
Currently, diagnosis is made using helical CT and stepwise compression color Doppler.[ 5 ] Diagnosis can be made based on persistent right lower quadrant pain and a visualized appendix greater than 6 mm in diameter.[ 6 ] New studies point to the efficacy of MRI, reporting a sensitivity of 96–96.8% and a specificity of 96–97.4%.[ 7 ],[ 8 ] The incorporation of this new modality will allow patients such as children to avoid exposure to radiation and intravenous contrast while maintaining diagnostic accuracy. This discovery foresee future first-line testing in children and possibly the general population.
The Alvarado scoring system is one of the most commonly used scoring systems to determine the need for surgical intervention in appendicitis.
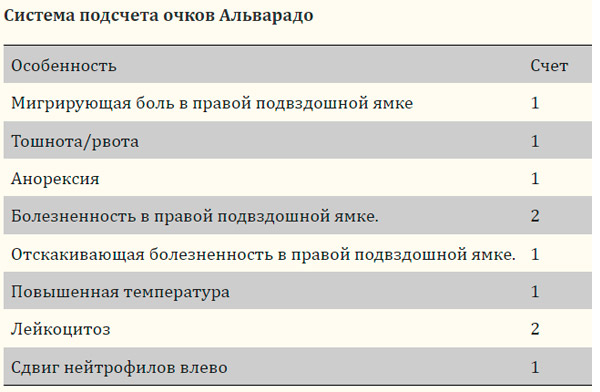
A score of 1–4 indicates “discharged home,” 5–6 indicates “observation,” and 7–10 indicates the need for “urgent surgery.”[ 9 ] The sensitivity and specificity of the Alvarado scoring system are reported to be 93.5% and 80.6%, respectively.[ 10 ] A simplified scoring system, known as the appendicitis inflammatory response scoring system, includes eight variables. These variables are vomiting, right lower quadrant pain, rebound tenderness, muscle guarding, white blood cell count, neutrophil percentage, C-reactive protein (CRP), and body temperature.[ 11 ]
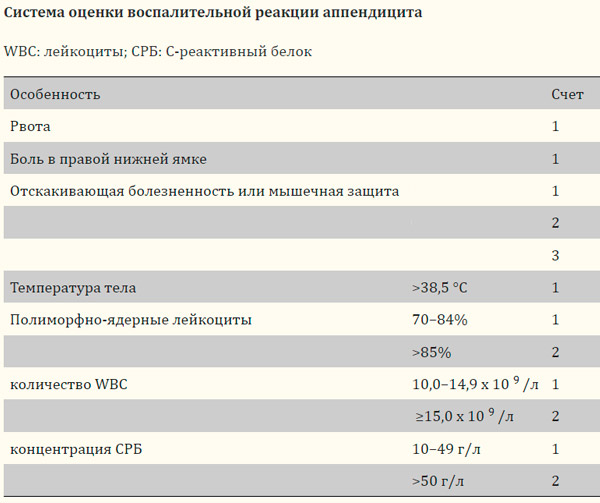
A score of 0–4 suggests “discharge home,” 5–8 indicates “observation,” and 9–12 indicates the need to “undergo surgery.” In a study comparing the appendicitis inflammatory response scoring system with the Alvarado scoring system, the sensitivity of the appendicitis inflammatory response scoring system was 93% compared with 90% using the Alvarado scoring system, with specificity being 85% compared with 55%, respectively. [ 12 ]. Other scoring systems have emerged, including the Fenyo, Eskelinen, Tzakis, and Raja Isteri Pengiran Anak Saleha Appendicitis (RIPASA). [ 13 ]
Differential diagnostics are carried out very carefully in cases of abdominal pain in children, especially in the presence of angina or tonsillitis, in which abdominal pain is caused by mesadenitis and solaritis.
Differential diagnosis of acute appendicitis
Surgical reasons
- Intestinal obstruction
- Intussusception
- Acute cholecystitis
- Perforated peptic ulcer
- Mesenteric adenitis
- Meckel's diverticulitis
- Colonic/appendicular diverticulitis
- Pancreatitis
- Rectus sheath hematoma
Urological causes
- Right ureteral colic
- Right-sided pyelonephritis
- Urinary tract infection
Gynecological causes
- Ectopic pregnancy
- Rupture of ovarian follicle
- Inverted ovarian cyst
- Salpingitis/Pelvic Inflammatory Disease
Therapeutic reasons
- Gastroenteritis
- Pneumonia
- Terminal ileitis
- Diabetic ketoacidosis
- Pre-herpetic pain in the area of the 10th and 11th spinal nerves on the right.
- Porphyria
Who to contact?

