
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Infarction of the spleen
Medical expert of the article
Last reviewed: 04.07.2025
A complex disease – splenic infarction – is a condition in which focal tissue death of the organ is detected. Such a pathological process can be provoked by various factors, and not only the spleen suffers, but also the patient’s body as a whole.
The spleen acts as a kind of filter and directly affects the state of the immune system. When it is damaged, the work of all internal systems deteriorates, and the patient feels the problem almost immediately. However, an infarction of this organ is dangerous because with minor damage, symptoms may be virtually absent. Why does the disorder occur, how to prevent, recognize and treat it? You can find out about this from our article.
Epidemiology
The spleen is a vital organ necessary for normal immune defense and hematopoiesis. In a healthy person, the spleen weighs approximately 150 g and measures approximately 11 cm. This organ is difficult to palpate, meaning that it can usually be felt only when it is pathologically enlarged and extends beyond the costal arch.
The physiological functions of the spleen are as follows:
- elimination of microorganisms and antigens from the circulatory system;
- production of IgG, tuftsin and factor P;
- use, processing of pathological erythrocytes;
- embryonic hematopoiesis.
The spleen acts as a depot for a third of all platelets in the body and a large number of neutrophils, which are produced in response to infectious pathology or bleeding.
Splenic infarction is a fairly common pathology, although the foci of the disease are in most cases small. For example, in the United States, the incidence rate is from 2 to 5% among all diseases of the organ. The probability of mortality depends on many factors - in particular, on the size and number of foci of tissue necrosis. [ 1 ]
The pathology is equally often found in male and female patients, but more often affects elderly people over 60 years of age.
The mortality rate for splenic infarction is no more than 2%.
The disease can be detected by doctors of different profiles. Most often, the pathology is diagnosed by gastroenterologists, therapists, hematologists, surgeons, immunologists, and infectious disease specialists. It is to these specialists that patients most often turn when the first symptoms of the disorder appear.
Causes spleen infarction
In general, splenic infarction is a process of circulatory or angiogenic tissue necrosis, which may be a consequence of thrombosis, embolism, or prolonged spastic state of the vessels. When blood flow through the arteries is disrupted, an acute reaction occurs in the form of organ ischemia, which leads to the death of part or all of the spleen.
Causes of splenic infarction may include:
- diseases of this organ itself (torsion, cystic formations, or other pathologies that are accompanied by increased pressure in the vessels, trophic disorders, and ischemic processes);
- infectious or parasitic lesions, infectious toxic shock (circulatory disorders, septic conditions, vascular spasm);
- injuries complicated by closed or open damage to abdominal organs, damage to the integrity of the ribs (development of vascular embolism);
- vascular pathologies of a systemic or inflammatory nature that can narrow the lumen and block the vessel, causing the formation of a thrombus (a thrombus rupture can lead to the development of embolism of the splenic vessels); [ 2 ]
- heart diseases that negatively affect the quality of blood circulation and contribute to increased thrombus formation (endocarditis, heart defects, arrhythmia, infarctions); [ 3 ]
- blood picture disorders (accelerated clotting, long-term use of oral contraceptives, anemia, etc.); [ 4 ]
- malignant blood diseases (leukemia, lymphoma, malignant granuloma).
Infarction of the spleen is observed against the background of complete or incomplete occlusion of the organ artery or its auxiliary branches due to narrowing or blockage. [ 5 ]
Risk factors
Age is considered one of the prognostic unfavorable factors for the development of splenic infarction, since the disease is much more common in older people. Most cases of the pathology are diagnosed in patients over 60 years of age.
The following negative factors also increase the risk of developing splenic infarction:
- diseases or disorders of the cardiovascular system;
- congenital immune disorders, immunodeficiency states;
- tendency to thrombosis;
- atherosclerosis;
- hematological diseases.
If we consider risk factors that are related to people's lifestyle, the following can be particularly noted:
- smoking;
- the presence of a large amount of meat and fatty foods in the diet;
- drinking small amounts of liquids and plain water;
- excess weight;
- alcohol abuse.
Neutralization of the above-mentioned factors can help prevent the development of splenic infarction.
In some cases, doctors are unable to establish the true root cause of the disease, since the pathology can be provoked by several unfavorable factors at the same time, and it is not possible to single out any one of them. [ 6 ]
Most often the disease is associated with diseases of the cardiovascular system, typhus, traumatic injuries of internal organs, and mitral stenosis.
Pathogenesis
The spleen is an important and yet little-studied human organ. It is located in close proximity to the stomach, on the left side under the diaphragm.
The basic functional purpose of the spleen is to prevent infection from entering the body, participate in blood clotting processes, and cleanse the bloodstream of toxic components.
How does a disorder such as splenic infarction develop? Under the influence of provoking factors (in particular, spastic contraction of blood vessels, blockage by an embolus), oxygen transport to the organ deteriorates. Prolonged oxygen starvation of tissues entails the necrosis of part of them (if the branches of the artery are affected), or the entire spleen (if the basic arterial trunk is affected), which acquires a pale yellowish tint and signs of an inflammatory process.
An infarction may develop due to a violation of the integrity of any of the splenic vessels. Against the background of impaired arterial blood flow, collateral circulation continues to function, and excess pressure on the vascular walls appears. As a result, the membranes are damaged, and bleeding occurs. The organ tissue acquires a red "bloody" hue, zones of necrosis and infiltrates are distinguished. An infarction of the spleen significantly worsens its functionality, immune and endocrine processes are disrupted, and erythroleuko-lymphopoiesis suffers.
Symptoms spleen infarction
The clinical picture of splenic infarction can vary greatly: patients with small or single lesions may have no symptoms at all, while large or multiple lesions may present with acute, painful symptoms. [ 7 ]
One of the most common symptoms is pain localized in the upper left segment of the abdomen. Other common signs include fever, chills, chest pain radiating to the left shoulder area, nausea and vomiting.
The severity of symptoms is directly related to the scale of the pathological process. In mild cases, splenic infarction does not manifest itself at all, or makes itself known by constant fatigue and general malaise: since such symptoms are far from specific, they are often ignored or attributed to other existing diseases.
In more complex cases, the first signs become more indicative:
- acute pain in the area of the spleen projection, or in the left side of the abdomen, sometimes radiating to the left arm (shoulder);
- increase in body temperature;
- signs of general intoxication;
- dyspepsia (diarrhea, nausea, etc.);
- increased heart rate.
In case of massive splenic infarction, there is a sharp stabbing or cutting pain on the left side under the ribs, radiating to the area of the shoulder blade, lower back, and left chest. Diaphragmatic mobility decreases, diarrhea is replaced by constipation, and signs of intoxication increase. During palpation examination, an enlarged and painful spleen is detected.
With the development of complications (numerous abscesses, bleeding, pseudocystic formations), the clinical picture expands and worsens.
Forms
In medicine, the following types of splenic infarction are distinguished:
- By extent of damage:
- small focal;
- extensive.
- By the number of pathological foci:
- plural (numerous);
- single.
- By etiological factor:
- non-infectious;
- infectious (septic).
Depending on the type of damage to the splenic parenchyma, infarction is divided into the following types:
- Ischemic infarction of the spleen, or white infarction, develops against the background of blockage of the main artery of the organ or its branches that provide blood flow to the parenchyma. In the case when the reaction to the developing pathology is the formation of numerous "bypass" blood flow paths, the vascular bed loses its filling and collapses. Microscopically, this appears as paleness and yellowing of tissues, limitation of the peripheral area by inflammatory infiltrate.
- Hemorrhagic infarction of the spleen, or red infarction, develops as a result of blockage of the main arterial vessel and oversaturation of capillaries with blood. Dead tissues are saturated with blood, which is manifested by their bright red color. Another factor in the development of pathology can be venous congestion, with impaired blood outflow. Microscopic signs of the disorder are as follows: erythrocyte hemolysis, infiltrates and necrotic areas.
Complications and consequences
The intensity of the clinical picture depends on the extent of damage to the splenic tissue. Minor splenic infarctions often do not manifest themselves in any way and are not complicated. With large pathological foci and large-scale tissue necrosis, the patient's condition worsens, pain syndrome and intoxication develop:
- there is a feeling of heaviness under the ribs on the left;
- pain occurs (dull, sharp – depending on the lesion);
- the digestive process is disrupted (dyspepsia, flatulence, vomiting, etc.);
- breathing becomes difficult;
- the pulse quickens;
- body temperature rises (to high levels).
There may be an enlargement of the organ - splenomegaly, which can be detected already during the initial medical examination.
If the necrosis area becomes infected, an inflammatory process develops, a separate cavity is formed, inside which purulent masses accumulate. Such a complication is called an abscess. The clinical picture of an abscess is manifested by a strong intoxication syndrome, and its prognosis is very unfavorable: in the absence of timely treatment, the probability of the patient's death is close to 100%. [ 8 ]
When an abscess spontaneously opens into the abdominal space, peritonitis and sepsis develop.
Hemorrhagic infarction can be complicated by bleeding, as well as the formation of large pseudocysts.
Diagnostics spleen infarction
Diagnostic measures begin with a thorough medical examination: palpation is performed, anamnesis is collected. In all cases, additional diagnostics are required in the form of ultrasound, radiography, magnetic resonance imaging. Laboratory diagnostics are also mandatory.
After a preliminary examination, the doctor prescribes laboratory tests:
- general and biochemical blood tests;
- general urine analysis;
- PCR for detection of certain types of viruses (hepatitis B and C, cytomegalovirus, etc.).
Sometimes, in addition to PCR, an immunogram is prescribed - a complex analysis to assess the state of the immune system. However, the tests are not informative in all cases. In case of massive tissue damage and infectious and inflammatory reactions, suppression of hematopoiesis processes is detected, ESR increases, and there are signs of anemia.
The basic diagnostic method is palpation. Normally, the spleen should not be palpable, and the procedure itself is painless. In case of a heart attack, palpation is accompanied by unpleasant sensations, splenomegaly - an enlargement of the organ - may be noted. As a rule, the procedure is carried out in two positions: the patient lies on his back, and then lies on his left side, bending and pulling his right leg to his stomach. In this case, the right hand is placed behind the head, and the bent left hand is placed on the chest. Percussion is also performed simultaneously with palpation, which allows you to determine the size of the organ.
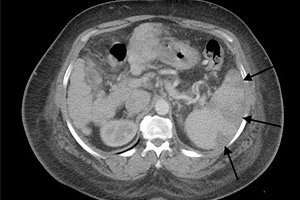
To clarify details, instrumental diagnostics are required:
- magnetic resonance imaging;
- computed tomography or multispiral CT;
- ultrasound examination;
- biopsy with further histological examination of the biopsy.
MRI is one of the most informative diagnostic methods. The procedure does not require special preparation. However, during pregnancy, as well as in the presence of pacemakers, metal implants, prostheses, MRI is contraindicated.
Among X-ray examinations, CT, or computer tomography, is the most informative. You should prepare a little for the procedure: do not eat food 4 hours before the diagnosis, and exclude from your diet foods that increase gas formation (cabbage, peas, etc.) two days before. CT may be refused to pregnant women, patients with severe cardiovascular diseases or obesity. [ 9 ]
Ultrasound examination is performed with preliminary preparation (as before CT), however, emergency diagnostics are also allowed. The main advantage of ultrasound is a reliable and fast result that does not require additional decoding.
Splenic infarction on ultrasound
The spleen is one of a number of organs that are well defined during ultrasound. The splenic parenchyma has greater echogenicity than the nearby kidney, but is approximately similar in echogenicity to liver tissue.
In a healthy person, the organ length can be 8-13 cm, with a thickness of up to 4.5 cm (sometimes up to five). A fairly common phenomenon is additional splenic lobes, which, however, most often do not have significant clinical significance.
In the case of splenic infarction, the ultrasound picture may not change at the initial stages. However, as the pathological process progresses, a hypoechoic zone is formed, which is the infarction focus. Over time, this zone may become hyperechoic. It decreases, acquiring the appearance of a small hyperechoic area. In the case of hemorrhage in the infarction area, the picture changes: the focus again acquires a hypoechoic appearance, or is a combination of hyper and hypoechoic areas. In case of repeated infarctions, a decrease in the size of the spleen may be observed, with numerous hyperechoic zones from previous injuries remaining.
Differential diagnosis
Pain in the spleen area is considered an important initial sign of several hematological and other pathologies at once, therefore it requires careful diagnosis, including differential diagnosis.
During palpation and examination, it is necessary to pay attention to many points. Thus, respiratory displacements of the organ allow identifying splenic pathology from tumor processes in the kidneys or pancreas. In case of slight splenomegaly, patients are examined in a lying position on the right side.
If the etiology of the disease is unclear or if the patient is overweight, they rely primarily on the results of ultrasound, which will demonstrate the structural picture of the affected organ. Computer tomography and splenic scintigraphy are also considered reliable research methods. [ 10 ]
It is important to focus on the size of the spleen. Infectious and inflammatory edemas are often accompanied by a soft consistency of the organ, and increased density and tightness may indicate long-term pathologies.
In general, differential diagnostics are carried out with the following diseases:
- circulatory disorders (portal hypertension syndrome);
- infectious and inflammatory processes;
- autoimmune pathologies, granulomatosis;
- hemolytic anemia;
- tumor processes in the spleen, cystic formations, metastases;
- lymphatic neoplasia;
- myeloid neoplasia;
- amyloidosis.
Among bacterial infections, differentiation is required for typhus, miliary tuberculosis, brucellosis, leptospirosis, and Lyme disease.
Among viral infections, it is necessary to exclude hepatitis A, B and C, infectious mononucleosis, cytomegalovirus, and AIDS.
Particular attention is required in the diagnosis of parasitic infections such as malaria, leishmaniasis, Chagas disease, etc.
Treatment spleen infarction
Latent asymptomatic course of splenic infarction (this is the overwhelming majority of cases) does not require surgery. The patient is observed and, if necessary, prescribed drug treatment:
- painkillers;
- anticoagulants;
- nonsteroidal anti-inflammatory drugs;
- symptomatic drugs. [ 11 ]
Some patients with isolated abscesses undergo percutaneous drainage followed by antibiotic therapy.
In case of extensive spleen infarction and development of complications in the form of numerous abscesses, bleeding, and pronounced pseudocysts, surgical treatment is performed – complete or partial resection of the organ.
The operation can be performed by conventional access (planned or emergency, depending on the situation) or by laparoscopy. In the second case, ultrasound or radiofrequency ablation is used to separate the parenchyma.
If possible, the surgeon removes only the damaged part of the spleen, preserving its function. This reduces the risk of postoperative complications and speeds up the recovery period.
After the operation, the patient is prescribed a restorative and rehabilitation course of drug therapy. The main drugs in this period are analgesics (Spazmalgon, Analgin), drugs that prevent increased thrombus formation (Warfarin), non-steroidal anti-inflammatory drugs (Ibuprofen), antibiotics (Ceftazidime, Erythromycin), and immunostimulants.
Surgical treatment
Surgical intervention for splenic infarction can be represented by splenectomy (laparoscopic splenectomy, or complete removal of the organ) or resection - an organ-preserving operation that involves preserving a section of functionally capable tissue.
Laparoscopic splenectomy is a modern type of surgical treatment that has many advantages:
- there is no need for large incisions, so there are no visible scars after the operation;
- minimal tissue damage;
- constant video surveillance during the operation;
- fast recovery period with minimal complications and low pain syndrome.
Removal of the spleen is considered a complex surgical intervention that requires not only highly qualified personnel, but also technically equipped hospital and operating conditions. During laparoscopy, it is possible not only to remove the diseased organ, but also to simultaneously perform a biopsy (if necessary).
The choice of treatment method remains with the attending physician, after a thorough study of the diagnostic results. [ 12 ]
After splenectomy, the spleen's functions are taken over by the bone marrow and liver. The patient is prescribed a special diet, exercise therapy, and the use of a bandage.
Postoperative recovery involves taking the following medications:
- analgesics and antispasmodics (Spazmalgon, Ketorol);
- antibiotics (macrolide series, cephalosporins, fluoroquinolones);
- nonsteroidal anti-inflammatory drugs (Ibuprofen);
- fibrinolytics (Fibrinolysin);
- anticoagulants (Heparin);
- means for supporting the immune system (interferons, Immunorix).
After splenectomy, patients experience a sharp weakening of the immune system, so they are advised to limit social activity, avoid crowded places, and not use public transport to prevent possible infection.
Prevention
Preventive measures to maintain the spleen in a healthy condition are generally simple: proper nutrition and a healthy lifestyle. This organ will function better with regular physical activity, as well as with systematic breathing exercises:
- Practice abdominal breathing, with a deep breath. Place your hands in the solar plexus area, tuck your thumbs and little fingers inward, and point the tips of the remaining fingers toward the central part of the plexus. Press on it with your fingers, and say "h-u-u-u" while exhaling.
- Stand freely, feet shoulder-width apart. Inhale and exhale softly, calmly. During inhalation, arms are crossed and raised to the chest. During exhalation, one arm is raised palm up, and the other is lowered palm down (as if expanding the space). Then arms are crossed again at chest level and the exercise is repeated, changing the order. During the exercise, on exhalation, pronounce "h-u-u-u".
- On inhalation, raise your arms forward, crossing your wrists at head level. On exhalation, lower your arms.
In addition to exercise, it is important not to self-medicate at any painful symptoms and to seek medical help in a timely manner.
A timely visit to a doctor will allow you to solve the problem at an early stage with minimal losses and disruptions.
What foods can harm the spleen? These are animal fats, salt, hot spices, alcohol, synthetic preservatives and flavor additives. Preference should be given to vegetable dishes, low-fat dairy products, and liquid porridges. Dishes made from beets, cabbage, apples, avocados, pomegranates, nuts, honey, and sour berries will be especially beneficial. In general, a properly organized diet will help protect your own health from many problems that, it would seem, do not depend on our food preferences. It is harmful to overeat and consume a lot of refined sugars. By the way, obesity is one of the risk factors for the development of many pathologies, including splenic infarction. [ 13 ]
Dehydration and insufficient fluid intake during the day are no less harmful. It is useful to drink both plain clean water and fruit and berry compotes, fruit drinks, natural juices, and herbal teas.
The spleen should be protected from injury, and any infectious processes in the body should be treated promptly.
Forecast
The outcome of the disease may vary, depending on the extent of damage, the timeliness of diagnostic and therapeutic measures. If there is a small spleen infarction, then with early medical attention and competent treatment, we can confidently talk about a favorable prognosis. A scar is formed in the area of tissue necrosis. The ischemic area often softens with the subsequent formation of a false cyst.
If the spleen infarction is significant in size, has complications in the form of a cystic or abscessing process, then there are risks of infectious spread and the development of septicemia. In such a development of events, emergency medical care must be provided. If this does not happen, the patient will die.
Growing dysfunction of the organ often becomes an indication for surgical treatment of splenic infarction. However, even after splenectomy, the risk of developing bacterial infectious pathologies, including sepsis, increases significantly, since patients with no spleen have a severely impaired immune defense. In addition, persistent lifelong changes in the blood picture occur - in particular, the number of leukocytes, reticulocytes and platelets increases.

