
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Skin grafting
Medical expert of the article
Last reviewed: 04.07.2025
Indications for the procedure
The main indications for skin transplantation are related to combustiology: if more than 10% of the body's skin is burned, then skin transplantation is performed after a 2nd degree burn, but most often it is necessary for 3rd degree skin burns, when the basal layer of the epidermis and all layers of the dermis are destroyed. And for 4th degree burns, a delayed transplantation is performed.
In traumatology, skin grafting is used to treat extensive wounds – lacerated, crushed, scalped – with a significant area and volume of damage. Such wounds cannot heal by primary intention, and their cavity is filled by fibroblast proliferation and the formation of granulation (connective) tissue.
Skin transplantation is performed for trophic ulcers – long-term non-healing inflammations with necrosis of the dermis and hypodermis caused by diabetes mellitus, varicose veins, obliterating thromboangiitis or thrombophlebitis of the lower extremities, lymphostasis or vasculitis.
In case of frostbite of the extremities, leading to the death of skin tissue, a skin graft on the leg (often on the feet of both legs) or a skin graft on the arm may be required.
Serious defects and deformations of the skin of the face and neck, including ulcers after phlegmon, are the main reasons for which skin grafting is performed on the face.
In all of the above cases, skin grafting is performed on the child, regardless of his or her age.
Reconstructive surgery – skin flap transplantation – helps improve the quality of life of patients after surgical removal of dermatological malignancies (most often melanoma), as well as patients with dystrophic bullous epidermolysis.
Is skin transplantation possible for vitiligo? This autoimmune dermatological disease with the formation of whitish spots on the skin is treated in some foreign private clinics by transplanting melanocytes (pigment-producing epidermal cells) from healthy areas of the skin to discolored spots, followed by exposure to an excimer laser. The method of cellular autotransplantation of cultured melanocytes is also used.
But skin grafting for stretch marks (striae) associated with atrophic changes in the skin is not provided: various local remedies and hardware methods are used to treat banded atrophoderma. Read more about them - Stretch marks: what causes them and how to get rid of them?
Preparation
In addition to the generally accepted preoperative examination, preparation for skin transplantation involves stopping the inflammation of the damaged surface (burn, wound, affected by trophic ulceration, etc.), which is completely cleared of pus and dead tissue by performing necrectomy. This requires a certain amount of time, during which patients are prescribed appropriate medications and physiotherapy, and a microbiological study of wound discharge (cytogram for the presence of pathogenic microorganisms) and monitoring of the state of granulation tissue in the wound bed is performed.
Also, to close the defect, it is necessary to prepare the transplanted material. If transplantation of a skin flap from the patient himself is possible (autotransplantation), then a flap of healthy skin is taken from him (using a special instrument - a dermatome).
Where is skin taken for transplantation? The main donor areas are the places from which the autotransplant is taken: buttocks, anterior abdominal wall, thighs (front and outer surfaces), chest (front and side surfaces), shoulders (upper parts of the arms from the shoulder joint to the elbow). The surgeons precisely determine the required size and thickness of the skin flap in advance - depending on the area and depth of the damage, as well as its location. Flaps can be either very thin (split, consisting of only a few epithelial layers), or thicker (full-layer, with a portion of subcutaneous fat).
To ensure that donor sites heal quickly and without complications after skin transplantation, bleeding is stopped and the wound surface is dried, onto which sterile bactericidal dressings with silver ions are applied: the micro-mesh of such dressings absorbs the secreted exudate without sticking to the wound, and promotes the formation of a dry scab, under which the wound heals.
When a thin flap is taken, a solution of potassium permanganate can be used to treat the donor area, followed by surgical collagen wound dressings. And narrow wounds after flap excision are usually sutured with the application of an aseptic pressure bandage.
In burn centers, donor sites are covered with lyophilized xenoderm grafts (from pig skin); they can also be used to temporarily cover extensive 2nd-3rd degree burns, and after some time, autografts are transplanted onto the wounds prepared in this way.
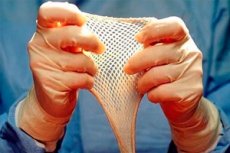
If it is impossible to transplant the patient's own skin, the skin of another person can be used - allogeneic transplantation (allogranistration). In addition, explants are used abroad - artificial skin for transplantation (Integra, Silastic, Graftskin), which is a collagen lattice frame (in some versions - with cultured human epidermal cells), which becomes a matrix for the ingrowth of fibroblasts, capillaries, lymphatic vessels and nerve fibers from healthy tissue surrounding the wound.
Based on innovative technologies of regenerative biomedicine, using mesenchymal stem cells of the blood and induced pluripotent stem cells of the bone marrow, it is possible to grow skin for transplantation after burns. But for now this is a rather lengthy and expensive process.
Technique skin grafts
The technique of transplantation is described in detail in the publication – Skin transplantation surgery after a burn
Before placing the flap in the wound bed, decompression necrotomy is performed (the resulting scab on the burn wound is dissected) followed by treatment with antiseptics.
In most cases, the transplanted autograft is held in place with a few small stitches or surgical staples. A drain is placed and a compression bandage is applied.
Experts note the peculiarities of the technique and donor sites when transplanting skin on the hands. Thus, for free skin transplantation in a child with burn injuries to the palmar surface, a full-layer flap is used, which is taken from the inner surface of the thigh. In adults, in the same cases, wounds are closed with flaps from any donor zones, as well as from the plantar side of the feet.
Skin grafting on fingers is often compared to fine work, and a variety of techniques are used here, the choice of which is dictated, first of all, by the localization of the damage and the presence of healthy tissues nearby. So both free autoplasty (with flaps on the back of the hand, from the shoulder, etc.) and non-free autoplasty can be performed - with cross flaps from undamaged phalanges, flaps on a feeding stalk, etc. If skin grafting is needed on the fingertips, it is performed with flaps of the patient's skin taken from the inner surface of the thighs.
A separate problem is post-burn scars, which disfigure the appearance and deform the limbs with joint contracture. When neither drug treatment nor physiotherapy methods give a positive result, skin transplantation is used. But this is not literally a skin transplantation onto a scar: first, the scar tissue is excised and only after that the defect is closed, most often by the method of moving counter (non-free) triangular flaps according to Limberg.
Skin grafting techniques
The main methods of skin transplantation are:
- free skin grafting, when the transplanted flap is isolated, that is, it is completely cut off from the place where it was cut;
- non-free skin grafting – either by transposition of partially separated fragments of healthy skin near the wound, or by means of a migrating (rotational) flap connected to the skin of the donor area by a so-called feeding pedicle. It is cut off only after complete engraftment of the transferred flap.
There is also a method of non-free autodermoplasty using a stalk flap - skin transplantation according to Filatov, when a stalk-shaped flap is formed from a longitudinal separated strip of skin (obtained by two parallel incisions), which is sutured along the entire length). The ends of such a "stem" are connected to the skin (in fact, these are two feeding legs), and when the flap is sufficiently vascularized, its distal end relative to the wound is cut off and sutured to the desired location.
Today, there are many modified versions of the Filatov method, first used at the beginning of the 20th century. Although earlier skin transplants according to Filatov were performed using techniques with Hacker and Esser flaps, and non-free scalp transplants were performed (and are still performed) with the Lexer flap.
The currently accepted classification of free skin grafting techniques includes:
- use of a full-thickness flap (the entire thickness of the skin), which allows for covering small but deep burns and wounds. Such autografts are used when skin transplantation is required on the face and distal parts of the extremities (feet and hands);
- restoration of lost skin in one area with one split (thin epithelial) flap;
- the use of a split flap divided into strips - skin grafting according to Thiersch;
- closing the defect with several isolated small flaps – skin grafting according to Reverdin (modified Yatsenko-Reverdin technique);
- transplantation of a split perforated flap, on which longitudinal rows of short interrupted incisions are made (with a brick-like offset). This allows the graft to stretch and cover a larger area, and also prevents the accumulation of exudate underneath it, which is extremely important for good survival of the flap.
Contraindications to the procedure
Medical contraindications for skin grafting include:
- shock or feverish state of the patient;
- burn toxemia and septicotoxemia;
- the presence of a local inflammatory process at the transplant site;
- significant blood loss;
- serous and serous-hemorrhagic diseases of the skin;
- elevated levels of protein fractions and/or leukocytes in the blood, low hemoglobin levels (anemia).
Consequences after the procedure
First of all, the consequences after the skin graft transplant procedure can be, as with any surgical intervention, in the form of a reaction to anesthesia, hematomas and swelling, bleeding, as well as the development of an inflammatory process due to infection.
Complications after the procedure include:
- destruction of the transplant (due to poor blood flow at the transplant site or accumulation of exudate);
- rejection of the skin flap (as a result of its inadequate preparation or non-sterility of the wound bed);
- deformation (wrinkling) of the transplanted flap (especially split) with a decrease in its size;
- increased pigmentation;
- coarse hypertrophic scars, scars after skin grafting (with limited mobility of the joints of the extremities);
- decreased sensitivity of the skin at the transplant site.
A complication such as a dent after skin grafting may be associated with either postoperative necrosis in the wound or the fact that the thickness of the skin flap did not correspond to the depth of the defect, or the level of granulation in the wound bed was insufficient at the time of grafting.
Care after the procedure
Postoperative care consists of dressings, taking prescribed medications (painkillers, antibacterials); depending on the condition of the surgical area, skin grafting treatment is performed using antiseptic solutions (for example, Furacilin, Dioxidine, Diosizol, Sodium deoxyribonucleate), as well as corticosteroids.
On what day does the skin take root after transplantation? The transplanted skin usually begins to take root three days after the operation. At first, the flap is nourished by plasma absorption, but after 48-72 hours - as it revascularizes (grows new blood vessels) - the trophism of the transplanted skin begins to be provided by microcirculation in the capillaries.
This process lasts at least three weeks, and how long it takes for the skin to take root after transplantation in each specific case depends on a number of factors. Firstly, the reason for resorting to this operation and the scale of skin loss play a role. The patient's age, the state of his immune system, the body's reparative reserves and, of course, the presence of certain diseases in the anamnesis are also important. The thickness of the transplanted skin flap is of great importance: the thinner it is, the faster it takes root.
To ensure that healing after skin grafting goes without complications, anti-inflammatory ointments can be used after skin grafting: Levomekol, Miramistin, Methyluracil, Dermazin (with silver sulfadiazine), Depanthenol. More information in the material - Ointments for wound healing
Skin grafting takes at least two to three months to heal, but may take longer. Patients should support the graft with compression stockings. In addition, grafted skin does not produce sweat or sebum, and should be lubricated daily for two to three months with mineral oil or another mild oil to prevent drying out.
Nutrition during skin transplantation should be complete, with an emphasis on animal proteins - to ensure the intake of amino acids and nitrogen-containing compounds. Of the microelements, zinc, copper, manganese, selenium are especially important during this period, and of the vitamins - retinol (vitamin A), pyridoxine (vitamin B6) and ascorbic acid (vitamin C).


 [
[