
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Rheumatoid arthritis and leg pain
Medical expert of the article
Last reviewed: 04.07.2025
Rheumatoid arthritis (RA) is a common autoimmune disease that can cause chronic inflammation of the joints, particularly the joints of the legs. This insidious disease can also cause inflammation and damage to internal organs. What are the causes of rheumatoid arthritis affecting the legs and how to deal with it?

Why does rheumatoid arthritis occur?
Rheumatoid arthritis can strike a person and cause pain in the legs and other organs when the body's tissues are mistakenly attacked by its own immune system. It contains a complex of cells and antibodies that are designed to "find and destroy" invaders of the body that cause various diseases, particularly infections.
People with autoimmune diseases have antibodies in their blood that aim to destroy their own tissues where inflammation occurs. This can affect other organs in the body, particularly the health of the legs. Rheumatoid arthritis is also called rheumatic disease.
The most dangerous age for patients who suffer from rheumatoid arthritis and leg pain is 20 - 50 years. Women's joints are much more often affected by such a disease as rheumatoid arthritis than men. This disease also does not spare children, usually affecting the knee joints. For men, changes in the joints of the feet, toes, knees and hips are more typical. For women, rheumatoid arthritis begins with pain in the hands, and then switches to the wrists, then the joints of the legs can hurt badly. However, there is no typical localization of pain for women - the extremities can be affected - both arms and legs.
What are the causes and risk factors for rheumatoid arthritis?
The causes of a disease such as rheumatoid arthritis are unknown. Although scientists have long suspected the influence of infectious agents such as viruses, bacteria and fungi, their influence has not been proven as a cause. In the field of world research, these causes are very actively investigated. It is believed that the tendency to develop rheumatoid arthritis can be genetically inherited.
Some genes that increase the risk of the disease have been identified. Some infectious diseases or environmental aggression can cause the immune system to activate in hypersensitive people. This is the immune system attacking the body's own tissues. This leads to inflammation in the joints and sometimes in various organs of the body, such as the lungs or eyes. Or the legs - which is most common.
It is not known what causes the onset of rheumatoid arthritis. Regardless of the exact trigger, the result is that the immune system is directed to promote inflammation in the joints and sometimes other tissues of the body. Immune cells called lymphocytes are activated and act as chemical messengers of tumor-causing cytokines, also known as necrosis factor, which are especially pronounced in inflamed areas of the body. In particular, the joints of the legs, which are very painful.
Environmental factors also play a role in the development of rheumatoid arthritis. For example, scientists have reported that smoking tobacco, exposure to silica in plants that we eat, and chronic periodontal disease significantly increase the risk of developing an insidious and dangerous disease such as rheumatoid arthritis.
Features of the course of the disease
Rheumatoid arthritis is a chronic disease, meaning it can last for many years, so people with the disease may experience the condition without any symptoms. However, rheumatoid arthritis is usually a progressive disease that tends to cause destruction of the joints of the legs and lead to functional disability.
A joint is where two bones meet to allow a person to move a limb, such as a leg. Arthritis of the legs is inflammation of the joints of the legs. Inflammation of our joints during rheumatoid arthritis causes swelling, pain, stiffness and redness in the joints. Inflammation can also last in the tissues around the joints, such as tendons, ligaments and muscles.
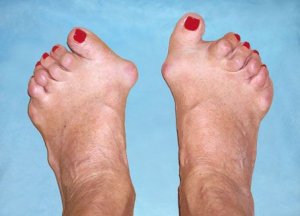
In some people affected by the disease, chronic inflammation leads to long-term destruction of cartilage, bones and ligaments, which eventually leads to joint deformation. Joint damage can be early in the disease and progressive. In addition, studies have shown that progressive damage to the joints of the legs does not necessarily correlate with the degree of pain, stiffness, swelling in the joints.
Rheumatoid arthritis is a common rheumatic disease that affects about 1.3 million people in the United States alone, according to current census data. The disease is three times more common in women than in men. Rheumatoid arthritis and the leg pain it causes affect people of all races equally.
This painful disease can affect a person's limbs at any age and even affects children (this is the so-called juvenile rheumatoid arthritis), but most often this disease begins at the age of 40-60 years. In some fairly athletic families, several people can be affected at once, which indicates a genetic cause for this autoimmune disorder.
 [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
[ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
What are the symptoms of rheumatoid arthritis associated with leg pain?
The symptoms of dangerous rheumatoid arthritis come and go depending on the degree of inflammation in the leg tissues. When the tissues are inflamed, the disease is active. When the inflammation of the leg tissues goes away, the disease becomes inactive (it is now in remission). Remission can occur spontaneously or can last for years, months, weeks. The symptoms of the disease during the remission stage may disappear, and people usually feel well. When the disease becomes active again (relapse), the symptoms of rheumatoid arthritis return.
The return of disease activity and its vivid symptoms is called a flare-up or attack. The intensity of leg pain varies depending on the general health of the affected individuals, with periods of flare-ups and remissions typical for leg pain.
When the disease is active, symptoms may include tired legs, general loss of energy, loss of appetite, low-grade fever, muscle and joint pain in the legs, muscle stiffness, and joint stiffness. They are usually most noticeable in the morning and after a period of inactivity.
During flare-ups of pain, the joints of the legs often become red, swollen, and painful. This is because the lining of the joint tissue becomes inflamed, causing excessive production of joint fluid (synovial fluid). The synovial membrane of the joint of the legs thickens and inflammation occurs (synovitis).
Symmetry of pain in the legs
Rheumatoid arthritis usually flares up in several joints of the legs symmetrically (on both sides of the body of the affected person). Early symptoms may be almost imperceptible. Small joints of the hands and especially the wrists are often involved in this process. People suffering from rheumatoid arthritis cannot perform even the simplest tasks of everyday life, such as turning a door handle and opening a can. Small joints of the foot are also often involved in the pain process, which can lead to painful walking, especially in the morning when a person has just gotten out of bed. Sometimes only one joint is inflamed.
When only one joint is involved in the pain process, joint inflammation caused by other forms, such as gout or joint infections, may occur. Chronic inflammation can lead to damage to body tissues, including the cartilage and bones of the legs. This leads to loss of cartilage, erosion and weakness of the bones and muscles, which leads to joint deformity, destruction and loss of function in the legs and arms.
Rarely, rheumatoid arthritis can severely affect the joint that is responsible for tightening our vocal cords to change the tone of our voice. When the joint becomes inflamed, it can lead to hoarseness. Symptoms in children with rheumatoid arthritis include limping, irritability, frequent crying, and poor appetite.
Human condition and rheumatoid arthritis
Rheumatologists also classify the functional state of people who suffer from rheumatoid arthritis, this happens as follows:
- Class I: The person is fully able to perform normal daily activities
- Class II: The person is able to perform normal activities for self-care and work, but is limited in activities outside of work (e.g., cannot play sports, do household chores)
- Class III: Able to perform normal self-care activities but has limitations in work and other activities
- Class IV: The person is limited in his or her ability to perform normal self-care activities, work, and other activities.
Another method your doctor may choose to diagnose the disease is called a joint puncture. In this procedure, sterile needles and syringes are used to remove joint fluid from the joint and are intended for testing in the laboratory.
A laboratory analysis of the joint fluid can help rule out suspected causes such as infections and gout. Sometimes cortisone medications are injected into the joint during a arthrocentesis to quickly relieve inflammation in the affected leg and provide further symptom relief.
Seropositive rheumatoid arthritis
Refers to diseases with unclear causes. Our body still remains a great mystery for scientists, which is difficult to solve even with high-tech equipment. Scientists, like doctors, can only assume that the main negative factors that trigger the mechanism in the body, as a result of which seropositive rheumatoid arthritis begins to develop, are:
- Virus attacks.
- Autoimmune processes (a failure in the immune system, in which the immune system fights its own cells).
- Hereditary predisposition.
- Age-related changes in the structure of joint tissue.
- Negative external factors.
- Harmful production.
- Increased stress on joints.
- Frequent bruises and injuries.
How to suspect seropositive rheumatoid arthritis
It is enough to be attentive to your body in order to react sensitively to all its signals. The human body is a supersensitive biological machine and it is capable of self-regulation, but with excessive and incorrect use, with a careless attitude to its resources, failures begin to occur that require specialized intervention.
The first signs that will allow you to suspect something is wrong with your joints begin to appear in the morning in the form of an unpleasant sensation in your arms and legs, stiffness of your fingers, and slight swelling. In the early stages of rheumatoid arthritis, there may not be any painful sensations as such. However, there is a constant slight increase in body temperature, weakness, and malaise. Closer to midday, the morning stiffness in your limbs goes away, but the next morning everything repeats itself again.
Course and clinical picture
It is almost impossible to predict the course of this disease. In some cases, seropositive rheumatoid arthritis may not show obvious symptoms for many years, limited to only minor pain in the joints in the morning and during stress on them. In other cases, the disease develops rapidly, deforming all small joints in a short time, including the cervical vertebrae, leading a person to disability.
Curved fingers and toes due to swollen and unnaturally deformed joints - this picture can be seen if you look closely at the hands of grandmothers in public transport or in stores, at markets. Often this disease is perceived as an integral companion of old age. But, as medical statistics show, young people also suffer from seropositive rheumatoid arthritis, and every year the age limit is getting lower, therefore, the disease is getting younger year after year.
It is worth knowing and remembering that seropositive rheumatoid arthritis is not only a joint disease. As it progresses, it can affect all connective tissue in the body, and it is part of all our organs. Thus, a patient who has been diagnosed with the above automatically falls into the risk group for developing diseases of the lymph nodes, liver, heart, spleen, lungs, and gastrointestinal tract.
Due to the fact that the digestive system is involved in the general pathological process, patients suffering from rheumatoid arthritis often experience dyspeptic disorders: nausea, often accompanied by vomiting, changes in stool, frequent bloating, intestinal pain.
The disease can be cured
If you consult a doctor already at the stage of morning unpleasant constricting sensations in the arms and legs, take all the necessary tests, including the determination of the rheumatoid factor in the blood, then timely treatment will allow you to make the necessary health adjustments and prevent further development of the negative process.
Even in the case when the treatment of the disease begins at later stages, a full recovery is also possible, but to achieve it you will need to spend more time, patience and show considerable endurance, going through all the procedures, observing the necessary strict rules of the daily routine, giving up your usual diet in favor of a strict therapeutic diet, maintaining an emotional background at a high level.
Unwavering faith in success is always of great importance in achieving recovery. Seropositive rheumatoid arthritis can be defeated - this is worth knowing and remembering.
Seronegative rheumatoid arthritis
One of the types of joint damage based on the principle of arthritis. Only professionals are able to distinguish between seronegative rheumatoid arthritis and seropositive. For a person without medical education, it is enough to know that the negative one develops rapidly, without the preliminary stage of morning stiffness in the limbs.
Symptoms and diagnostics
If we consider more detailed differences in different forms, it is worth noting that at the beginning of the disease only one joint suffers, and if several, then there is no symmetry of the location of the affected areas, which is typical for ordinary arthritis. The onset of the disease from one knee joint is also a distinctive and indicative factor that allows us to exclude ordinary arthritis. Many joints are susceptible to damage, but ultimately, the most favorite place of localization of this form is the wrist joints.
In laboratory studies of blood analysis, an important and significant indicator is the absence of the rheumatoid factor against the background of the presence of other high indicators characterizing the presence of a strong inflammatory process in the body. Suffice it to say that with other forms of rheumatoid arthritis, the blood test gives positive results for rheumatoid tests.
When making a diagnosis, they rely mainly on laboratory data from blood tests and X-ray images of the affected joints, which clearly show changes both in the joint itself and in the adjacent bone part.
Treatment and prognosis
Seronegative rheumatoid arthritis is also characterized by increased complexity in terms of treatment. In order to select the main components for basic treatment, it is necessary to approach strictly individually, because standard treatment regimens for the classical form do not work properly with this type, despite the fact that the general principle of treatment is preserved. The whole difficulty is in the high probability of developing side effects from taking many medications, which significantly complicate the treatment algorithm.
The general prognosis of this disease largely depends on age characteristics, the presence of other types of chronic processes, and the stage at which treatment was started. In general, it is not always possible to achieve complete recovery.
Classification of types of arthritis
The American College of Rheumatology has developed a rheumatoid arthritis classification system based on X-rays of the joints. This system helps health care professionals classify the severity of rheumatoid arthritis in relation to cartilage, ligaments, and bones.
Stage I
- Joints and bones are intact and visible on x-rays, although there may be signs of bone thinning.
Stage II
- X-rays show thinning of the bones around the joint or minor bone damage
- minor cartilage damage is possible
- joint mobility may be limited, there are no deformations, but there is
- atrophy of adjacent muscles
- soft tissue damage is visible
Stage III
- X-rays show damage to cartilage and bone tissue and thinning of the bones around the joint
- joint deformation and extensive muscle atrophy
- soft tissue disorders around cartilage
Stage IV
- X-rays show damage to cartilage and bone tissue and osteoporosis
- joint deformation with permanent fixation of the joint (called ankylosis)
- extensive muscle atrophy
- soft tissue disorders around joints
 [ 11 ]
[ 11 ]
Complications of Rheumatoid Arthritis
They arise because the disease is mainly of a protracted nature. Any pathological process occurring in the body cannot be limited to any one area. Complex systems of interaction of life cycles, which make up the entire body as a whole, are subject to constant destructive action of foreign agents, which leaves an imprint in the form of a rupture or disruption of the exchange of useful substances, a failure in normal functionality.
The main complications of rheumatoid arthritis affect a fairly large part of organs and systems. This list includes diseases:
- skin (ulcerative vasculitis, rheumatoid nodules, dermatitis).
- eyes (from minor redness to severe inflammation of the eyeball, leading to loss of vision).
- cardiovascular system (pericarditis, both chronic and exudative, infarction, stroke, vasculitis).
- blood (anemia, thrombocytopenia).
- lungs (pleurisy, rheumatoid nodules in the lung tissue)
In addition to the complications listed, patients have increased susceptibility to infectious diseases and decreased emotional defense, which manifests itself in the form of frequent depression.
In other words, complications of rheumatoid arthritis cover all spheres of our body's activity. Against the background of taking medications, each new symptom, sensation, should be discussed with the attending physician, perhaps the problems that have arisen are related to a specific drug and its replacement is necessary.
What complications does rheumatoid arthritis cause to leg function?
Rheumatoid arthritis is associated with an increased risk of heart attack, and the heart is closely linked to leg function, which is also affected. Rheumatoid disease can reduce the number of red blood cells in the blood (causing anemia). A decrease in white blood cells can be associated with an enlarged spleen (called Felty's syndrome) and an increased risk of infection.
Lumps under the skin (rheumatoid nodules) can occur around the elbows and fingers where they experience pressure. Although these nodules usually do not cause symptoms of pain, they can become infected. Rarely, serious complications of rheumatoid arthritis include inflammation of the blood vessels of the legs (vasculitis). Vasculitis can disrupt blood flow to tissues and lead to tissue death, particularly in the legs (necrosis). They are most often first visible as tiny black spots around the nails or as ulcers on the legs.
How is rheumatoid arthritis of the leg joints diagnosed?
There is more than one test to diagnose rheumatoid arthritis of the legs. Rheumatoid arthritis of the legs is diagnosed based on a combination of joint diagnostics, joint stiffness in the morning that is characteristic of arthritis, the presence of rheumatoid factor and citrulline antibodies in the blood, as well as rheumatoid nodules and radiographic changes (X-ray testing).
The first step in diagnosis is the interaction between the patient and the doctor. The doctor analyzes the history of symptoms, examines the joints of the legs, the possibility of their inflammation, pain, swelling, deformation of the skin in the area of rheumatoid nodules (firm bumps under the skin, most often on the elbows or between the toes), as well as other parts of the body with inflammation.
Certain blood tests and x-rays often provide definitive information about rheumatoid arthritis of the joints of the legs. The diagnosis is based on the pattern of symptoms, the distribution of swelling in the inflamed joints, and blood and x-ray studies. Several visits to the doctor may be necessary before the doctor is confident of the diagnosis. A doctor with special training in diagnosing and treating arthritis and related diseases is called a rheumatologist.
Making a diagnosis
The distribution of inflammation in the joints of the legs is very important in making a diagnosis. Small joints of the wrists, hands, feet and knees usually have a symmetrical distribution of inflamed areas. This is rheumatoid arthritis that affects both sides of the body, i.e. symmetrical. In the case of leg diseases - both legs.
When only one or two joints in the legs become inflamed, diagnosing a condition such as rheumatoid arthritis becomes increasingly difficult. To be sure, your doctor may order other tests to rule out arthritis due to infection or gout. Finding rheumatoid nodules (described above), most often around the elbows and fingers, may help suggest the diagnosis.
Abnormal antibodies can be found in the blood of patients suffering from a disease called rheumatoid arthritis. Antibodies called "rheumatoid factor" (RF) can be found in 80% of people with this disease. Patients who have rheumatoid arthritis and do not have a positive rheumatoid factor test are referred to as having "seronegative rheumatoid arthritis". Citrulline antibodies (also known as anticitrulline) are present in most women and men with this disease.
It is useful for diagnosing a disease such as rheumatoid arthritis when evaluating cases of unexplained joint inflammation. The citrulline antibody test is most useful in finding the cause of previously undetected non-inflammatory arthritis when a traditional rheumatoid arthritis blood test shows nothing at all. Citrulline antibodies are a good indicator of this disease in the early stages of the disease. Other antibodies called "antinuclear antibodies" (ANA) are also common in people who have rheumatoid arthritis.
 [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ]
[ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ]
Erythrocytes in diagnostics
The ESR (erythrocyte sedimentation rate) blood test is a measure of how quickly red blood cells fall to the bottom of a test tube. This test is used as a measure of joint inflammation. This test is usually more useful during flare-ups and the rate of red blood cell fall is slower during remissions. Another blood test used to measure the amount of inflammation in the body is the C-reactive protein. The blood test can also detect anemia, as anemia is common, particularly due to the frequent chronic inflammation of the joints of the legs.
Rheumatoid factor, ANA, erythrocyte sedimentation rates, and C-reactive protein tests may also be suboptimal for diagnosing other systemic autoimmune and inflammatory diseases.
Thus, abnormalities in these blood tests alone are not sufficient to diagnose rheumatoid arthritis.
X-rays may be indicative or may only show soft tissue swelling in the early stages of arthritis. As the disease progresses, X-rays may show bone erosions typical of rheumatoid arthritis of the joints.
X-rays may also be helpful in monitoring the progression of the disease and damage to the joints of the legs. Procedures using a small amount of radioactive material may also be used to show inflamed joints. MRI scans may also be used to show damage to the joints.
Differential diagnosis of rheumatoid arthritis
It is mainly carried out with other types of arthritis, in particular, with the reactive form. In addition, work is carried out on a thorough examination in order to exclude osteoarthrosis. Thus, we get two diseases that can give related symptoms, increasing the likelihood of an incorrect diagnosis - these are reactive arthritis and osteoarthrosis.
When considering these three diseases within the framework of differential diagnostics, a comparison is made of the existing symptoms and complaints with the presence and characteristic nature of these symptoms in related diagnoses.
The most convenient way to explain is to use a specific example. Let's look at some data that is important for making an accurate diagnosis and compare them across three diseases. So, we are interested in:
- Age of the patient.
- Severity of joint pain.
- Presence of morning stiffness in the limbs.
- Symmetry of joint damage.
- ESR indicators.
- Presence of rheumatoid factor in the blood.
These indicators in three cases will be, by and large, different. In such a disease as rheumatoid arthritis, the picture will be as follows: the patient's age is average or slightly above average, severe pain in the joints, with the presence of a feeling of stiffness in the limbs in the morning. The joints are affected symmetrically. The ESR in the blood is excessively high. The rheumatoid factor is positive in the seropositive form of the disease.
We will consider the same indicators for two other diseases through an apostrophe, in sequence - reactive arthritis osteoarthritis:
- Age: young-senior.
- Severity of joint pain: intense-moderate.
- Presence of morning stiffness in the limbs: moderate, absent.
- Symmetry of joint damage: completely absent, not expressed.
- ESR indicators: increased within normal limits.
- Presence of rheumatoid factor in the blood: absent in both cases.
We have not considered all the key indicators on the basis of which differential diagnostics of rheumatoid arthritis is carried out, but for a general understanding of the process itself, the given example is quite sufficient. Similar comparative analysis of symptoms is carried out for all types of diseases. This method allows you to exclude from the list of possible diagnoses a large number of those that do not fit the objective picture of the disease, which in turn gives the right to make a correct diagnosis without a doubt and prescribe adequate and appropriate treatment.
 [ 27 ]
[ 27 ]
Methotrexate for Rheumatoid Arthritis
Methotrexate has been effectively used for more than a decade in rheumatoid arthritis and has shown excellent results in achieving relief of the main symptoms of the disease. The method of treating rheumatoid arthritis based on the drug group - metabolites, which have an antitumor effect and are aimed at suppressing inflammatory processes, is good because methotrexate, which is the leading representative of this group, tends to accumulate directly in the joint tissue, which has a direct effect on the inflammatory process, suppressing all negative manifestations.
The drug methotrexate is very fast-acting, the first positive results can be seen by the end of the third week of its use. Like any medication, methotrexate has, in addition to indications for use, contraindications, individual intolerance and a number of restrictions that should not be ignored.
The group of people who are contraindicated methotrexate in rheumatoid arthritis includes patients suffering from all types of diseases of the blood, liver, stomach and duodenum (mainly ulcers), infectious diseases, both acute and chronic. A special group, when prescribing any drugs, are pregnant women and nursing mothers. For treatment during the period of change and after childbirth should be carried out only according to individual gentle schemes.
When taking methotrexate, in the absence of contraindications, one should not exclude the occurrence of its side effects, among which the most common are:
- nausea, less often vomiting;
- allergic reactions;
- problems with the liver and pancreas;
- anemia;
- changes in blood composition, in particular thrombocytopenia;
- interstitial pulmonary fibrosis, a rare but very serious consequence of taking methotrexate. This disease is an irreversible process that is difficult to cure.
Indications for the use of methotrexate should be substantiated by the attending rheumatologist. In addition to the main drug, the role of which is assigned to methotrexate, a number of concomitant drugs are required that will maximally balance the negative effects of methotrexate, enhancing its positive effects.
Folk remedies for rheumatoid arthritis
A long struggle with serious illnesses makes people resort to searching for various methods of treatment. Folk remedies are often considered as a saving straw for someone drowning in a deep pool. One of the most popular queries in Internet search engines is rheumatoid arthritis treatment with folk remedies.
Rheumatoid arthritis is indeed one of the most complex diseases, both in terms of symptoms and treatment. People spend many years in unsuccessful search for the most effective treatment methods, taking a large number of medications and agreeing to complex injections and surgeries.
However, there are folk remedies that, according to many who have been cured with their help, help to remove the main symptoms of the disease quite quickly. How correct is such an approach to solving the problem? Probably, this is a purely personal matter. As they say, if necessary, knock on all the doors, somewhere, and they will open. Therefore, we can name several recipes that, even if they do not bring visible results, will certainly not cause harm.
If you or a loved one has rheumatoid arthritis, treatment with folk remedies is as follows:
- For rubbing: take 150 ml of turpentine, 70% alcohol, olive oil. Add 3 ml of camphor. Mix all components. Rub twice a day, morning and evening. After rubbing, it is advisable to wrap the joint with elastic cloth for several hours.
- Mix camphor and mustard powder (50 grams of each component), pour in alcohol (100 ml). In a separate bowl, beat the egg white, the total weight of which is approximately 100 grams. Combine with the alcohol mixture of camphor and mustard powder. Apply daily, twice a day, rubbing small portions into sore joints. The mixture should be stored in the refrigerator for no more than three days.
- Paraffin compresses for sore joints are prepared as follows. Take medical paraffin and melt it in a water bath. Add goose fat and camphor in equal parts. Before applying the paraffin mass to the sore joints, spread an anti-inflammatory or pain-relieving ointment, a medicinal cream - those products that are most often used to lubricate joints, and then apply the paraffin.
Cover the paraffin with cellophane film, wrap it with warm cloth, leave it on the joints for an hour. After removing the paraffin, apply the healing ointment to the joints again.
There are many folk recipes that recommend the use of a variety of remedies, which sometimes quite unexpectedly appear as healing. Anyone who sets himself the goal of finding folk remedies for an illness will certainly find at least a hundred ways to recover based on improvised means.
Let us stipulate once again that this is a personal matter for everyone, it is only worth remembering that our body is a sensitive machine that reacts unpredictably to interference in its work. So, before experimenting, entering the query rheumatoid arthritis treatment with folk remedies, it would be nice to get advice from a professional. And if you make a choice in favor of folk remedies, then let them be recommended to you by proven people, for example, phytotherapists.
 [ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ]
[ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ]
Diet for Rheumatoid Arthritis
Its super task is to ensure sufficient content of the components necessary to support the body. The main restrictions concern salt, proteins, carbohydrates and fats of animal origin. Completely refuse sweets during the period of exacerbation. Adults are advised to avoid alcohol.
Special attention should be paid to foods with a high content of vegetable fats, low-fat dairy products, cottage cheese, vitamins, especially groups B, PP, C. Introduce more fruits, vegetables and berries into the diet, use fruit and vegetable or fruit and berry juices as drinks, without added sugar.
It is good to diversify the menu with fish dishes, porridges, especially buckwheat. Bread on these days should be made from bran or coarse flour. White bread, like bakery products, is contraindicated.
A proper and strict diet during the treatment of rheumatoid arthritis greatly contributes to the speedy recovery of the body. In some cases, a diet for rheumatoid arthritis is the only way to solve an important problem that can greatly slow down recovery - getting rid of excess weight.
Rheumatoid Arthritis Facts
- Rheumatoid arthritis is a dangerous autoimmune disease that can lead to chronic inflammation of the joints of the legs and other parts of the body.
- Rheumatoid arthritis can affect people of all ages.
- The causes of a disease such as rheumatoid arthritis often remain unknown.
- Rheumatoid arthritis of the joints of the legs is a chronic disease characterized by periods of outbreaks of the disease and then its remission.
- Rheumatoid arthritis is characterized by several joints in the legs often, but not always, being affected symmetrically.
- Chronic inflammation can lead to irreversible joint damage and deformation.
- Damage to the joints of the legs can occur early and does not correlate with the severity of symptoms.
- "Rheumatoid factor" is an antibody that can be found in the blood of 80% of people with rheumatoid arthritis of the joints of the legs.
- Treatment for the insidious disease rheumatoid arthritis involves a combination of medications, rest and exercise, and sometimes surgery.
- At the beginning of treatment of a disease such as rheumatoid arthritis, which affects the joints of the legs, it leads to better results than in its chronic form.

