
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Uterine perforation
Medical expert of the article
Last reviewed: 04.07.2025
Uterine perforation is an accidental injury to the uterus, a rare but dangerous obstetric emergency. It occurs in approximately 1 in every 250 (0.4%) abortions.
The main symptoms are: lower abdominal pain, heavy vaginal bleeding, bloating, nausea, vomiting, chills, fever and rapid heartbeat. Ultrasound is used to confirm the diagnosis.
Causes uterine perforation
Among the causes of intra-abdominal bleeding, a certain place is occupied by perforation of the uterus during medical manipulations in its cavity. Most often, this occurs during an artificial abortion and during the removal of the remains of the fertilized egg in women with spontaneous or criminal miscarriage, but perforation of the uterus can also occur during diagnostic curettage of the uterine mucosa, hysteroscopy, and the insertion of an intrauterine contraceptive.
Induced abortion is the most common gynecological operation. Despite the apparent simplicity and speed of performance, it is fraught with great danger, which experienced specialists are well aware of and young novice doctors forget. Perforation of the uterine wall is one of the most serious complications of this operation. The frequency of uterine perforation ranges from 0.03 to 0.5%. At present, these figures have not only not decreased, but have even increased somewhat. It is apparently impossible to completely eliminate this complication. Having improved the doctor's qualifications, clearly limiting the pregnancy period, choosing the most rational intervention technique, it is impossible to influence such risk factors as the woman's age, previous diseases of the reproductive system, uterine hypoplasia, myoma, developmental defects, etc. Recognition of the leading role of morphological changes in the tissues of the uterine wall should not calm the doctor, disarm him in the face of the fatal inevitability of such a complication. On the contrary, it should mobilize the attention of the operator before each intrauterine intervention. If this does not prevent injury, maximum concentration helps the doctor to recognize it in a timely manner.
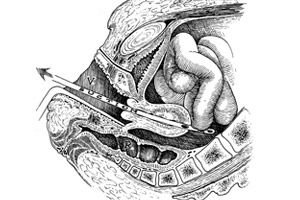
Uterine perforation may occur at any stage of the operation: during uterine probing, expansion of the cervical canal, emptying of the cavity. A distinction is made between uncomplicated perforations (without damage to adjacent organs) and complicated ones (with injuries to the intestines, omentum, bladder, uterine appendages, etc.).
Uterine perforations caused by a uterine probe are rare (2-5%) and pose the least danger, as they are usually not accompanied by profuse bleeding and injuries to adjacent organs. Trauma caused by Hegar dilators is somewhat more frequent (5-15%), the perforation opening is usually localized in the supravaginal part of the cervix, isthmus, and lower part of the uterine body. Intra-abdominal bleeding or hematoma between the layers of the broad ligament is observed much more often. Perforation of the wall by Hegar dilator is facilitated by excessive bending of the uterine body forward or backward, which the doctor did not pay attention to. Rough and hasty dilation of the cervical canal without using all dilator numbers, even without perforation of the uterus, can contribute to traumatization of the muscle layer in the area of the internal os. Ruptures of the internal os may be accompanied by significant bleeding from the cervical canal or lead to unfavorable long-term consequences - the formation of isthmic-cervical insufficiency.
The most frequent (80-90%) and dangerous uterine perforations are caused by manipulations with a curette and an abortion forceps. In this case, the perforation hole is usually located in the upper part of the uterus (fundus, anterior, posterior and lateral walls), the wound can be of significant size and be accompanied by profuse bleeding. The greatest danger in perforation of the uterus with a curette and especially an abortion forceps is trauma to the abdominal organs.
Where does it hurt?
Complications and consequences
The danger of the consequences of uterine perforation increases many times if this complication is not recognized in a timely manner. Meanwhile, the doctor's careful attention to all manipulations during the abortion almost completely eliminates the possibility of not noticing the perforation of the wall or its consequences.
Complications include inflammation of the abdominal lining (peritonitis), bowel or bladder injury, massive bleeding (hemorrhage), and infection (sepsis).
Diagnostics uterine perforation
Uterine perforation should be considered in cases where the instrument suddenly goes deep, as if falling through, without encountering resistance from the uterine wall. At this point, it is strongly recommended to stop all manipulations, “freeze,” without removing the instrument from the uterus, and try to palpate its end through the abdominal wall. This simple action helps to diagnose perforation in almost all cases. If the abortion operation is performed under local or conduction anesthesia, then the possibility of uterine perforation is indicated by sudden sharp pain. Complicated cases are sometimes recognized by removing the omentum, intestinal loop, ovary, etc. from the uterus. And, finally, careful, attentive observation of the woman’s condition by medical personnel in the first hours of the postoperative period helps to suspect uterine trauma that was not recognized at the time of the abortion. Signs of increasing internal bleeding or peritoneal symptoms force the doctor to perform an appropriate examination and make the correct diagnosis.
In all cases of uterine perforation during abortion, laparotomy, careful examination of all parts of the uterus and revision of adjacent pelvic organs and intestines are indicated. If a small defect in the uterine wall is detected, the scope of the operation is limited to suturing the wound after excision of its edges. First, it is necessary to scrape out the mucous membrane of the uterine wall through the perforation hole to prevent leaving parts of the ovum.
In the presence of large or multiple wall defects with damage to vascular bundles, with the formation of hematomas in the parametral tissue, it is necessary to perform supravaginal amputation, and in some cases - extirpation of the uterus. The scope of the operation is also expanded in cases where damage to the uterus occurs in women with myoma or adenomyoma.
In case of complicated uterine perforation, the operating gynecologist may encounter minor injuries to the bladder, intestine, omentum, which he will cope with on his own. However, having discovered extensive injuries to adjacent organs of the small pelvis or abdominal cavity, the gynecologist is obliged to resort to the help of appropriate specialists.
As often happens in the practice of a doctor, extreme situations, especially those of iatrogenic origin, are easier to prevent than to eliminate their consequences. Uterine perforation is no exception to this rule.
To prevent trauma to the uterus during an artificial abortion, it is necessary:
- do not perform surgery if the pregnancy period exceeds 12 weeks;
- It is essential to perform a bimanual examination immediately before the intervention to accurately determine the size and position of the uterus;
- It is imperative to apply bullet forceps to the anterior and posterior lips of the cervix: this simple technique when lowering the cervix ensures straightening of the angle between it and the body of the uterus;
- in no case should careful probing be neglected, with the help of which the length of the uterine cavity and the direction of the cervical canal are determined;
- carefully perform the dilation of the cervical canal: up to 8 weeks of pregnancy, it is advisable to use a vibratory dilator; Hegar dilators should be inserted in strict accordance with the numbering; rigid cervixes must be prepared by preliminary administration of antispasmodics or prostaglandins;
- evacuation of the fertilized egg at a pregnancy term not exceeding 8 weeks should preferably be carried out using a vacuum suction device; in some cases, use a curette, and use an abortion forceps only to remove detached parts;
- to perform the operation under adequate anesthesia not only in the interests of the woman, but also in order to create favorable conditions for the doctor’s work.
Uterine perforation may occur during diagnostic curettage performed due to suspected malignancy. In case of deep damage of the muscular layer by the cancerous process, perforation is performed without much effort of the operator. For better orientation in the state of the uterine cavity, diagnostic curettage should preferably be preceded by hysterography or hysteroscopy. The information obtained will allow tissue scraping to be taken with precision, maximum caution and, what is no less important, ablastically.
Uterine perforation may be a complication of intrauterine contraception. Most often, it occurs immediately at the moment of insertion of the IUD, especially if it is performed immediately after an abortion. However, perforation of the uterine wall may occur spontaneously. According to various authors, the frequency of perforations varies widely and depends on the form of the contraceptive. The frequency of uterine perforations is largely determined by the qualifications of the doctor.
Uterine perforation, even when it occurs at the time of IUD insertion, is not always easy to recognize. There are so-called silent perforations that do not manifest themselves immediately. It is even more difficult to diagnose spontaneous or secondary perforation.
The doctor must consider the possibility of uterine perforation if the woman experiences sharp pain during the insertion of the IUD. The possibility of this complication can also be assumed in cases where severe cramping pains persist for several days after the insertion of the IUD. Secondary perforation can be suspected if the woman complains of constant mild pain in the lower abdomen, while she did not notice the expulsion of the IUD, and the doctor does not detect the IUD threads in the vagina.
Expressed clinical signs of internal bleeding are rarely detected. Symptoms of limited or diffuse peritonitis appear quite late. Internal gynecological examination will not provide clear evidence of perforation. Therefore, modern hardware diagnostic methods are of primary importance: ultrasound examination, hysteroscopy and laparoscopy.
Accurate diagnostics of complete and incomplete perforation of the uterus by the IUD can be performed using ultrasound. Incomplete perforation of the uterus is best determined in phase II of the menstrual cycle, when the median uterine echo is clearly visible. The IUD going beyond the M-echo indicates incomplete perforation of the uterus. Complete perforation is indicated by the contraceptive being located outside the uterus.
Having confirmed the penetration of the IUD into the abdominal cavity, it is necessary to proceed to its surgical removal. "During the operation, the uterus is carefully examined and, depending on the changes detected, the question of its removal or preservation is decided. Early diagnosis of uterine perforation and timely surgical intervention ensure the safety of the uterus. Long-term presence of the IUD in the abdominal cavity leads to bedsores, the development of an inflammatory and adhesive process, intestinal obstruction. Necrotic and inflammatory changes in the uterine wall are a direct indication for its removal.
What do need to examine?
Who to contact?


 [
[