
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Neuroleptics, or antipsychotics
Medical expert of the article
Last reviewed: 04.07.2025
Antipsychotics (neuroleptics) are a class of psychotropic drugs primarily used to treat schizophrenia. Currently, it is common to distinguish two groups (or categories) of drugs: typical and atypical antipsychotics. Below is information on the pharmacological properties, indications for use, and side effects of therapy for each of these groups of drugs.
Indications for the use of typical antipsychotics
Currently, the main indications for prescribing traditional neuroleptics, according to recommendations provided by authoritative researchers in the field of psychopharmacotherapy, include the following.
- Relief of psychomotor agitation and behavioral disorders caused by severe psychotic symptoms. In these cases, the use of oral or parenteral forms of drugs with antipsychotic action is indicated, both global (clopromazine, levomepromazine, thioproperazine, zuclopenthixol) and selective - in the form of an effect on hallucinatory-paranoid disorders (haloperidol, trifluoperazine).
- Anti-relapse (preventive) therapy. For this purpose, depot forms of drugs are prescribed, especially in patients with poor drug compliance (haloperidol decanoate, prolonged form of flupentixol), or small or medium doses of drugs to obtain a disinhibitory (antinegative) effect, from among those drugs, high doses of which are used to relieve acute psychotic disorders (flupentixol, zuclopenthixol). In this type of therapy, it is also recommended to prescribe so-called small neuroleptics (thioridazine, chlorprothixene, sulpiride), the psychotropic activity of which consists of an effect on the manifestations of the depressive pole and insomnic disorders.
- Overcoming therapeutic resistance to atypical antipsychotics in the treatment of acute psychotic states. For this purpose, parenteral forms of traditional antipsychotics with global (chlorpromazine, levomepromazine, etc.) and selective (haloperidol) antipsychotic action are usually used.
These drugs cause various side effects, the nature of which depends on the features of the pharmacological profile of each drug. Antipsychotics with a more pronounced cholinolytic effect more often cause accommodation disorders, constipation, dry mouth, and urinary retention. A sedative effect is more typical of antipsychotics with a pronounced antihistamine effect, and orthostatic hypotension is more typical of drugs that block a1-adrenergic receptors. Blockade of cholinergic, nordrenergic and dopaminergic transmission by typical neuroleptics can lead to a number of disorders in the sexual sphere, such as amenorrhea or dysmenorrhea, anorgasmia, galactorrhea, swelling and soreness of the mammary glands, and decreased potency. Side effects in the sexual sphere are mainly associated with the cholinolytic and adrenoblocking properties of these drugs, and also with an increase in prolactin secretion due to the blockade of dopamine metabolism. The most serious side effects of typical neuroleptics are motor dysfunction. They are the most common reason for patients to stop taking medications. The three main side effects of therapy associated with the influence on the motor sphere include early extrapyramidal syndromes, tardive dyskinesia, and NMS.
Extrapyramidal syndromes are believed to be associated with blockade of D2 receptors in the basal ganglia. They include dystonia, neuroleptic parkinsonism, and akathisia. Manifestations of acute dystonic reaction (early dyskinesia) include suddenly developing hyperkinesis, oculogyric crises, contractions of the muscles of the face and trunk, opisthotonus. These disorders are dose-dependent and often occur after 2-5 days of therapy with highly potent neuroleptics such as haloperidol and fluphenazine. To relieve early dyskinesia, the neuroleptic dose is reduced and anticholinergic drugs (biperiden, trihexyphenidyl) are prescribed. Tardive dyskinesia usually involves the neck muscles and, unlike acute dystonic reaction, is less responsive to treatment with anticholinergics. Neuroleptic parkinsonism is characterized by decreased spontaneous motor skills, hypo- and amimia, resting tremor, and rigidity. It is important to distinguish these symptoms from the outwardly similar negative disorders in schizophrenia, which are represented by emotional alienation, dulling of affect, and anergia. To correct these side effects, the use of anticholinergics, a reduction in the dose of the neuroleptic, or its replacement with an atypical antipsychotic are indicated. Akathisia is manifested by internal anxiety, the inability to remain in one place for a long time, and the need to constantly move the arms or legs. To relieve it, anticholinergics and central beta-blockers (propranolol) are used.
Late dyskinesia is manifested by involuntary movements of any muscle group, most often the muscles of the tongue and mouth. Clinically, a number of its forms are distinguished: dyskinesia of the muscles of the cheeks, tongue, mouth (periodic contractions of the masticatory muscles, creating the impression of a grimacing person, the tongue may involuntarily protrude from the patient's mouth); tardive dystonia and tardive akathisia; (the patient makes choreoathetoid movements of the head, trunk, upper and lower limbs). This form of disorder is recorded mainly during long-term treatment with traditional neuroleptics and is detected in approximately 15-20% of patients taking them as maintenance therapy. Probably, in some patients the risk of developing dyskinesia symptoms is increased, since some of them were observed in the clinic of schizophrenia even before the "neuroleptic era". In addition, tardive dyskinesia has been described in elderly women and patients with affective disorders. Tardive dyskinesia is thought to be associated with an increase in the number of dopamine receptors in the striatum, although GABAergic and other neurotransmitter systems are also likely to be involved in its pathogenesis. There is no effective universal treatment for such side effects. It is suggested that low doses of high-potency neuroleptics with dopamine-blocking action or vitamin E may have a moderate beneficial effect in these disorders. The most effective measure for tardive dyskinesia is a reduction in the dose of a typical neuroleptic or its replacement with an atypical antipsychotic.
According to current data, neuroleptic malignant syndrome occurs in approximately 0.5% of cases of psychopharmacotherapy. Probably, the rare occurrence of such a life-threatening complication can currently be explained by the widespread introduction of atypical antipsychotics into practice, since the risk of developing NMS during treatment with these drugs is insignificant. It is generally accepted that the main cause of NMS development is excessive blockade of the dopaminergic system during therapy with neuroleptics, especially after increasing the dose of a highly potent antipsychotic. The main symptoms of NMS are hyperthermia, increased tone of skeletal muscles and tendon reflexes, impaired consciousness with transition to a coma. Blood tests reveal leukocytosis, increased erythrocyte sedimentation rate, liver transaminase activity; urine tests reveal the presence of albuminuria. Water and electrolyte balance disorders occur quickly, which creates the prerequisites for the formation of cerebral edema. NMS is an acute condition requiring urgent hospitalization of the patient for intensive infusion therapy. In the treatment of NMS, hydration and symptomatic therapy are most important. In this situation, any prescribed neuroleptics require immediate discontinuation. In some cases, dopamine receptor agonists (for example, bromocriptine) or muscle relaxants have a positive effect, although their effectiveness has not been studied. After eliminating NMS, the neuroleptic should not be resumed for at least two weeks. Subsequently, a low-potency antipsychotic may be prescribed, preferably a new-generation drug. The dose of the newly prescribed drug should be increased extremely carefully, monitoring the state of vital functions and laboratory data (blood and urine tests).
Typical neuroleptics rarely cause dangerous fatal complications. Overdose manifestations are mainly related to the individual profile of the antiadrenergic and anticholinergic action of the drug. Since these drugs have a strong antiemetic effect, gastric lavage is indicated for their elimination from the body, rather than the administration of emetics. Arterial hypotension, as a rule, is a consequence of adrenergic receptor blockade, and it should be corrected by the administration of dopamine and norepinephrine. In case of cardiac arrhythmia, the use of lidocaine is indicated.
Mechanism of action and pharmacological effects of typical antipsychotics
As psychopharmacology developed, various options for the effect of antipsychotics on neuroreceptors were proposed. The main hypothesis remains that they affect dopamine neurostructures (primarily D2 receptors), based on data on the disruption of normal dopamine metabolism in brain structures in psychoses. Dopamine D2 receptors are located in the basal ganglia, the nucleus accumbens, and the frontal cortex; they play a leading role in regulating the flow of information between the cerebral cortex and the thalamus.
The figure demonstrates a more detailed understanding of the disturbances in dopamine transmission in the cortical and subcortical areas of the brain and the role of these disturbances in the development of schizophrenia symptoms (adapted from the monograph by Jones R.B., Buckley P.F., 2006).
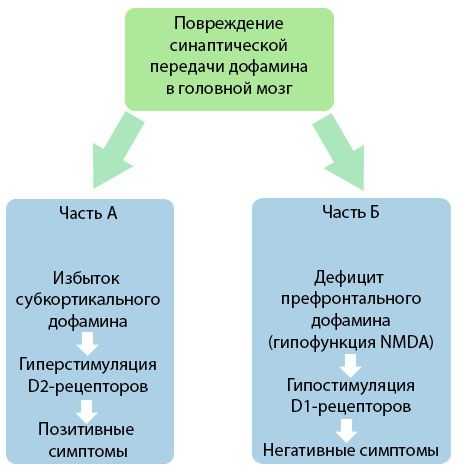
Part A reflects the classical, early dopamine theory, postulating an excess of dopamine in subcortical areas and hyperstimulation of D2 receptors, which leads to the emergence of productive symptoms. Part B demonstrates the subsequent modernization of the theory in the early 1990s. The data obtained by this time revealed that a deficiency of dopamine in D receptors, together with insufficient stimulation of these receptors in the prefrontal cortex, leads to the emergence of negative symptoms and cognitive deficits. Therefore, according to modern understanding, both types of dopaminergic transmission disorders - an excess of subcortical dopamine and its deficiency in the prefrontal cortex - are the combined result of a disruption of synaptic transmission in the prefrontal area and are associated with N-methyl-N-aspartate hypofunction. In addition to the initially isolated dopamine, other neurotransmitters involved in the pathogenesis of schizophrenia were later identified, such as serotonin, gamma-aminobutyric acid, glutamate, norepinephrine, acetylcholine and various neuropeptides. Although the role of these mediators has not been fully studied, nevertheless, as knowledge develops, it becomes clear that the manifestation of numerous neurochemical shifts in the body. Therefore, the clinical effect of an antipsychotic drug is a summation of the effects on various receptor formations and leads to the elimination of homeostasis disorders.
In recent years, due to the emergence of new research methods such as radioisotope ligand binding and PET scanning, significant progress has been made in elucidating the fine biochemical mechanism of action of neuroleptics. In particular, the comparative strength and tropism of drugs to bind to individual neuroreceptors in various areas and structures of the brain has been determined. A direct dependence of the severity of the antipsychotic effect of a drug on the strength of its blocking effect on various dopaminergic receptors has been shown. Recently, four types of such receptors have been identified:
- D1 are located predominantly in the area of the substantia nigra and the striatum (the so-called nigrostriatal region), as well as the prefrontal region;
- D2 - in the nigrostriatal, mesolimbic regions and the anterior pituitary gland (secretion of prolactin);
- D3 (presynaptic) - in various brain structures, control dopaminergic activity according to the law of negative feedback;
- D4 (presynaptic) - predominantly in the nigrostriatal and mesolimbic areas.
At the same time, it can now be considered proven that it is the blockade of D2 receptors that causes the development of antipsychotic, secondary sedative effects, as well as extrapyramidal side effects. Other clinical manifestations of the blockade of this type of receptors are the analgesic and antiemetic effect of neuroleptics (reduction of nausea, vomiting as a result of suppression of the vomiting center), as well as a decrease in the content of growth hormone and an increase in the production of prolactin (neuroendocrine side effects, including galactorrhea and menstrual irregularities). Long-term blockade of nigrostriatal D2 receptors leads to the appearance of their hypersensitivity, which is responsible for the development of tardive dyskinesias and "hypersensitivity psychoses". Probable clinical manifestations of the blockade of presynaptic D3 and D4 receptors are associated mainly with the stimulating effect of neuroleptics. Due to the partial blockade of these receptors in the nigrostriatal and mesolimbocortical areas, activating and incisive (powerful, highly active) neuroleptics in small doses can stimulate, and in high doses suppress, dopaminergic transmission.
In recent years, interest in the function of the serotonergic systems of the brain, including serotonin receptors, has increased sharply. The fact is that in various parts of the brain, the serotonergic system has a modulating effect on dopaminergic structures. In particular, in the mesocortical region, serotonin inhibits the release of dopamine, and accordingly, the blockade of postsynaptic 5-HT receptors leads to an increase in dopamine content. As is known, the development of negative symptoms in schizophrenia is associated with hypofunction of dopamine neurons in the prefrontal structures of the cerebral cortex. Currently, about 15 types of central 5-HT receptors are known. It has been experimentally discovered that neuroleptics bind mainly to 5-HT receptors of the first three types.
These drugs have a mainly stimulating (agonistic) effect on 5-HT1a receptors. Probable clinical consequences: increased antipsychotic activity, decreased severity of cognitive disorders, correction of negative symptoms, antidepressant effect and decreased incidence of extrapyramidal side effects.
The effect of neuroleptics on 5-HT2 receptors, especially on 5-HT2a subtypes, is of significant importance. They are located mainly in the cerebral cortex and their sensitivity is increased in patients with schizophrenia. The ability of new-generation neuroleptics to reduce the severity of negative symptoms, improve cognitive functions, regulate sleep by increasing the total duration of slow-wave (D-wave) sleep stages, reduce aggression and alleviate depressive symptoms and migraine-like (arising from cerebrovascular disorders) headaches is associated with the blockade of 5-HT2a receptors. On the other hand, with the blockade of 5-HT2a receptors, hypotensive effects and ejaculation disorders in men are possible.
It is believed that the effect of neuroleptics on 5-HT2c receptors causes a sedative (anxiolytic) effect, increased appetite (accompanied by an increase in body weight) and a decrease in prolactin production.
5-HT3 receptors are located predominantly in the limbic region, and when they are blocked, the antiemetic effect develops first, and the antipsychotic and anxiolytic effects are also enhanced.
The occurrence of Parkinsonism-like symptoms also depends on the blocking power of the drug on muscarinic cholinergic receptors. Cholinolytic and dopamine-blocking effects are to a certain extent in reciprocal relationships. It is known, for example, that in the nigrostriatal region D2 receptors inhibit the release of acetylcholine. When more than 75% of D2 receptors in the nigrostriatal region are blocked, the balance is disturbed in favor of the cholinergic system. This is the reason for the corrective effect of anticholinergic drugs (correctors) on neuroleptic extrapyramidal side effects. Chlorprothixene, clozapine and olanzapine have a high affinity for muscarinic receptors and practically do not cause extrapyramidal side effects, since they block cholinergic and dopaminergic receptors simultaneously. Haloperidol and piperazine phenothiazine derivatives have a pronounced effect on dopamine receptors, but have a very weak effect on choline receptors. This is due to their ability to cause pronounced extrapyramidal side effects, which are reduced when very high doses are used, when the cholinolytic effect becomes noticeable. In addition to reducing the dopamine-blocking effect on D2 receptors of the nigrostriatal region and leveling extrapyramidal side effects, a strong cholinergic effect can cause deterioration of cognitive functions, including memory disorders, as well as peripheral side effects (dry mucous membranes, impaired visual accommodation, constipation, urinary retention, confusion, etc.). Neuroleptics have a fairly strong blocking effect on type I histamine receptors, which is associated, first of all, with the severity of the sedative effect, as well as an increase in body weight due to increased appetite. The antiallergic and antipruritic effects of neuroleptics are also associated with their antihistamine properties.
In addition to dopamine blocking, antiserotonergic, cholinolytic and antihistamine effects, most neuroleptics have adrenolytic properties, i.e. they block both central and peripheral a1-adrenoreceptors. Adrenoblockers such as chlorpromazine and chlorprothixene have a pronounced sedative effect. In addition, the blocking effect of these drugs can cause neurovegetative side effects (arterial hypotension, tachycardia, etc.), as well as an increase in the hypotensive effect of adrenoblockers.
The works of a large number of authors provide data on the binding strength (affinity) of individual neuroleptics with different types of neuroreceptors.
Based on their neurochemical profile of action, typical and atypical antipsychotics, among those predominantly used in clinical practice, can be conditionally divided into six groups.
The first group consists of selective blockers of D2 and D4 receptors (sulpiride, amisudpride, haloperidol, etc.) from the groups of benzamide and butyrophenone derivatives. In small doses, mainly due to the blockade of presynaptic D4 receptors, they activate dopaminergic transmission of nerve impulses and have a stimulating (disinhibitory) effect, in large doses they block D2 receptors in all areas of the brain, which is clinically manifested by a pronounced antipsychotic effect, as well as extrapyramidal and endocrine (due to prolactinemia) side effects.
The second group includes highly active D2-receptor blockers, as well as drugs that weakly or moderately block 5-HT2a- and 5-HT1a-receptors (flupentixol, fluphenazine, zuclopenthixol, etc.), i.e. mainly piperazine derivatives of phenothiazine or thioxanthenes close to them in stereochemical structure. Like the drugs of the first group, these neuroleptics have, first of all, a pronounced antipsychotic (incisive) effect, and also cause extrapyramidal pye effects and prolactinemia. In small doses, they have a moderately activating (psychostimulating) effect.
The third group consists of polyvalent sedative neuroleptics that block most neuroreceptors in an undifferentiated manner. These drugs have a clearly expressed blocking effect on dopamine receptors and also cause strong adrenolytic and cholinolytic effects. This includes most sedative neuroleptics, primarily aliphatic and piperidine derivatives of phenothiazine, as well as thioxanthenes that are close to them in stereochemical structure (chlorpromazine, levomepromazine, chlorprothixene, etc.). The spectrum of psychotropic activity of these drugs is dominated, first of all, by a pronounced primary sedative effect, developing regardless of the dose used, and a moderate antipsychotic effect. In addition, due to their pronounced anticholinergic effect, drugs of this group cause weak or moderate extrapyramidal and neuroendocrine side effects, but often lead to the development of orthostatic hypotension and other autonomic reactions due to pronounced blockade of a1-adrenergic receptors.
The fourth group includes neuroleptics that block D2- and 5-HT2a-receptors in a balanced manner, i.e. to the same extent (the latter to a slightly greater extent) and a1-adrenoreceptors to a moderate extent. This group includes representatives of the new generation of atypical antipsychotics (risperidone, ziprasidone, sertindole), which have different chemical structures. The neurochemical mechanism of action determines their selective influence primarily on the mesolimbic and mesocortical areas of the brain. Along with a distinct antipsychotic effect, the absence or weak expression of extrapyramidal side effects (when using therapeutic doses), weak or moderate prolactinemia and moderate adrenolytic properties (hypotensive reactions), this group of neuroleptics is able to correct negative symptoms by indirect stimulation of dopaminergic transmission in the cerebral cortex.
The fifth group consists of polyvalent atypical antipsychotics of tricyclic dibenzodiazepine or similar structure (clozapine, olanzapine and quetiapine). Just like the drugs of the third group, they block most neuroreceptors in an undifferentiated manner. However, 5-HT2a receptors are blocked more strongly than D2 and D4 receptors, especially those located in the nigrostriatal region. This determines the actual absence or weak extrapyramidal effect and the absence of neuroendocrine side effects associated with increased prolactin production with a distinct antipsychotic effect and the ability to reduce the severity of negative symptoms. In addition, all drugs of this group have pronounced adrenolytic and antihistamine properties, which determines the sedative and hypotensive effects. Clozapine and olanzapine also have a fairly pronounced blocking effect on muscarinic receptors and lead to the development of cholinolytic side effects.
Thus, the ability to block postsynaptic dopaminergic receptors with a compensatory increase in the synthesis and metabolism of dopamine is the only common biochemical property for all neuroleptics considered in these groups.
The sixth group includes the only atypical antipsychotic, aripiprazole, which has appeared on the domestic psychopharmacological market relatively recently. This drug is a partial agonist of D2-dopamine receptors, and acts as a functional antagonist in a hyperdopaminergic state and as a functional agonist in a hypodopaminergic profile. Such a unique receptor profile of aripiprazole makes it possible to reduce the risk of extrapyramidal disorders and hyperprolactinemia when using it. In addition, aripiprazole acts as a partial agonist of 5-HT1a receptors and at the same time it is an antagonist of 5-HT2a receptors. It is assumed that such interaction with receptors leads to a generally balanced functioning of the serotonin and dopamine systems, so the mechanism of action of aripiprazole can be designated as stabilizing the dopamine-serotonin system.
Thus, the current level of knowledge about the neurochemical mechanisms of action of neuroleptics allows us to propose a new, pathogenetically more substantiated pharmacodynamic classification of this group of psychotropic drugs. The use of this classification allows us to predict to a large extent the spectrum of psychotropic activity, tolerance and probable drug interactions of a particular drug. In other words, the features of the neurochemical activity of a drug largely determine the features of its clinical activity, which should be used when choosing a particular antipsychotic drug for a specific patient.
The effectiveness of the global antipsychotic effect of any neuroleptic is estimated using the so-called chlorpromazine equivalent, which is taken as 1. For example, the chlorpromazine equivalent of haloperidol = 50. This means that the antipsychotic effectiveness of 1 mg of haloperidol is comparable to 50 mg of chlorpromazine. Based on this indicator, a classification has been developed that provides for the allocation of neuroleptics with high (chlorpromazine equivalent> 10.0), medium (chlorpromazine equivalent = 1.0-10.0) and low (chlorpromazine equivalent = 1.0) antipsychotic activity, called patentity. Typical neuroleptics (first-generation antipsychotics) have been widely used in clinical psychopharmacotherapy for almost half a century. The spectrum of their therapeutic activity includes:
- global antipsychotic action in the form of the ability to evenly and differentially reduce various manifestations of psychosis:
- primary sedative (inhibitory) effect - the ability of drugs to quickly relieve psychomotor agitation;
- selective, selective antipsychotic action, manifested in the ability to influence individual symptoms: delirium, hallucinations, disinhibition of drives, etc.;
- activating (disinhibitory, disinhibitory, antiautistic) neurotropic action, manifested by the development of extrapyramidal symptoms;
- somatotropic action in the form of development of neuroendocrine and vegetative side effects;
- depressant effect, expressed in the ability of some antipsychotics to cause depressive symptoms.
The effectiveness of first-generation antipsychotics in the treatment of not only psychotic disorders, but also disorders within borderline psychiatry has been proven many times and is indisputable. Therefore, despite the high frequency of side effects of therapy when they are prescribed, they continue to be used in medical practice.
Atypical antipsychotics
Modern guidelines contain data on the advantages of using second-generation antipsychotics in pharmacotherapy. The term "atypical" (synonym - second-generation antipsychotics) is conditional and is used mainly for the convenience of designating the new generation. Compared with traditional neuroleptics, drugs of this group are more effective in correcting negative, affective and cognitive disorders, which is combined with better tolerability and a lower risk of extrapyramidal symptoms. Differences in the nature of the therapeutic effect of one or another drug from a series of atypical antipsychotics are explained, as in the group of typical neuroleptics, by its individual profile of pharmacological action.
To clarify the possibilities of psychopharmacotherapy with atypical antipsychotics, it is advisable to focus on the drugs of this group registered in Russia.
 [ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ]
[ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ]
Clozapine (dibenzodiazepine)
The founder of the group of atypical antipsychotics. The mechanism of action of clozapine is characterized by a slight blockade of D2 receptors with simultaneous high antagonism to 5-HT2a receptors, a1, a2-adrenergic and H1-histamine receptors. It has proven itself as an effective antipsychotic in cases of resistance to other antipsychotics (a drug of the reserve group), and is also indicated for the treatment of chronic mania, psychotic agitation, aggression. In domestic practice, clozapine is often prescribed to achieve sedation and as a hypnotic in psychotic patients. It should be recognized that such use of clozapine does not correspond to its main profile of indications for use in therapy. Probably, the attitude to this antipsychotic as a drug of secondary importance should be revised, since today it is the only drug with proven effectiveness in resistant patients.
Clozapine, unlike typical neuroleptics, does not cause serious extrapyramidal disorders due to the aforementioned low affinity for O2 receptors. It also turned out that it can be used to treat late dystonia and severe akathisia. Due to the low risk of developing NMS, clozapine can be considered a drug of choice in patients who have previously suffered from this complication.
However, a number of serious side effects may develop during clozapine therapy. The most dangerous of them (even when small doses are prescribed) is agranulocytosis, which occurs in 0.5-1.0% of patients. Other important side effects that may occur when using the drug include drowsiness, hypersalivation, and weight gain, which is often already elevated by the time clozapine is prescribed under the influence of previous antipsychotic therapy. Attention should also be paid to the possibility of developing tachycardia, arterial hypotension, and epileptic seizures when taking it. The likelihood of seizures depends on the dose. Their risk increases significantly if the clozapine dose exceeds 600 mg/day. The development of seizures is not a contraindication for further use of the drug, but requires a halving of the dose and the prescription of anticonvulsants, such as valproic acid. Prevention of side effects of clozapine treatment includes careful monitoring of white blood cell counts, as well as ECG and endocrine parameters.
Clozapine overdose may cause depression of consciousness up to the development of coma, as well as symptoms associated with the cholinolytic effect (tachycardia, delirium), epileptic seizures, respiratory depression, extrapyramidal syndromes. A fatal outcome may occur when taking a dose exceeding 2500 mg of the drug.
 [ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ], [ 39 ], [ 40 ], [ 41 ]
[ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ], [ 39 ], [ 40 ], [ 41 ]
Risperidone
A benzisoxazole derivative with high affinity for serotonin and dopamine Dj receptors with a predominant effect on the serotonin system. The drug has a wide range of indications for use, including relief of exacerbations, anti-relapse treatment, therapy for the first psychotic episode, and correction of negative symptoms of schizophrenia. The drug has been shown to improve cognitive functioning in patients with schizophrenia. Preliminary data have been obtained that risperidone also reduces comorbid affective symptoms in patients with schizophrenia and may be a drug of choice in the treatment of bipolar affective disorders.
Side effects of risperidone therapy, especially extrapyramidal disorders, are dose-dependent and occur more often at doses exceeding 6 mg/day. Other side effects include nausea, vomiting, anxiety, drowsiness, and increased serum prolactin levels. Long-term use of risperidone may lead to weight gain and the development of type 2 diabetes mellitus, but with a lower probability compared to clozapine, olanzapine.
Overdose may cause somnolence, epileptic seizures, prolongation of the QT interval and widening of the QRS complex, and arterial hypotension. Cases of fatal outcome due to risperidone overdose have been described.
The undoubted advantage of the drug is the availability of liquid and fast-dissolving (sublingual) forms, the use of which accelerates the entry of the drug into the patient's body and facilitates control over its intake. There is also a prolonged form of the drug - powder for the preparation of a suspension for intramuscular administration (consta-risperidone in microspheres). It is recommended for maintenance treatment of patients with schizophrenia, especially for patients with poor compliance. It is necessary to take into account the fact that the drug needs about three weeks to enter the bloodstream, therefore, when starting therapy with consta-risperidone, the patient must additionally take the oral form of risperidone for at least 3 weeks after the first injection.
Olanzapine
In terms of pharmacological action, it is close to clozapine, since it has a pleiomorphic receptor profile with significant affinity for serotonin, muscarinic, a1-adrenergic, and histamine receptors. The therapeutic activity of olanzapine has features similar to the effectiveness of clozapine and risperidone in terms of the impact on positive, negative, and depressive symptoms of schizophrenia. At the same time, data have been obtained on the greater effectiveness of olanzapine compared to other atypical antipsychotics in patients with the first psychotic episode and in the correction of cognitive functioning indicators. It should be taken into account that at the beginning of therapy using the tablet form of the drug, a rapid disinhibitory effect may appear with increased psychomotor agitation and anxiety. Therefore, in the treatment of attacks accompanied by severe psychomotor agitation, the use of the injection form of the drug is indicated.
Olanzapine rarely causes extrapyramidal disorders or tardive dyskinesia, and the most common side effects with its use are metabolic disorders and weight gain. It has been established that patients receiving olanzapine quite often experience elevated levels of cholesterol, plasma lipids, and a predisposition to type 2 diabetes mellitus, but such effects were equally common in patients receiving both olanzapine and clozapine. At the same time, data have been obtained showing that weight gain correlates with a positive response to olanzapine (i.e. serves as an important prognostic indicator of therapy), and develops into obesity only in 20-30% of patients who have gained excess weight during treatment.
Overdose may cause sedation, toxic anticholinergic effects, epileptic seizures, and arterial hypotension. There is currently no convincing data to assess the risk of death from overdose.
Quetiapine
It is classified as a dibenzothiazepine compound. Its receptor profile is largely similar to that of clozapine. The binding level of quetiapine to D2 receptors is low (less than 50%) and short-term even when high doses are used. The drug is effective in the treatment of positive, negative and general symptoms of schizophrenia. There is evidence of its successful use both in cases of high resistance to therapy and for improving the cognitive functioning of patients, which gives the right to recommend it as a first-line antipsychotic for maintenance therapy of schizophrenia. Finally, quetiapine has a moderate antidepressant, activating effect. Therefore, it is indicated in the treatment of depressive-delusional attacks and disorders of the senesto-hypochondriacal circle.
The established high thymotropic activity of quetiapine explains the fact that it is registered as a means for the relief and secondary prevention of depressive disorders. For the treatment of manic episodes within bipolar disorders of type I and II, quetiapine is used as an additional means. The absence of injection forms somewhat limits its use in patients with agitation and aggressive behavior.
Quetiapine is well tolerated, it practically does not cause extrapyramidal syndromes, except in cases where maximum doses are used. Quetiapine does not cause hyperprolactinemia, less often than olanzapine and clozapine, it leads to weight gain and impaired glucose tolerance.
Ziprasidone
Has a unique profile of receptor activity. Being a potent antagonist of 5HT2a receptors and D2 receptors, it is also an active inhibitor of serotonin and norepinephrine reuptake. Clinical studies have demonstrated significant superiority of ziprasidone in its effect on psychotic symptoms and manifestations of aggression compared to haloperidol. There is also data on the positive effect of ziprasidone on the cognitive functions of patients with schizophrenia, as well as on comorbid affective symptoms, indicators of social functioning. Ziprasidone is usually well tolerated and very rarely causes extrapyramidal syndromes, weight gain and metabolic disorders. More often there is an extension of the QT interval over 460 ms, therefore, it is advisable for patients receiving this drug to undergo an ECG examination both before prescribing the drug and control monitoring during treatment. Particular attention should be paid to concomitant therapy (taking antiarrhythmic drugs), which can aggravate the prolongation of the QT interval and lead to the development of cardiac arrhythmia, ventricular fibrillation.
Sertindole
Belongs to derivatives of phenylindole. It has high functional antagonism in relation to D2-, serotonin (especially 5-HT2a-receptors) and a1-adrenergic receptors. According to electroneurochemical studies, sertindole selectively inhibits dopamine receptors in the ventral segmental region. Such selectivity, in all likelihood, ensures a low risk of extrapyramidal syndromes and hyperprolactinemia when using the drug. The results of comparative studies have shown that sertindole is comparable to haloperidol in terms of antipsychotic activity. The drug has a pronounced disinhibitory effect in patients with negative and depressive symptoms, which is superior to a similar effect of rispolept. There is also evidence confirming the effectiveness of sertindole for the correction of cognitive impairment in patients with schizophrenia. Sertindole is generally well tolerated by patients, rarely causes sedation and is therefore recommended as a replacement drug when side effects occur during therapy with other modern antipsychotics.
Serious side effects include the ability of the drug to prolong the Q-T interval, which can lead to cardiac arrhythmia. When analyzing post-marketing studies, it became clear that the cardiac profile of sertindole does not differ from that of other new-generation antipsychotics.
Aripiprazole
It has antipsychotic activity comparable to other atypical agents, but has a greater effect on the parameters of cognitive functioning of patients with schizophrenia. The above-mentioned unique pharmacological action of the drug - a partial agonist of D2 receptors - allows to reduce the risk of extrapyramidal syndromes and hyperprolactinemia when using it.
 [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ]
[ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ]
Amisulpride
Belongs to the class of substituted benzamides. The drug selectively binds to the subtypes of D2 and D3 dopaminergic receptors, has no affinity for the subtypes of D1, D4 and D5, as well as for serotonin, H1-histamine, a1-adrenergic and cholinergic receptors. When used in high doses, it blocks postsynaptic D2 receptors. In low doses, its disinhibitory effect is manifested due to the blockade of presynaptic D2, D3 receptors, due to which its use is also effective in the treatment of negative symptoms, although it is not a combined antagonist of D2 receptors and serotonin receptors. The results of a number of studies indicate a pronounced antipsychotic activity of the drug when used in high doses, which is superior to traditional drugs.
 [ 48 ], [ 49 ], [ 50 ], [ 51 ], [ 52 ], [ 53 ], [ 54 ], [ 55 ]
[ 48 ], [ 49 ], [ 50 ], [ 51 ], [ 52 ], [ 53 ], [ 54 ], [ 55 ]
Side effects of antipsychotic therapy
The table lists the main side effects of atypical antipsychotic therapy.
Preparation |
Extrapyramidal |
Conduction disturbance on ECG |
Metabolic disorders (weight gain, increased levels of glucose, cholesterol, triglycerides in the blood) |
||
Clozapine |
. |
++ |
++ |
++- |
|
Risperidone |
++ |
+/- |
++ |
+/- |
|
Olanzapine |
+ |
+/- |
+++ |
++ |
+++ |
Quetiapine |
+/- |
+ |
+/- |
--- |
|
Ziprasidone |
+ |
++ |
+/- |
+/- |
+/- |
Sertindole |
++ |
-- |
+/- |
-- |
|
Ariliprazole |
-- |
--- |
+/- |
-- |
-- |
Amisulpride |
++ |
+/- |
|||
Note. Severity of side effects: "+++" - high; "++" - average; "+" - low; "+/-" - questionable; "-" - absent.
Extrapyramidal syndromes
One of the main features of atypical antipsychotics, in contrast to traditional ones, is their low ability to cause extrapyramidal syndromes, which became a breakthrough in the maintenance pharmacotherapy of schizophrenia. However, as follows from the data in the table, when using individual drugs of this series (risperidone, amisulpride), such symptoms may occur, which requires special attention when prescribing them.
 [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
[ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
ECG abnormalities
The possibility of developing cardiac side effects is a serious problem when using some modern antipsychotics in therapy. In these cases, we are talking about prolongation of the Q-T interval, which can lead to the development of arrhythmia. Conduction disturbances, primarily prolongation of the Q-T interval, are most often observed during treatment with clozapine, sertindole, ziprasidone. Concomitant pathology in the form of bradycardia, atrioventricular block, hypothyroidism can contribute to the occurrence of this complication during therapy with the above-mentioned drugs. Currently, ECG monitoring is recommended approximately once every 3 months in patients receiving maintenance therapy with atypical antipsychotics.
 [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ]
[ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ]
Endocrine disorders
Currently, the greatest concern is caused by the ability of atypical antipsychotic drugs to cause weight gain. Increased body weight, glucose and triglyceride levels in the blood can lead to metabolic disorders and the development of type 2 diabetes. Particular caution and weekly monitoring of biochemical parameters are necessary during therapy with clozapine and olanzapine. According to J. Geddes et al. (2000), P.B. Jones, P.F. Buckley (2006), it should be recognized as appropriate to conduct a thorough examination of patients before prescribing them a particular antipsychotic of the modern generation, since it is known that metabolic disorders more often occur in patients who had a hereditary predisposition, excess body weight, lipid spectrum disorders and hyperglycemia before the start of treatment. The monitoring algorithm proposed by P.B. Jones, P.F. Buckley (2006) includes several points.
- Collection of medical history and family factors regarding the risk of metabolic disorders.
- Registration of body mass index, ECG, blood pressure and pulse before the start of treatment.
- Collection of laboratory data (glucose, lipid profile, cholesterol) before starting therapy.
- Regular monitoring of body mass index and vital signs during treatment.
- Monitoring laboratory data during treatment.
The occurrence of hyperprolactinemia during antipsychotic therapy is due to central blockade of dopamine receptors in the hypothalamus, which leads to the release of prolactin from the anterior pituitary gland. Hyperprolactinemia most often occurs with treatment with olanzapine, risperidone, and amisulpride.
 [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ]
[ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ]
Agranulocytosis
Another serious complication of antipsychotic therapy. It can be observed during treatment with clozapine and olanzapine. According to J. Geddes et al. (2000), it was diagnosed during the first 3 months in 1-2% of patients taking these drugs. In this regard, weekly blood tests are recommended for patients taking these drugs during the first 18 weeks of therapy and monthly monitoring thereafter. It has been shown that when the dose of the above-mentioned neuroleptics is reduced, the clinical blood test returns to normal. At the same time, it should be recognized that to date there is no clear strategy for patients who experience the above-mentioned side effects associated with metabolic disorders. Most often, one atypical antipsychotic is replaced by another. Another promising direction is the appointment of special corrective therapy, in particular the use of bromocriptine to correct hyperprolactinemia. The ideal situation is one in which the care of a patient with such disorders is carried out with the periodic involvement of internists, in particular endocrinologists, cardiologists and other specialists.
In conclusion, it should be noted that if the given algorithms for prescribing and monitoring not only the mental but also the physical state of patients are followed, the use of second-generation drugs is safer than typical neuroleptics.
A number of other antipsychotics are currently in the development stage. Next-generation drugs will likely have a different mechanism of action (for example, a GABAergic profile) and will be able to influence various manifestations of schizophrenia, including deficit disorders proper.
Attention!
To simplify the perception of information, this instruction for use of the drug "Neuroleptics, or antipsychotics" translated and presented in a special form on the basis of the official instructions for medical use of the drug. Before use read the annotation that came directly to medicines.
Description provided for informational purposes and is not a guide to self-healing. The need for this drug, the purpose of the treatment regimen, methods and dose of the drug is determined solely by the attending physician. Self-medication is dangerous for your health.

