
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
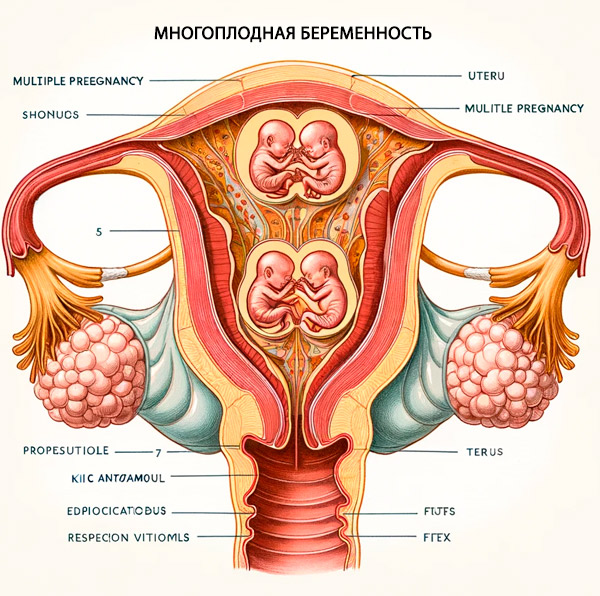
Multiple pregnancies
Medical expert of the article
Last reviewed: 12.07.2025
Multiple pregnancy is a pregnancy in which two or more fetuses develop in a woman's body. Births with two or more fetuses are called multiple births.
Epidemiology
Twin pregnancies account for 2 to 4% of all births. [ 1 ], [ 2 ], [ 3 ] The incidence of spontaneous twin pregnancies varies worldwide. Prevalence rates range from fewer than 8 twin pregnancies per 1,000 births in East, Southeast, and South Asia, India, and Oceania, to 9–16 per 1,000 births in the United States and Latin America, to 17 or more per 1,000 births in Africa. [ 4 ] The highest rate of twin pregnancies is in Nigeria and the lowest in Japan. [ 5 ] This difference is mainly due to dizygotic twin pregnancies, as the incidence of monozygotic pregnancies is virtually constant, ranging from 3.5 to 4 per 1,000 births.
Causes multiple pregnancy
The causes of multiple pregnancy are varied and have not been sufficiently studied. Heredity plays a certain role in the tendency to multiple pregnancy. Most likely, the tendency to develop multiple pregnancy can be inherited through the maternal line in a recessive manner.
An increase in the level of follicle-stimulating hormone (FSH), which promotes the maturation of several eggs, plays a major role in the occurrence of multiple pregnancies. This can be hereditarily determined, as well as a consequence of drug influence (use of ovulation stimulants, withdrawal of estrogen-gestagen drugs, in vitro fertilization). An increase in FSH also explains the fact that the frequency of multiple pregnancies increases with the age of the woman.
Among women with multiple pregnancies, multiparous women predominate.
Multiple pregnancies can occur as a result of the fertilization of two or more eggs that mature at the same time - fraternal or dizygotic twins; and also as a result of the development of two or more embryos from one fertilized egg - identical or monozygotic twins. [ 6 ]
Risk factors
Risk factors for dizygotic multiple pregnancy include: geography (more common in countries with milder climates), ethnicity (black ethnicity), multiple pregnancy, advanced maternal age (ovarian hyperstimulation due to elevated gonadotropin levels at ages 35 and 39), low socioeconomic status, use of oral contraceptives, 8 family history (7–15% of the population have a dominant gene that causes twin pregnancy), and use of assisted reproductive technologies.[ 7 ]
Symptoms multiple pregnancy
The course of multiple pregnancy, compared to singleton pregnancy, has a number of unfavorable features. In addition, the course of pregnancy in the monochorionic type is more unfavorable compared to the dichorionic type.
The volume of circulating blood in multiple pregnancies increases by 50-60%, while in single pregnancies it increases by 40-50%. This causes earlier and more frequent development of hemodynamic disorders.
The most common complications of multiple pregnancies are:
- premature birth (in 25-50% of cases). The average pregnancy duration for twins is 37 weeks, and for triplets - 35 weeks;
- spontaneous abortion;
- gestosis in pregnant women occurs much more frequently and is more severe than in singleton pregnancies;
- bleeding during pregnancy;
- anemia of pregnancy;
- polyhydramnios;
- intrauterine growth retardation of fetuses.
In multiple pregnancies, fetal malformations are observed twice as often as in singleton pregnancies, especially in monozygotic twins.
In multiple pregnancies, varicose veins develop more often. The enlarged uterus displaces the diaphragm, which complicates the heart's activity, resulting in shortness of breath and tachycardia. And compression of the internal organs by the enlarged uterus can be accompanied by intestinal dysfunction, heartburn, and frequent urination.
Multiple Pregnancy - Course and Complications
The course of labor in multiple pregnancies
The prevalence of preterm birth ranges from 5 to 18% in different countries. Brazil, India, China, Nigeria, and the United States are among the 10 countries with the highest estimated rates of preterm birth.[ 8 ],[ 9 ] Preterm birth occurred in 51% of twin pregnancies, and early preterm birth (birth before 32 weeks) occurred in 14% of twin pregnancies.[ 10 ],[ 11 ]
The course of labor with twins is often accompanied by significant complications. Premature labor with multiple pregnancy is observed in almost every second woman. During labor, untimely discharge of amniotic fluid (premature or early) is often observed, and prolapse of the umbilical cord loops of the fetus, its small parts is possible.
Due to overstretching of the uterus, labor can be protracted, since the period of opening of the cervix is extended due to the weakness of labor activity.
The period of expulsion is often protracted. Sometimes the presenting part of the second fetus tries to insert itself into the pelvis at the same time, and prolonged labor is necessary for one head to insert itself into the pelvic entrance.
A fairly common complication of the expulsion period is delayed rupture of the amniotic sac, which also leads to a prolongation of this period of labor.
Untimely rupture of amniotic fluid and prolongation of labor increase the risk of postpartum purulent-septic complications in the mother and fetal distress.
One of the serious complications of the expulsion period is premature placental abruption, caused by a rapid decrease in the volume of the uterus and a decrease in intrauterine pressure after the birth of the first fetus.
A very rare but extremely serious complication of the expulsion period in multiple pregnancies is a collision (linkage) of twins. There are different options for linking the fetuses. Most often, the head of one fetus links with the presenting head of the other. This occurs when the first twin is born in a breech presentation and the second in a cephalic presentation, or the first in a breech presentation and the second in a transverse position.
After the birth of the first twin, the second may take a transverse position even if before the birth it was in a longitudinal position, which also causes various complications.
In the afterbirth and early postpartum periods, hypotonic bleeding often occurs due to overstretching of the uterus.
In the postpartum period, subinvolution of the uterus is also possible.
The management of labor in multiple pregnancies has its own characteristics. The main factors that determine the management of labor in multiple pregnancies are:
- pregnancy period;
- condition of the fruit;
- fetal position and presentation;
- nature of labor;
- integrity of the amniotic sac.
According to indications, surgical delivery is used: cesarean section, vaginal delivery operations (vacuum extraction by the fetal head, obstetric forceps operation). Indications for planned and emergency cesarean section in case of multiple pregnancy are generally the same as in case of singleton pregnancy. It should also be known that multiple pregnancy with breech presentation of the first fetus is an indication for cesarean section.
In case of occipital presentation of the first fetus, intact fetal bladder, regular labor activity and good condition of the fetuses, labor is carried out actively and expectantly under cardiomonitoring control of the condition of the fetuses with the help of the nature of contractile activity of the uterus, the dynamics of the opening of the cervix, insertion and descent of the presenting part of the first fetus, the condition of the woman in labor. Prevention of weakness of labor activity and hypotonic bleeding is carried out.
After the birth of the first fetus, not only the fetal but also the maternal end of the umbilical cord is tied. If this is not done and the twins are identical, the second fetus may quickly die from bleeding through the umbilical cord of the first.
The physician's tactics after the birth of the first fetus should be active-expectant. After the birth of the first fetus, the fetal heartbeat is monitored, an external obstetric examination is performed to clarify the obstetric situation. If after the birth of the first fetus the general condition of the woman in labor is satisfactory, and the fetus is in a longitudinal position and without signs of distress, then there is no need for immediate opening of the amniotic sac of the second twin and its extraction. If after the birth of the first fetus the second fetus is not born within 10-1.5 minutes, the amniotic sac of the second fetus is opened, amniotic fluid is slowly released and, if the longitudinal position, labor continues conservatively. If the second fetus is in a transverse position, a combined turn onto the foot of the fetus is performed under anesthesia with its subsequent extraction. If the fetus is large, is in a breech presentation or transverse position, a cesarean section is performed.
It is possible to perform obstetric operations to extract a second fetus if labor is complicated by weak labor or fetal distress. In this case, depending on the obstetric situation, a cesarean section, vacuum extraction of the fetus by the head, or extraction of the fetus by the pelvic end is performed.
In case of pregnancy with three or more fetuses, preference is given to delivery by caesarean section. Cesarean section is also performed in case of twin fusion.
In case of multiple pregnancy, special attention should be paid to the third (subsequent) period due to the high risk of bleeding. It is necessary to carefully monitor the woman's condition and the amount of blood lost, and carry out bleeding prevention, including uterotonics.
The delivered placenta is carefully examined. Attention is paid not only to its integrity, but also to the number of membranes in the partition between the amniotic sacs.
In the postpartum period, with multiple pregnancies, late postpartum hemorrhage, subinvolution of the uterus, and postpartum purulent-inflammatory diseases often occur. Therefore, it is necessary to carry out timely prevention of these complications, in particular, monitor the contraction of the uterus after childbirth and, if necessary, prescribe uterotonics.
Forms
Depending on the number of fruits, we speak of twins, triplets, quadruples, etc.
There are two types of twins: fraternal (dizygotic) and identical (monozygotic). Children born from fraternal twins are called fraternal or not identical, and children from identical twins are called twins. Twins can be of the same or different sexes, while twins are only of the same sex.
Fraternal twins are the result of fertilization of two eggs, the maturation of which usually occurs during one menstrual cycle in one or both ovaries. The literature describes cases of so-called "superfetation" (the interval between fertilizations of two eggs is more than one menstrual cycle) and "superfecundation" (fertilization of eggs occurs during one ovulatory cycle, but as a result of different sexual acts). In dizygotic twins, each embryo/fetus develops its own placenta, and each of them is surrounded by its own amniotic and chorionic membranes. Thus, the interfetal septum consists of 4 layers. Such fraternal twins are called bichorionic biamniotic. The frequency of fraternal twins (among twins) is 70%.
In monozygotic twins, one egg is fertilized, and in this type of twins, the number of placentas formed depends on the time of division of the single fertilized egg. If division occurs within the first three days after fertilization, two embryos, two amniotic cells, and two chorions/placentas are formed. The interfetal septum, as in dizygotic twins, consists of 4 layers. Such monozygotic twins are also called bichorionic biamniotic.
When the division of the egg occurs in the interval of 3-8 days after fertilization, two embryos are formed, two amnios, but one chorion/placenta. The interfetal septum consists of two layers of amnion. This type of identical twins is called monochorionic biamniotic.
When the egg divides between 8 and 13 days after fertilization, one chorion and two embryos are formed, surrounded by a single amniotic membrane, i.e. there is no interfetal septum. Such identical twins are monochorionic monoamniotic.
The result of division of the fertilized egg at a later date (after the 13th day) is fused twins.
Thus, both fraternal and identical twins can be dichorionic, while only identical twins can be monochorionic. Examination of the placenta/placentas and interfetal membranes after the birth of the child does not always make it possible to accurately determine zygosity. In the presence of four interfetal membranes (which is possible with both monozygotic and dizygotic twins), only the different sexes of the children clearly indicate dizygosity. At the same time, the presence of two interfetal membranes clearly indicates monozygotic twins.
In the case of same-sex children, zygosity can be determined through additional blood testing (including HLA typing) or examination of skin biopsies from children.
Diagnostics multiple pregnancy
Before the introduction of ultrasound into clinical practice, the diagnosis of multiple pregnancies was not always simple; the diagnosis was often made in the late stages of pregnancy and even during childbirth.
Currently, the diagnosis of multiple pregnancy is based on the assessment of anamnesis data, the results of clinical, instrumental and laboratory research methods.
When collecting anamnesis, it often turns out that the pregnant woman or her husband is one of the twins. Information that the pregnancy occurred after ovulation stimulation or the use of assisted reproduction methods may indicate the possibility of multiple pregnancy.
In the first trimester, it is necessary to pay attention to the discrepancy between the size of the uterus and the gestational age - the growth of the uterus seems to be ahead of the gestational age. Particularly rapid growth of the uterus is observed in the second trimester of pregnancy.
In the late stages of pregnancy, the data of external obstetric examination are of certain importance for establishing the diagnosis: the abdominal circumference, the height of the fundus of the uterus are greater than they should be for a given period of pregnancy. Sometimes it is possible to palpate many small parts of the fetus and two or more large parts (heads and pelvic ends).
An auscultatory sign is the detection of foci of clear listening of fetal heart tones in different parts of the uterus. Different heart tones also indicate twins.
Biochemical tests play a certain role in diagnosing multiple pregnancy: the level of human chorionic gonadotropin and placental lactogen is higher than in singleton pregnancy. The level of alpha-fetoprotein may also be elevated.
The most accurate method for diagnosing multiple pregnancies is ultrasound. Ultrasound diagnostics of multiple pregnancies in the early stages is based on visualization of several fetal eggs in the uterine cavity, and from the 5th-6th week of pregnancy - two or more embryos.
In addition to early detection of multiple pregnancy, ultrasound in the II and III trimesters allows to establish the nature of development, position, presentation of fetuses, localization, structure, number of placentas and amniotic cavities, volume of amniotic fluid, presence of congenital malformations, condition of fetuses, nature of uteroplacental and fetoplacental blood circulation (UPC and FPC) using Doppler, determination of BPP. Difficulties arise in ultrasound diagnostics of a long-frozen fetus from twins ("paper fetus"), as well as in the presence of conjoined twins.
Diagnosis of the position and presentation of the fetus is especially important before childbirth to select the optimal method of delivery.
Possible options for the position and presentation of fetuses in twins:
- both fetuses are in a longitudinal position (most common):
- both in the head;
- both in the pelvic;
- one in the head, the other in the pelvic and vice versa;
- both fruits are in a transverse position;
- one fruit is in a longitudinal position, the other in a transverse position.
Conducting fetometry during ultrasound allows to detect intrauterine growth retardation of one or both fetuses. In addition, during ultrasound, Dopplerography is performed, which makes it possible to detect a violation of fetoplacental blood circulation, as well as placentometry, which determines the number and location of placentas, the structure of the placentas, the presence of a septum between the amniotic cavities. In the absence of visualization of the septum, one should assume monoamniotic twins, which are characterized by a high risk during labor. Ultrasound fetometry and placentometry allow to detect twin transfusion syndrome in the early stages.
Cardiac monitoring using a non-stress test is also of great importance for assessing the condition of the fetus.
How to examine?
Treatment multiple pregnancy
Early diagnosis of multiple pregnancy allows for the development of the most appropriate pregnancy management plan and timely prevention of possible complications.
Patients with twins require special attention throughout the pregnancy. It is very important to pay attention to the function of the cardiovascular system, kidneys, early symptoms of gestosis. If symptoms of gestosis or other complications of pregnancy appear, hospitalization in an obstetric hospital is necessary. In case of uncomplicated pregnancy, the patient should be sent to the maternity hospital 2-3 weeks before delivery, and in case of triplets - 4 weeks.
During pregnancy, it is important to monitor weight gain and take timely measures to prevent anemia.
A serious complication of multiple pregnancy is miscarriage. Multiple pregnancy itself is a risk factor for miscarriage. It dictates the need for treatment and preventive measures to prevent this pregnancy complication.
Due to significant overstretching of the uterus, the absence of a full contact belt due to the small size of the presenting part of the fetus in multiple pregnancies, there is a risk of premature rupture of amniotic fluid. To prevent this complication, a gentle regimen should be recommended and tocolytic agents should be prescribed.


 [
[