
All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Klebsiella in urine: norm, treatment
Medical expert of the article
Last reviewed: 04.07.2025
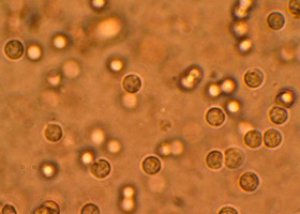
Klebsiella in urine, detected during laboratory tests, does not bode well, since the gram-negative enterobacteria Klebsiella spp., being an opportunistic microorganism, can cause many serious diseases.
Although this bacterium is present in small quantities in the human microbiota, it is one of the most common nosocomial infections that can “join” during hospital treatment, colonizing the lungs, urinary and gall bladder, liver, kidneys, and intestines. And Klebsiella, as is expected of all opportunistic infections, most actively demonstrates its pathogenicity in weakened immunity and severe conditions, as well as in elderly patients and infants.
According to clinical studies, the main types of Klebsiella – Klebsiella pneumoniae and Klebsiella oxytoca – are largely responsible for cases of severe inflammation of the urinary tract, secondary infection of postoperative wounds, nosocomial pneumonia, bacteremia, septicemia, and sepsis.
Since Klebsiella spp. is highly resistant to many classes of antimicrobial agents, doctors' prescription of a urine test for Klebsiella is a clear sign that the antibiotics used are not effective.
Klebsiella norm in urine
Urine tests conducted during a medical examination are in most cases required to establish or clarify a diagnosis in the presence of a pathological condition. The results obtained are supposed to be compared with the average standard values for healthy people. So, since the exact infectious dose of Klebsiella spp. is currently unknown, the very conditional norm of Klebsiella in urine, which is adhered to in clinical diagnostics, should not be higher than the indicator - 102-105 CFU in one milliliter of urine.
CFU is a colony forming unit that microbiologists use to quantify the results (bacteria count) of a bacteriological examination of urine sediment.
The definition of urinary tract infection at the level of significant bacteriuria is based on the presence of Klebsiella in the urine (mainly Klebsiella pneumoniae and Klebsiella oxytoca species) – in quantities greater than 100,000 colony-forming units per milliliter, i.e. greater than 10 5 (105) CFU/mL of urine. This value was chosen because of its high specificity for diagnosing true infection even in the absence of symptoms. However, several studies have found that more than 50% of women with bladder inflammation have lower CFU counts.
In men, the minimum level of Klebsiella in urine indicating urinary infection is 103 CFU/ml, and in the case of long-term use of a catheter – no higher than 102 CFU/ml.
Klebsiella pneumoniae in urine
In laboratory studies, K. pneumoniae can be isolated from blood, pleural fluid, wound exudates, and also from nasopharyngeal tests (nasopharyngeal swabs).
But Klebsiella pneumoniae is more often found in urine. And if the body is weakened due to illness or decreased immunity and has become more susceptible to pathogens, then there is a real threat of developing:
- - acute uncomplicated cystitis;
- - recurrent cystitis (in young women with a K. pneumoniae count of 100 CFU/ml);
- - complicated urinary tract infection (UTI), Klebsiella in urine at a level of 103 CFU/ml and higher;
- - acute cystitis in young men (102-103 CFU/ml);
- - acute pyelonephritis (105 CFU/ml or more).
Klebsiella oxytoca in urine
Klebsiella oxytoca – Klebsiella oxytoca may also be present in urine, but it is almost never isolated separately.
Colonies of this species of Klebsiella spp. can be found almost anywhere, but Klebsiella oxytoca prefers to colonize the surface of the skin, the mucous membrane of the nasopharynx and the colon.
Although this bacterium causes fewer pathologies than Klebsiella pneumoniae, it accounts for up to 8% of all bacterial infections in Europe and North America.
Klebsiella planticola in urine
Klebsiella planticola is not detected in urine or other clinical materials for diagnostic purposes.
Initially, K. planticola, described in 1981, was found exclusively in aquatic, botanical and soil environments. In 1983, the bacterium was described as Klebsiella trevisanii, and in 2001 as Raoultella planticola. And so far, nothing is known about the expression of its virulence factors, nor about its ability to colonize human tissues and organs.
However, one recent study identified K. planticola in throat and rectal swabs from neonates, according to a report in the Journal of Clinical Microbiology. Given that the endogenous microflora is thought to be the primary source of neonatal Klebsiella infections, further study of this bacterium is clearly warranted.
Klebsiella in urine in adults
Along with bacteremia, Klebsiella in the urine of adults in quantities exceeding the analysis value of 100-105 CFU/ml causes infectious lesions of the urinary system and urinary tract.
In men, Klebsiella levels in urine that rise to more than 1000 CFU/ml are indicative of a urinary tract infection, with a sensitivity and specificity of 97%.
Klebsiella is second only to Escherichia coli as a cause of urinary tract infection in older adults.
Clinical symptoms that appear when the bladder is affected in the form of acute cystitis and pyelonephritis include:
- dysuria with increased frequency of urination;
- imperative urge to urinate with a small amount of urine excreted;
- a burning sensation when urinating and sharp pains in the perineum and lower abdomen;
- dull and aching pain in the lumbar region;
- urination with blood (hematuria);
- the appearance of purulent impurities in the urine (pyuria).
Systemic symptoms such as fever and chills usually indicate concomitant pyelonephritis or prostatitis.
Klebsiella in urine during pregnancy with a colonization level of more than 105 CFU/ml causes the same symptoms. And with an indicator of more than 103 CFU/ml, asymptomatic bacteriuria is observed.
Klebsiella in urine of a child
According to statistics from foreign clinical microbiologists, the most common causes of urinary tract infections among children are Escherichia coli (more than 62%), and Klebsiella is in second place (23%). Then come Proteus mirabilis (7%), Citrobacter (5.4%), Staphylococcus saprophyticus (1.3%) and Candida albicans (0.4%). Moreover, E. coli is the most common cause of UTI among children of all ages, and in case of urinary system pathologies in newborns, Klebsiella is detected in the child's urine in 42.8% of cases.
It is also noted that in children under three months of age with a temperature above +38°C – in the absence of an obvious source of infection – it is mandatory to take a urine test for Klebsiella planticola. And take into account the indicator of the presence of this bacterium of 50,000 CFU/ml, although strict definitions of colony counting criteria are operational, not absolute.
What tests are needed?
Who to contact?
Treatment Klebsiella in the urine
Treatment of urinary tract infections caused by Klebsiella spp. is carried out using antibiotics. And the choice of drug for a specific patient, the method of administration and dosage - taking into account contraindications - remains with the doctor.
Adults and children are treated against Klebsiella with: Augmentin, Levofloxacin, Amoxicillin + Clavulanic acid, Amikacin, Ciprofloxacin, Cefuroxime, Nitrofurantoin monohydrate, Doxycycline monohydrate, Fosfomycin.
Symptomatic urinary tract infections complicate 1-2% of pregnancies, usually in women with persistent bacteriuria. In case of pyelonephritis, most pregnant women should be treated with antibiotics. Tetracyclines and fluoroquinolones should be avoided during pregnancy. And what antibiotics can be used, read more - Cephalosporins during pregnancy

